Radiotherapy is planned taking into account the following factors. Firstly, this is the main diagnosis, i.e. localization of the malignant tumor and the extent of its spread to surrounding tissues and distant organs. Secondly, this is the degree of malignancy, the presence of lymphovascular invasion and other prognostic and predictive factors, which are determined by morphological, immunohistochemical and molecular genetic studies. Thirdly, the presence of previous treatment and its effectiveness. And fourthly, this is, of course, the general condition of the patient, age, the presence and degree of correction of concomitant pathology and the patient’s life expectancy.
The effect of radiation therapy is based on ionizing irradiation of a certain area with a flow of particles that can damage the genetic apparatus (DNA) of the cell. This is especially pronounced in actively dividing cells, since they are most susceptible to damaging factors. The functions and vital activity of cancer cells are disrupted, which in turn stops their development, growth and division. Thus, as a result of radiotherapy, the malignant tumor decreases in size until it disappears completely. Unfortunately, healthy cells that are located on the periphery of the tumor can also enter the irradiation zone in different volumes (depending on the type of radiotherapy used), which subsequently affects the degree of their damage and the development of side effects. After treatment or in between irradiation sessions, healthy cells are able to repair their radiation damage, unlike tumor cells.
Treating cancer with tightly focused beams (such as stereotactic radiation therapy) helps avoid these unwanted effects. This technique is available at the radiation therapy center of the OncoStop project. Stereotactic radiotherapy is generally well tolerated by patients. However, when prescribing it, it is necessary to follow some lifestyle recommendations, as they can reduce the risk of side effects and improve the quality of life.
Types of radiation therapy
There are several classifications of radiation therapy. Depending on when radiotherapy is prescribed, it is divided into: neoadjuvant (before surgery), adjuvant (after surgery) and intraoperative. The goals of neoadjuvant irradiation are to reduce tumor size, achieve an operable state, and reduce the risk of metastasis through the vessels of the circulatory and lymphatic system to lymph nodes and distant organs (for example, in breast cancer, rectal cancer). Adjuvant radiation is aimed at minimizing the risk of local tumor recurrence (eg, breast cancer, malignant brain tumor, bone tumor). In each specific case, the advisability of prescribing radiotherapy is determined individually.
When choosing a method for delivering a radiation dose, the radiotherapist first evaluates the location of the tumor, its size, and the proximity of blood vessels, nerves, and critical organs. In this regard, there are 3 ways to administer the dose :
- External beam radiation therapy uses an external radiation source (for example, a linear accelerator) that directs radiation beams to the tumor.
Contact (brachytherapy) - radioactive sources (for example, radioactive grains) are placed inside (for prostate cancer) or near the tumor.
Let's look at each of these types of radiotherapy in more detail.
When did radiation therapy appear?
In 1896 in Vienna, Dr. Freund was the first in the world to use x-rays not to diagnose a disease, but to treat a superficially located benign formation. A few years later, the spouses Pierre and Marie Curie discovered radioactive radium, which began to be used for contact radionuclide therapy.
Over the past 125 years, radiation therapy has undergone a long journey of improvement, has become widely used and has reached a qualitatively new level. According to the expert community, currently at least 60-70% of all cancer patients require radiation therapy.
What will you get from radiation therapy at the Rassvet Clinic?
Oncologists at the Rassvet Clinic are highly qualified specialists and regularly undergo international training and internships.
Rassvet is a multidisciplinary expert clinic. We provide support from related specialists at all stages of specific antitumor treatment, and also provide the full range of necessary supportive therapy. We pay great attention to the comfort of our patients and make every effort to minimize psycho-emotional stress during treatment and rehabilitation.
The Rassvet Clinic works with reliable and trusted radiation therapy centers, and their doctors and radiation therapists are part of our multidisciplinary team for the treatment of oncological diseases.
Goals of radiotherapy
The goal of radiation therapy is to achieve the maximum possible effect on the tumor and areas of its clinical and subclinical spread with a high degree of accuracy and minimal consequences for surrounding tissues and organs. The goal of radiation therapy is the destruction of the tumor mass, ideally leading to its elimination or reduction in size and metastatic potential, slowing growth, which helps prolong life and improve its quality.
Radiation therapy can be used at different stages of treatment:
- Preoperative (so-called induction, or neoadjuvant)
- Intraoperative – during surgery
- Postoperative (adjuvant)
- Independent (definitive)
Preoperative radiotherapy
The goal of preoperative radiation therapy is to minimize the tumor volume, prevent tumor cells from entering the lymphatic or circulatory system, and reduce the risk of developing distant metastases. For most types of tumors, a tandem of radiation and chemotherapy is most often used. This combined effect allows further radical intervention with complete removal of the tumor. In some cases, preoperative radiation/chemoradiotherapy can lead to complete regression of the tumor, thus becoming an independent treatment method. Achieving complete clinical regression, proven by radiological methods (CT, MRI, PET-CT) and supported by biopsy data, increases the possibility of delaying or refusing surgery. Thus, for rectal tumors with a complete clinical response to chemoradiotherapy, the “waitandsee” concept has gained recognition, i.e. “wait and watch”, enshrined in international and national treatment standards.
Intraoperative radiotherapy
Intraoperative radiation therapy is the irradiation of the tumor bed immediately after its surgical removal, directly in the surgical field. This is an effective method of reducing the risk of local relapse. Intraoperative radiation therapy is used for breast tumors, soft tissue sarcomas, and even gastrointestinal tumors. This method is very effective, but is not without its drawbacks. Firstly, it requires special mobile and compact radiation units, which can be located in the operating room. Secondly, a single dose of radiation may be insufficient, and the volume of intraoperatively irradiated tissue is quite limited. Intraoperative radiation therapy does not allow the lymphatic flow to be affected. It is difficult to ensure the accuracy of dosimetric planning. The radiation procedure increases the time the patient remains under anesthesia and the overall duration of the intervention. Therefore, intraoperative radiation therapy is often an integral part of combined irradiation, a stage of complex treatment.
Postoperative radiotherapy
Postoperative radiation therapy is the effect on the area of the removed tumor and lymphatic drainage pathways in order to prevent the possibility of the spread of individual tumor cells during surgery, i.e. reducing the risk of developing local and distant metastases. Postoperative radiation therapy is necessary both after major operations and after minimally invasive interventions. Currently, it is most often used in the treatment of breast cancer, soft tissue sarcomas, and head and neck tumors.
Side effects and consequences
Radioactive rays, to one degree or another, affect not only the tumor, but also normal tissues located next to the malignant tumor or located between it and the source of radiation. However, short-term dosed radiation does not cause irreversible processes in healthy cells: they are able to recover from damage caused by radiation. Modern technologies of radiation exposure minimize the likelihood and severity of complications, however, side effects from radiation therapy can be observed both immediately after irradiation and over long periods of time.
Most often, immediately after the procedure, transient side effects are observed, such as general weakness and redness of the skin at the site of irradiation, and less often - swelling. The nature and severity of other possible complications and side effects are related to the location of the tumor.
With the correct regimen, nutrition and timely medical correction, the side effects of RT do not affect the patient’s quality of life.
Restoration and elimination of the consequences of radiation therapy
Full recovery after radiation therapy takes from 2 weeks to 2-3 months, and sometimes more. In general, after modern radiosurgery treatment, the patient can return to daily activities the very next day. The main task during rehabilitation is to remove toxins from the body formed during the breakdown of cancer cells. Also, if there were side effects during therapy, their consequences are eliminated during rehabilitation. The general period of rehabilitation, as well as recommendations for the regimen, nutrition and taking medications during the rehabilitation period depend on the diagnosis and general health of the patient, the individual characteristics of his body and the treatment performed.
Independent or definitive radiotherapy
Independent radiation/chemoradiation therapy is indicated in cases where its effectiveness is comparable to radical surgical treatment, i.e. for early cancer, or, on the contrary, when radical intervention is impossible - in the presence of general contraindications or due to the spread of the tumor. Currently, it is considered as an alternative treatment method for early tumors of the vocal larynx and a number of skin tumors. It is most widely used in the treatment of prostate cancer. In combination with chemotherapy, it is successfully used for early tumors of the esophagus and anal canal. Chemoradiation treatment is the leading treatment for cervical cancer.
Finally, radiation therapy is used to eliminate symptoms of a tumor disease, such as pain, difficulty swallowing, etc. (symptomatic radiation therapy) or to contain the tumor process (palliative radiation therapy).
Chemoradiation therapy
Radiation therapy is rarely performed as a stand-alone treatment. Most often it is combined with some other type of treatment: surgical, and most often with medication. This can be either the option of simultaneous or sequential chemoradiotherapy, as well as options for combining radiation therapy with immunotherapy, targeted and hormonal therapy. Such types of treatment may have significantly higher antitumor efficacy, however, the risks of joint side effects must be carefully assessed, so decisions on any volume of treatment for oncological pathology should be made by a multidisciplinary oncological council.
Book a consultation 24 hours a day
+7+7+78
Radiotherapy technology
The sequence of treatment measures for each patient is decided on by an oncological council consisting of an oncological surgeon, a chemotherapist and a radiotherapist. Having determined the indications for radiation treatment, the radiotherapist formulates a general treatment plan: course duration, dose fractionation regimen (dose per one radiation session), total radiation dose, the need for simultaneous chemoradiation treatment, and the use of radiomodifiers. Irradiation sessions are preceded by a pre-radiation preparation stage.
Pre-radiation preparation includes:
- Computer (X-ray) topometry
- Contouring of the target and adjacent organs
- Dosimetric planning
Computer topometry
The creation of an individual dosimetric radiation map begins with computer topometry, which is carried out by a radiologist together with a radiotherapist. On a computed tomography simulator, with the same fixing devices and in the same position in which the treatment will be carried out, the area of the anatomical location of the tumor is scanned (chest, abdominal cavity, brain, etc.). Structural and anatomical features are assessed - tumor localization, volume extent, relationship with adjacent organs, density of internal tissues. During this procedure, graphic landmarks are placed on the patient’s skin—marks for centering the radiation beams, which will further speed up navigation during treatment sessions. A sequence of computer scans is transmitted to a planning station to create an individual radiation plan.
Contouring of the target and adjacent organs
Next comes the stage of processing the resulting images. The scans are imported into the planning system, where the radiotherapist, with the help of a radiologist, outlines the tumor target and all adjacent organs in each scan received. Based on a set of volumetric images, dose loads during treatment on the tumor and neighboring organs are subsequently calculated, taking into account their tolerance to radiation.
Dosimetric planning
After completing the delineation, assessing the location of the tumor and adjacent organs, the stage of dosimetric planning of the course of radiation treatment begins, which is performed by medical physicists. Dosimetric planning is the selection of the number and conditions for the formation of radiation beams, their spatial placement in order to deliver the maximum possible therapeutic dose to the tumor with minimal consequences for neighboring organs. Modern medical accelerators with multi-leaf collimators make it possible to form fields of complex configurations that most accurately match the volume and shape of the irradiated target, producing the so-called. conformal irradiation. Based on the objectives, optimal target coverage can be planned using 3D multifield intensity modulated radiation (IMRT) or intensity modulated arc radiation (VMAT).
The image shows an example of 3D multifield radiation. It can be seen that 3 beams are used to irradiate the tumor.
Make an appointment
Sign up for onco by number. Consultation with an oncologist takes place by calling in advance. The cost is presented on our website. In our clinic you can take any tests, undergo the necessary examinations with a detailed interpretation of the results and the prescription of effective treatment. We use the most effective methods according to international standards.
Our specialists have many years of experience in the medical practice of treating oncology. We work not only on weekdays, but also on holidays and weekends. The clinic is located in Moscow, in the Central Administrative District (CAO), near the Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya, and Chekhovskaya metro stations.
Patient immobilization means
In order to accurately deliver ionizing radiation to the irradiated target, it is necessary to clearly reproduce the position in which the process of preparation for radiation treatment took place, i.e. computer topometry and dosimetric planning. This is provided by a variety of means for positioning and immobilizing the patient. They can be in the form of different standard decks with headrests, fastenings, bolsters and supports for arms, legs, and pelvis. There are also individual means. For example, vacuum mattresses and thermoplastic masks that fix the individual shape of the patient’s body in the irradiation position. These devices make it possible to avoid displacement of the irradiated area due to involuntary movements of the patient.
Types of radiation therapy
External beam radiotherapy
With remote irradiation, the source of ionizing radiation is located at a distance - outside the patient’s body and outside the tumor target. Depending on the type of radiation device, external beam radiation therapy includes x-ray therapy, telegammatherapy, electron and proton therapy. The most common option for external beam radiation therapy today is irradiation with high-energy photons and electron beams at medical electron accelerators. Modern models of accelerators, using computer control of the parameters and geometry of the radiation beam, ensure maximum compliance with the shape of the target source and the distribution of the radiation dose in it. The ability to form beams of bremsstrahlung (photon) and corpuscular (electronic) radiation with varying powers - from 6 MeV to 18-20 MeV - makes it possible to irradiate both surface and deep-lying objects in the body tissues.
Particular attention is currently focused on proton therapy. Russia's first clinical proton therapy center was built in St. Petersburg. The advantage of the method is the peculiarity of heavy charged particles (protons). Protons release their braking energy as much as possible at the end of their travel path, and the dose decrease from 90% to 20% occurs at a distance of 2-5 mm. This possibility of concentrating the dose at the end of the particle path allows not only to best concentrate the dose, but also to minimize the radiation load on the tissue along the beam and behind the pathological focus. Proton therapy is relevant in onco-ophthalmology, radioneurosurgery, and especially for pediatric patients. Currently, the scope of proton therapy is expanding, but so far the use of the method is significantly limited by its high cost.
Modern technology of external irradiation is stereotactic radiation therapy - a method of high-precision large-fraction irradiation of tumors no larger than 5 cm in size. Unlike radiosurgery, developed for the treatment of brain tumors, which uses a single irradiation, the total number of fractions with stereotactic irradiation varies from 1 to 5-6. A single focal dose ranges from 8 Gy to 20 Gy, the total equivalent absorbed dose from 50 Gy to 150 Gy, which is significantly higher than with the classic version of fractionation of radiation therapy. Gamma knife is one of the types of radiation installations for stereotactic irradiation of brain tumors. Accelerators with microleaf collimators allow stereotactic irradiation of any lesion (brain, prostate, lung, bones, liver, pancreas, lymph nodes, soft tissues). During stereotactic irradiation, displacements of the focus that occur during breathing must be taken into account. For this purpose, CT images are recorded during CT simulation with synchronization of the respiratory cycle (4D radiation therapy).
Taking a course of radiotherapy
The course of cancer treatment using radioactive radiation includes several successive stages.
Preliminary preparation
- The tumor is scanned using CT, MRI or PET diagnostics.
- Based on the images obtained and the results of other clinical studies, the optimal method (or a combination of several methods) is determined.
- Planning is carried out to determine treatment tactics, number of sessions (fractions), dose and time of irradiation. Planning is one of the most important stages of radiation therapy in oncology. Properly planned radiotherapeutic treatment ensures maximum intensity of the destructive effect of radiation on the cancer tumor and minimal stress on healthy tissue. The planning of radiation treatment for cancer involves the attending physician and specialized specialists: radiation oncologist, radiation physicist and dosimetrist.
Carrying out the procedure
- A nurse with the appropriate specialization participates in preparing the patient for a radiotherapy session.
- The patient is placed on a medical table; various devices can be used to support his body in a given position.
- The procedure is short, painless and in the vast majority of cases does not cause any unusual sensations.
- If a course of radiation therapy includes several fractions, adjustments may be made to the plan as necessary.
Nutritional Features
The diet during the preparatory period, during the course of treatment and after its completion is determined by the location of the cancer tumor and radiation exposure.
It is most important to adhere to a diet if the esophagus, abdomen and pelvis area is exposed to radiation. General recommendations include drinking enough fluids and limiting fatty, dairy, and fiber-rich foods in your diet. You should eat food often, in small portions.
Contact radiotherapy
With contact radiation therapy or brachytherapy, a radiation source is introduced into the affected organ. The advantages of this type of therapy are a short course, high accuracy and low load on adjacent organs, which is very important for the future quality of life of patients. For brachytherapy, various radioactive sources are used - isotopes of cobalt (Co⁶⁰), iridium (Ir¹⁹²), cesium (Cs¹³⁶).
Contact radiation therapy has different types: application, intracavitary, interstitial and radionuclide radiation therapy.
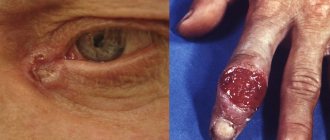
Application radiotherapy
In application radiation therapy, the source is located on the surface of the external object being irradiated (skin).
Intracavitary radiotherapy
In intracavitary radiation therapy, the source is brought directly to the tumor in the organ cavity. It is most often used for cancer of the rectum, anal canal, esophagus, and intrabronchial formations. Intracavitary or intraluminal brachytherapy is more often used as a stage of combined radiation therapy, before or after external beam irradiation. However, brachytherapy as an independent method is often sufficient after minimally invasive surgery in the early stages of cancer. In the palliative treatment of esophageal cancer, brachytherapy is an effective way to eliminate dysphagia (swallowing disorder).
Interstitial radiotherapy
In interstitial radiation therapy, the source is injected into the tissue of the tumor itself. Interstitial brachytherapy is most common for prostate tumors and is widely used for breast radiation, head and neck tumors, and liver tumors.
Radionuclide radiotherapy
In radionuclide or radioisotope therapy, the source of radiation is a radiopharmaceutical, which, after being introduced into the patient’s body, selectively accumulates in tumor tissues. The most widely used radiopharmaceuticals are radionuclides containing iodine I¹³¹ (thyroid cancer), I¹²⁵ (in the form of granules for the treatment of prostate cancer), strontium Sr⁸⁹ (bone metastases). Disadvantages limiting the use of radionuclide therapy are a narrow therapeutic range, limited possibility of precise dosimetric planning, and the inapplicability of multifraction irradiation. Considering the number of absolute restrictions, the cost of the method is quite high.
Publications in the media
A significant proportion of cancer patients require radiation therapy at some stage of treatment. Radiation therapy can be used as an independent or combined method, as well as in combination with chemotherapy drugs. Depending on the stage of the tumor process, the radiosensitivity of the tumor, and the general condition of the patient, it can be radical or palliative. Radiation therapy is prescribed only with morphological verification of the diagnosis.
Modern methods of radiation therapy are varied, both in the types of radiation used and in the method of delivering its energy to the tumor. Currently, various electromagnetic radiations (X-ray and bremsstrahlung of high energies, g- and b-rays of radioactive substances) and corpuscular radiation (electrons, protons, neutrons, negative p-mesons, multiply charged ions, etc.) are used. Based on the method of application, remote and contact irradiation methods are distinguished.
• With remote irradiation , the source is located at a distance from the patient, the radiation beam is given the required shape and directed to the required part of the body (organ).
• The contact method is used in three variants: •• application - placing the radiation source on the surface of the body in special applicators; •• intracavitary - the radiation source is introduced into the body cavity (oral cavity, uterus, vagina, etc.); •• interstitial - the introduction of radioactive substances (drugs) directly into the tumor tissue, or the introduction of special drugs into the body with their subsequent absorption by the tumor tissue (for example, I131 for thyroid cancer).
The main goal of radiation therapy is to provide maximum radiation exposure to tumor cells with minimal damage to healthy tissue. It is believed that radiation-induced cell death is associated primarily with damage to DNA, the membrane complex, and gross disturbances in the properties of proteins, cytoplasm, and enzymes. All human tissues (with varying sensitivity) are susceptible to ionizing radiation. The most sensitive to radiation are hematopoietic tissue, intestines, and gonads. Less sensitive are fibrous tissue, parenchyma of internal organs, cartilage, bone, nervous tissue, and muscles. The histological structure of the tumor is an indicative sign for predicting radiosensitivity. One of the ways to increase the effectiveness of radiation treatment of tumors is to control the radiosensitivity of the tumor and normal tissues. The difference in radiosensitivity between tumors and normal tissues is called the radiotherapeutic interval.
Several methods are used to increase the radiotherapeutic interval. • Changing the dose, rhythm and time of irradiation. They use both an increase in single doses with a decrease in their number, and a decrease in a single dose with shortened intervals between fractions, as well as a dynamic fractionation regime, split courses of radiation, which lead to better patient tolerance of the entire course of treatment, and also involve reoxygenation of the tumor during the break. • Using the radiomodifying effect of oxygen by increasing the radiosensitivity of the tumor by its oxygenation and reducing the radiosensitivity of normal tissues by creating short-term hypoxia in them. • Radiosensitization of the tumor with the help of certain chemical agents , chemotherapy drugs. • Local tumor hyperthermia , which affects many mechanisms of biochemical processes in the tumor cell and causes disruption of post-radiation recovery processes. • Creation of artificial hyperglycemia , which causes a decrease in pH in the tumor tissue, which makes it selectively vulnerable to the effects of ionizing radiation.
Type of radiation therapy • Radical (radical program) radiation therapy consists of therapeutic radiation exposure to the area of clinical spread of the tumor and, if necessary, prophylactic irradiation of areas of possible subclinical metastasis. The goal of complete damage to tumor tissue is most often achievable in the early stages of the disease, with small tumors with high radiosensitivity. Radiation therapy (either alone or in combination with chemotherapy) can be radical for some cancers (for example, Hodgken's disease, some head and neck tumors, cancer of the skin, lower lip, cervix) •
Palliative radiation therapy is indicated when radical removal of the tumor or metastases is impossible, the patient refuses surgical treatment, or there are contraindications to it. The main goal of palliative radiation therapy is to minimize the biological activity of the tumor, reduce the size of the tumor, or inhibit its growth. At the same time, clinical symptoms, compression of vital organs/tissues, inflammatory reactions, etc. are reduced.
Therapeutic combinations . Radiation therapy can be used alone or in combination with chemotherapy or surgery • Chemotherapy can be used together with or before radiation treatment to increase the effectiveness of the latter •• For example, pyrimidine acts as a radiation sensitizer during radiation therapy •• Combination therapy can cause severe toxic reactions. A classic example is the effect of return of the radiation reaction - the development of an enhanced (or reactive) local reaction in a previously irradiated area with the simultaneous administration of doxorubicin and/or methotrexate • In combination with the surgical method, radiation therapy is used both in the pre- and postoperative period •• Preoperative irradiation has several goals: maximum damage to the most sensitive proliferating tumor cells and a decrease in the biological activity of others; reducing the likelihood of dissemination of cancer cells during surgical procedures, preventing relapses and metastases by reducing the possibility of intravascular dissemination of tumor elements and devitalization of micrometastases (so-called radiation ablastics), reducing tumor volume. Preoperative irradiation may slightly increase the risk of postoperative complications (epithelitis, pneumonitis, poor wound healing, fistula formation, etc.). In these cases, the interval between the end of irradiation and the operation should be sufficient to maximize the effect of therapy and not coincide with the time of the height of radiation reactions, creating optimal conditions for wound healing.
Contraindications to radiation therapy: anemia, leukopenia, thrombocytopenia, cachexia, intercurrent diseases accompanied by a febrile state, active forms of tuberculosis, during chest irradiation - cardiovascular diseases and respiratory failure, inflammatory diseases of the lungs, kidney diseases, central nervous system, signs of tumor tissue disintegration .
Complications • Radiation reactions and damage •• Reactions - acute local effects (mainly swelling and inflammation) are observed within days or weeks of radiation •• Damage may appear for several months or even years after radiation therapy. Radiation damage includes persistent organic changes in organs and tissues adjacent to the tumor and exposed to radiation. Radiation damage can be of the nature of atrophic or hypertrophic dermatitis, indurative edema, fibrosis, radiation ulcer, rectitis, cystitis, pneumosclerosis, pericarditis, etc. Radiation complications require long-term special treatment. • The severity of adverse reactions depends on the location, size of the irradiated field, type of source, and dose pattern (eg, total dose, single session dose, dose rate). Local effects can be reduced by: •• accurately defining the tumor field using radiological techniques (eg, CT and MRI) •• avoiding the direct effect of radiation on vital organs (eg, spinal cord) •• protecting normal tissue from radiation •• reducing area of the irradiated field during the treatment course (boosting). • General effects on the body : malaise, fatigue, anorexia, suppression of hematopoiesis; general symptoms are especially characteristic of patients receiving concurrent chemotherapy and radiation treatment. • Skin reactions have been observed following high-dose radiation to areas of the skin (eg, chest after mastectomy) or female genitalia (eg, vulva).
Repeated irradiation or incorrect use of the joining fields method (with the superposition of one irradiation field on another) can cause multiple reactions •• Acute reactions are manifested by erythema, dry desquamation with itching, as well as wet desquamation of the epithelium ••
The damaged area should be clean and dry. Additional treatment includes: ••• local application of ointments with vitamins A and D, liquid oil for children ••• cleansing the affected area with hydrogen peroxide solution and 0.9% sodium chloride solution (1:1 ratio) •• • topical application of HA •• Patients should not wear clothing that irritates the damaged area; It is also necessary to avoid exposure to direct sunlight.
• Irradiation of the head or neck with high doses causes reactions from the oral cavity and pharynx - inflammation of the mucous membrane, pain, anorexia, dry mouth, dental caries •• To reduce such reactions, strict adherence to oral hygiene, local use of anesthetics, drugs that regulate salivation, proper nutrition •• In severe cases, it may be necessary to provide nutrition through a gastric tube or gastrostomy tube.
• Gastrointestinal reactions are observed with doses above 40–55 Gy •• Esophagitis usually resolves by 7–10 days; patients are predisposed to candidal lesions. Treatment: antacids, liquid foods and local anesthetics •• Radiation gastritis and enteritis may present with nausea, vomiting, diarrhea, abdominal pain, loss of appetite, bleeding. Treatment: ••• antiemetics (eg, prochlorperazine, trimethobenzamide) ••• antidiarrheals ••• liquid, easy-to-digest, low-fat foods ••• dietary supplements •• Bleeding and/or pain accompany rectal inflammation. The patient's condition is alleviated by an appropriate diet and enemas with HA.
• Radiation pneumonitis with cough, shortness of breath, and chest pain usually develops after irradiation of a significant volume of the lung. The condition is controlled by prescribing prednisolone 4 times a day, 15 mg (should be discontinued gradually to prevent withdrawal syndrome).
• CNS lesions can be observed both during the course of therapy and long after treatment •• Acute symptoms accompanying irradiation of the head: dull, prolonged headache, signs of increased ICP, nausea and vomiting. When prescribing dexamethasone (4 mg 4 times / day) - rapid disappearance of symptoms •• Delayed symptoms: violations of short-term (working) memory, pathology of the white matter of the brain, dilatation of the ventricles and the appearance of foci of calcification •• Drowsiness syndrome (hypersomnia and fatigue) is observed during many weeks and months after irradiation of the skull (especially in patients who received injections of chemotherapy drugs under the membranes of the brain).
• Suppression of bone marrow hematopoiesis occurs during irradiation using the wide-field method used in the treatment of lymphogranulomatosis (Hodgken's disease) and neoplasms in the pelvic area; especially pronounced in patients simultaneously receiving chemotherapy. For leukopenia or thrombocytopenia, blood transfusion therapy is often necessary. The development of anemia is rarely observed. When the Hb level decreases below 80 g%, blood transfusion is indicated.
ICD-10 • Y84.2 Radiological procedure and radiation therapy