December 21, 2020
Trigeminal neuralgia (facial or trigeminal neuralgia) is a disease of the peripheral nervous system characterized by short-term, intense and repeated pain in the area of innervation of one or more branches of the nerve.
Trigeminal neuralgia (facial or trigeminal neuralgia) is a disease of the peripheral nervous system characterized by short-term, intense and repeated pain in the area of innervation of one or more branches of the nerve. The nerve received its name due to the presence of three branches in it: ophthalmic (upper), maxillary (middle), mandibular (lower).
It is extremely difficult to independently diagnose pathology due to the nonspecific symptoms inherent in many diseases (for example, dental ones). That is why, if any unpleasant sensations occur in the facial area, it is necessary to promptly contact a neurologist. Trigeminal neuralgia most often affects adults, especially the elderly, and is more common in women.
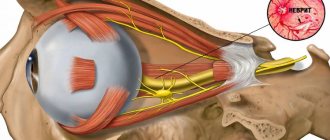
The pathogenesis is not completely clear. It is currently believed that the disease occurs as a result of compression of the trigeminal nerve (at the site of its exit from the pons) by tortuous, pathologically altered vessels or, less commonly, by a tumor. As a result of compression, the nerve root adjacent to the cerebral pons undergoes demyelination. This reason explains up to 80-90% of cases of the disease. Rarely, patients with multiple sclerosis develop a plaque in the area of the sensory nucleus of the trigeminal nerve, which leads to neuralgia.
The factors that most often provoke the development of the disease include: pinching of the trigeminal nerve (temporomandibular joint injuries, congenital anomalies in the development of bone structures of the skull, tumors of the brain and facial area, pathological vasodilatation, etc.); viral nerve damage (herpetic infection, polio); odontogenic infections (“unsuccessful” filling or extraction of teeth or other surgical interventions in the face and oral cavity, reaction to anesthesia of dental canals, dental flux).
Trigeminal and facial neuralgia
Neuralgia is a disease in which damage or compression of the trigeminal nerve and/or its branches occurs. This causes a sharp piercing pain that occurs suddenly and brings physical and psychological discomfort to the patient. Despite the fact that the term “neuralgia” can be literally translated as “nerve pain,” the matter is not limited to pain. Trigeminal and facial neuralgia are radically different in symptoms. The facial nerve contains mostly motor fibers, so neuralgia leads to dysfunction of the facial muscles (the degree depends on the severity of the disease), and can also cause lacrimation, dry eyes and partial loss of taste. Pain in facial neuralgia is usually concentrated in the area of the parotid gland (the patient complains that the pain radiates to the ear), but there may be no pain at all. It is because of the lack of pain that some experts use the term “neuropathy” when talking about damage to the facial nerve. With the trigeminal nerve it’s exactly the opposite, since it contains many sensory fibers.
Diagnosis of neuralgia
Diagnosis of neuralgia in the CELT Clinic does not cause difficulties, since it has a number of pronounced signs. When talking about the clinical manifestations of the disease, patients try not to touch the affected side of the face and remain in a tense state because they expect a new attack.
Studies are carried out on the functions of the facial and trigeminal nerves, which begin with assessing the symmetry of the patient’s face. In addition, a number of tests are carried out to check taste and sensitivity.
For the most accurate diagnosis of pathological processes in the nerves of the face, an ultrasound scan of the nerves is performed.
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Symptoms
The first attack of pain can be triggered by elementary things that no person can do without: laughter, smiling, articulation, brushing teeth, eating, frostbite on the face. Pain appears in one half of the face. At first, the painful attacks are short-lived. They end, just as they begin, abruptly. Over time, pain occurs more frequently and lasts longer. Often the pain begins to originate in the jaw and can be confused with toothache. Then the painful sensations move to the area of the cheek, ear, and forehead. There is lacrimation, paresis of the facial muscle, and the face becomes asymmetrical. After the attack, a period of remission occurs, which lasts several minutes. During remission there is no pain.
Causes
Unlike neuritis, neuralgia is not an inflammatory disease. Fever, fever, swelling and other symptoms of the inflammatory process are not associated with this disease. However, if the trigeminal nerve is damaged due to neuritis, pain sensations that fit the description of neuralgia may well occur. To avoid confusion and differentiate the two pathologies, it is necessary to consider their etiology.
The cause of neuritis (like any other inflammatory disease) is viruses and infections that cause gradual destruction of the membrane and nerve trunk, and classical neuralgia in the vast majority of cases occurs due to mechanical effects on the nerve. Today, experts identify dozens of factors that provoke the development of the disease.
Main causes of neuralgia
- Head injuries leading to changes in the cranial structure and displacement of bones.
- Benign and malignant tumors that, as they grow, compress the trigeminal nerve.
- Various bite pathologies and other dental anomalies.
- Pathologies of the structure and diseases of blood vessels located in close proximity to the nerve (atherosclerosis, aneurysm, vasodilatation, etc.).
- Sinusitis and otitis in chronic form.
- Trigeminal neuralgia after tooth extraction. Occurs during a traumatic or incorrectly performed extraction procedure.
- Damage as a result of infection resulting from a number of diseases: periodontitis, periodontitis, stomatitis, herpes, syphilis.
Trigeminal neuralgia from hypothermia occurs rarely. However, this factor contributes to the development of the disease and complicates treatment. The same can be said about decreased immunity, metabolic disorders, neurosis, diabetes and other complicating factors.
Facial neuritis (facial nerve neuropathy)
Paralysis of the facial muscles on one side of the face (prosopoplegia) as a result of damage to the facial nerve is a common disease that requires urgent treatment.
In a large number of cases, damage to the facial nerve (FN) occurs in the bony canal (pyramid of the temporal bone), before exiting the skull through the stylomastoid foramen. Bone canal L.N. is quite narrow, which contributes to compression of the nerve in it during the formation of edema. Edema is usually caused by impaired blood supply to the nerve as a result of hypothermia or a viral infection. In the first hours after the onset of paresis of the facial muscles, therapeutic measures should be aimed at relieving swelling of the facial nerve. Otherwise, irreversible death of nerve fibers may occur. On the first day of the disease, it is important to establish the location, nature and extent of nerve damage. In the following days, the diagnosis aims to accurately establish the etiological factor - infection, ischemia, etc.
In accordance with these standards, our clinic primarily performs brain tomography (MRI, CT) and electromyographic study of L.N.
Localization of facial nerve damage
First of all, it is important to differentiate between the intracranial localization of the lesion, the lesion in the bony canal of the temporal bone and after the exit of the nerve on the face.
1. If paralysis of the facial muscles occurs simultaneously with the appearance of hemiplegia (weakness) in the limbs of the ipsilateral (same) half of the body, then we are talking about a focal lesion of the opposite hemisphere of the brain. The most likely cause is a stroke. Brain tomography in this case makes it possible to clarify the cause of hemisphere damage (tumor, multiple sclerosis?). In mild cases, tomography does not reveal lesions. In this case, EEG (electroencephalographic study) allows one to differentiate between damage to the cerebral cortex and subcortical (lacunar) strokes. We do not perform EMG in cases of hemispheric lesions.
In rare cases, limited central damage (damage to the cerebral hemispheres) appears only on the face. In this case, a simple forehead wrinkling test can exclude a central lesion. The forehead muscles receive innervation from both hemispheres. Therefore, if one of the hemispheres is damaged, the forehead muscles do not suffer. At the same time, when the facial nerve itself or its nuclei are damaged, paresis of the facial muscles of the entire half of the face, including the muscles of the forehead, is observed.
*It must be remembered that the masticatory muscles receive innervation from the trigeminal nerve system. Therefore, their function is preserved. The oculomotor muscles, innervated by the 3rd, 4th and 6th pairs of cranial nerves, are also preserved. Ptosis (drooping eyelid) is not a symptom of facial nerve damage. On the contrary, damage to the facial nerve is characterized by the inability to close the eye.
2. Damage to the nuclei of L.N. in the brainstem is usually accompanied by paralysis or paresis of the limbs of the opposite side (Millard-Hubler syndrome) and/or paresis of the abducens nerve on the same side, due to the involvement of the nucleus n. Abducens (Fauville syndrome). The latter is manifested by convergent strabismus: the inability to move the eye of the affected side to the side.
*The upward movement of the eyeball when the eyes are closed (Bell's phenomenon) is not a symptom of damage to the oculomotor nerves.
We definitely do an MRI, since MRI is better at visualizing the deep structures of the brain than CT. Brain tomography visualizes structural abnormalities. We obtain additional information about the localization of functional disorders by conducting EMG studies of the blink reflex (R1 and R2 components of the blink reflex are generated in different parts of the brainstem) and acoustic brainstem evoked potentials (Components IV are generated in different parts of the brainstem).
Most often, disorders at this level are caused by demyelinating disease, tumors, vascular malformations, syringomyelia, etc. With the sudden appearance and development of symptoms (within hours) of damage to the hemispheres or brain stem, an acute cerebrovascular accident is assumed. The patient is admitted to the intensive care unit.
3. The third variant of intracranial lesion is the lesion of L.N. along the path from the brain stem to the entrance to the bony canal of the temporal bone (porus acusticus internus) in the so-called cerebellopontine angle. Here the facial nerve follows next to the auditory nerve and the intermediate (regulates tear and salivation, carries taste fibers from the anterior two-thirds of the tongue) nerve. Therefore, with pathology in the area of the cerebellopontine angle, in addition to paresis of the facial muscles, there is deafness on the same side, loss of taste on the same side of the tongue, dry mouth and decreased tear production may be felt.
The most common causes are acoustic neuroma, vascular malformations, basal gliomas, etc. MRI is performed to verify the diagnosis. If necessary, contrast-enhanced MR angiography is performed. Throughout the entire length from the cerebellopontine angle to the exit of the facial nerve to the face, the symptoms of its damage may indicate the presence of a serious ENT pathology: purulent otitis, with the formation of a fistula, mastoiditis (inflammation of the mastoid process), etc. Therefore, in case of the specified localization of the lesion, a consultation with an ENT specialist is required in our clinic.
4. Upon entering the bony canal, the facial and intermediate nerves diverge from the auditory nerve. Therefore, with damage to the canal, deafness (if it is not associated with ENT pathology) is not observed. On the contrary, so-called hyperacusis is detected - increased sensitivity of the ear to sounds, especially high tones. This phenomenon is associated with dysfunction of the nerve fibers that run as part of the L.N. to muscle m. Stapedius of the inner ear, which regulates the adjustment of the mechanical part of the sound-receiving apparatus.
5. Symptoms of damage to the facial nerve in the bone canal of the temporal bone. As the facial nerve moves from inside to outside in the canal, the following nerve branches are successively separated from it: n. Petrosus major (lacrimation), n. Stapedius (to the muscle m. Stapedius), Chorda timpani (salivation and taste fibers). Therefore, when the nerve lesion is localized before the origin of n. Petrosus major, no lacrimation observed. Hyperacusis can be observed only when the nerve is damaged before the n. Stapedius. Dry mouth and taste disturbances occur if the nerve is affected before the Chorda timpani leaves. The latter departs from the facial nerve close to its exit from the bone canal to the outside.
Bell's palsy - paralysis of the facial muscles of half the face with the addition of these symptoms, resulting from swelling and compression of the nerve in the bone canal - the most typical case of L.N. neuropathy.
Hunt's neuralgia (Ramsey Hunt syndrome) is Bell's palsy + pain and the presence of characteristic bubbles in the area of the external auditory canal, pinna and behind the ear. Hunt's neuralgia is a sign of herpetic nerve damage. In this case, we carry out a serological blood test for Herpes Zoster.
6. After the release of L.N. outward from the stylomastoid foramen, it branches on the face. Here it is available for direct study using electromyographic methods. Typically, M-responses of the nasal muscles, orbicularis oculi and oris muscles are studied when the nerve at the exit from the stylomastoid foramen is stimulated. Identification of signs of neuropathy in the peripheral part of the facial nerve on both sides indicates the presence of polyneuropathy. In this case, an EMG study of the nerves of the limbs is performed to verify the presence of polyneuropathy.
After branching, some branches pass through the parotid gland. Tumors of the parotid gland can cause their damage.
If an EMG study is performed in the first 4 days (preferably in the first two days) after the onset of paralysis of the facial muscles, then these studies allow for differential diagnosis of lesions on the face and inside the bone canal (when topical diagnosis based on the clinical symptom complex is impossible). After 4-7 days, Wallerian degeneration of distal nerve fibers (on the face) may occur if they are damaged proximally (in the canal).
NB: Intracranial lesion indicates the presence of serious diseases that threaten to lead to damage to other parts of the brain if not diagnosed and treated in a timely manner. The first examination of the patient is brain tomography.
Neuritis of the facial nerve in the classic form, i.e. in case of damage in the bone canal and in the facial area, it also requires urgent hospitalization of the patient in a neurological hospital with immediate anti-edematous therapy, the basis of which is corticosteroids. It is important to carry out timely measures to restore nutrition and blood supply to the nerve.
*Facial nerve neuritis is a common but outdated name. More correctly, neuropathy of the facial nerve, since this concept includes not only inflammatory (neuritis) diseases, but also nerve lesions of other etiologies.
Objective criteria for the severity of facial nerve damage.
Nature of the lesion and prognosis.
Please note that slight facial asymmetry without facial muscle weakness is not a consequence of facial neuritis. Close your eyes, stretch your lips in a wide smile, whistle, wrinkle your forehead and frown - make sure that the muscles are really paralyzed.
1. The first EMG study for neuropathy of the facial nerve is recommended to be carried out in the first 4 days after paralysis. The study consists of two parts: EMG of the facial nerve and study of the blink reflex on both sides. With EMG L.N. recording is made from the facial muscles innervated by direct stimulation of the nerve in the area where it exits the bone canal. The blink reflex is recorded from both orbicularis oculi muscles when the trigeminal nerve is stimulated. The impulse along the trigeminal nerve enters the brain stem, where it switches and enters the nuclei of the L.N. on both sides. After which, from the core of L.N. the impulse travels along the entire nerve (including the bone canal) to the facial muscles.
Three typical types of lesions with neuritis of the facial nerve and their interpretation:
— deviation from the norm in EMG L.N.: lesion on the face
- normal EMG results of L.N., but the amplitude of the R1 component of the blink reflex is reduced: lesion in the bone canal - complete destruction of axons or axonotmesis (incomplete damage to the axon with the formation of a persistent block of conduction along it). Complete absence of the reflex is an unfavorable prognosis.
- normal EMG results of L.N., but the latency of the R1 component of the blink reflex is increased: demyelination of the nerve (damage to the myelin sheath). Favorable prognosis.
2. The second EMG study is recommended to be carried out 10-15 days after paralysis. The following EMG signs allow you to verify the diagnosis:
— decrease in amplitude (%) of the M-response of the facial muscles during EMG L.N. compared with the first study in proportion to (%) irreversible degeneration of nerve fibers. If the amplitude has not decreased, the prognosis for complete recovery is favorable.
— the amplitude of the M-response is preserved, but the amplitude of the reflex response is significantly reduced with normal latency: axonotmesis, restoration of nerve function may take several months (with adequate therapy).
— the amplitude of the M-response remains at the same level, but the latency of the first component of the blink reflex is significantly increased. Compared to the first study, a clear correction of the deviation of the reflex component from the norm is noted. Recovery occurs due to remyelination (restoration of the myelin sheath of the nerve). The prognosis is favorable. Recovery within several weeks with adequate therapy.
— The M-response of the facial muscles has disappeared: an extremely unfavorable prognosis. Formation of facial muscle contractures.
- The M-response has sharply decreased, the reflex response is absent in the first and second studies of the blink reflex. The prognosis is unfavorable. Recovery is possible by the sprouting of new fibers into denervated muscles with the formation of aberrant conduction (hemifacial spasm, tics).
If it is not possible to compare with the first study (late hospitalization), from 2-3 weeks from the onset of the disease, it is possible to conduct needle EMG of the facial muscles to verify axonal damage.
3. The third study is recommended to be carried out 1.5-2 months from the onset of paralysis. In addition, during the treatment process there is often a need to evaluate the effectiveness of the therapy. Then additional research is carried out on an individual basis. In addition, if the restoration of the nerve as a result of axonotmesis lasts for several months, we repeat the neurophysiological study after 3-4 and after 5-6 months.
There is no need to dramatize the situation if you notice sudden paralysis of the muscles of half the face. As a result of systematic tactics of therapeutic and diagnostic measures, timely therapy aimed at limiting the spread of the pathological process, and a pathogenetically determined approach to identifying the etiology of the disease, it is possible to achieve complete restoration of facial muscle function in the vast majority of patients. But remember: if you have neuritis of the facial nerve, you must immediately consult a doctor. Treatment and examination should be started within the first hours of the onset of the disease.
For information about making an appointment with specialists, please contact us by phone: 8;, or by email. The email address is being protected from spambots. Javascript must be enabled in your browser to view the address. / The email address is protected from spambots. Javascript must be enabled in your browser to view the address.
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
Symptoms
Manifestations of the disease occur acutely, within a few hours, for a maximum of 3 days. The gradual appearance of signs is most typical of compression of the nerve by a tumor growing from the surrounding tissue.
Depending on the severity, neuritis of the facial nerve is accompanied by the following symptoms:
- movements of the facial muscles are weakened, up to barely noticeable, disruption of conjugate contractions of symmetrical areas of the face;
- facial asymmetry, even disfiguring;
- difficulty closing the eyes; in severe cases, the palpebral fissures do not close completely;
- disorders of swallowing, chewing, speech;
- when the disease is complicated by keratitis, vision loss gradually develops;
- taste disturbance, weakening or strengthening of sound sensations;
- lacrimation;
- with simultaneous damage to the trigeminal nerve - severe pain in the facial area.
Signs of intoxication and fever are uncharacteristic and usually occur due to the infectious nature of neuritis of the facial nerve.
Types of trigeminal neuralgia
There is an additional classification that can also be used in making a diagnosis.
Acute
Acute trigeminal neuralgia, accompanied by frequent and severe attacks.
Chronic
Chronic trigeminal neuralgia is a consequence of an untreated disease. The patient has been observed for a long time: remissions alternate with exacerbations.
Atypical
Atypical trigeminal neuralgia occurs against a background of stress and nervous exhaustion (psychosomatics).
Postherpetic
Postherpetic trigeminal neuralgia occurs after a history of herpes and its symptoms differ from the classic type. The pain is usually burning and may not go away for two to three hours.
Causes
Facial neuritis occurs under the influence of the following etiological factors:
- in 15% of patients this is damage to the branches of the nerve during surgical interventions on the middle ear, mastoid process, and also associated with otitis media and other lesions of the hearing organ, for example, cholesteatoma;
- in rare cases, the disease is caused by infection - herpes virus (Hunt syndrome), mumps, polio, influenza, as well as Lyme disease, transmitted through tick bites;
- in 75% of cases, the cause of neuritis of the facial nerve cannot be determined; in this case, they speak of Bell's palsy, which worsens after hypothermia and colds.
Other causes include head trauma, surgery on the salivary gland, and removal of an acoustic neuroma.
Diagnosis of the disease
Modern medicine has in its arsenal many diagnostic techniques that make it possible to determine the type of neuralgia and the cause of its occurrence:
- visual examination and questioning of the patient;
- X-ray of the jaw;
- MRI of the brain and blood vessels;
- laboratory analysis of urine and blood;
- electromyography.
Diagnosis is carried out by a neurologist, but additional examinations by other specialists are often required: dentist, ophthalmologist, otolaryngologist. Particular attention is paid to differential diagnosis, since neuralgia may resemble other diseases in its symptoms, in particular glaucoma, otitis media, ethmoiditis, Slader syndrome, etc.
Examination for facial nerve disease - find and eliminate the cause of the disease
The symptoms of facial nerve pain are almost the same in all cases, but its causes are different and require different treatments. Treatment “blindly” can delay the healing process. Therefore, in our clinic everything starts with searching for the exact cause and location of the nerve damage.
MRI of the brain, temporal bone. MRI scans show the brain centers of the facial nerve and its area of exit (root) to the base of the brain, blood vessels, and temporal bone. Circulatory disorders, cysts and tumors are easily recognized.
Blood tests to check for infections, biochemical changes that damage the facial nerve. The trigeminal nerve is a favorite area of attack by the herpes virus group. The suspicion of the presence of the virus and its activity can be easily verified using a blood test.
Electromyography, Blink reflex - measurement of electrical potentials of facial muscles. Helps assess the function of impulse transmission along the facial nerve, the degree of its impairment, judge the effectiveness of treatment, the presence of complications, and help in choosing the correct treatment tactics.
Stimulation electromyography of the facial nerve (electroneuromyography, myography of the facial nerve)
Treatment of trigeminal neuralgia
Treatment and drugs
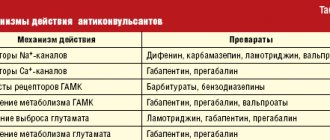
For successful treatment, complex drug therapy is used. First of all, these are anticonvulsants (carbamazepine, finlepsin or clonazepam), which are included in the mandatory rehabilitation program and relieve the main manifestations of neuralgia. The dosage and duration of treatment are determined strictly by the attending physician.
For additional effect, antihistamines and local pain relievers may be prescribed. To compensate for the lack of gamma-aminobutyric acid (a kind of mediator between the brain and the nervous system), baclofen, phenibut or gabapentin are prescribed. In the stage of exacerbation of neuralgia, specialists often prescribe antidepressants to eliminate psychological discomfort (the most common remedy is finlepsin). If the cause of the disease is a virus or infection, antiviral and antibacterial agents, as well as NSAIDs, are prescribed. During the recovery period, it is recommended to take B vitamins.
Physiotherapy
To eliminate pain, novocaine blockades and sodium hydroxybutyrate injections are actively used. The most popular and effective physiotherapeutic techniques: acupuncture, ultraphonophoresis, magnetic therapy, and low-frequency laser therapy. Massage for trigeminal neuralgia is also a good addition to general treatment and allows for better blood circulation.
Possible complications
Treatment of facial neuritis cannot be delayed. The later therapy is started, the greater the likelihood of developing complications:
- With a long course of the disease, the patient develops a persistent contracture of the facial muscles on the affected side: the muscles are involuntarily tense, contracted, and involuntary movements are possible. Recovery from such a complication is extremely difficult.
- The appearance of the face can change greatly: immobile muscles create a significant cosmetic defect.
- Persistent disturbances of taste.
- Corneal ulcers, infection, cataract formation, blindness.
- Constant spasm of the muscles of the face or eyelid.
Prevention
Taking into account the main causes of the disease, its prevention includes protection from colds, hypothermia, as well as timely treatment of diseases of the ENT organs. It is useful to harden the body, treatment in sanatoriums on the seashore, and a diet rich in B vitamins.
After suffering from facial neuritis, self-massage of the face with essential oil of fir or cedar is useful to prevent recurrence of the disease. It can be done at night during the cold season.
The paid services department of NIKIO invites patients with neuritis and neuropathies of the facial nerve for treatment. The patient is examined by an experienced doctor; a consultation with a candidate or doctor of medical sciences is possible. The clinic uses modern physiotherapy equipment. If necessary, the patient undergoes surgery to quickly restore the function of the damaged nerve.