According to WHO, among viral infections, the ARVI group of viruses is in first place, and the herpes simplex virus, which can affect the genital area, is in second place. The uniqueness of this virus lies in its ability to invade various organs and systems, causing a wide variety of clinical manifestations and complications. For this reason, the formation of a unified approach to the diagnosis and treatment of patients with herpes is one of the most important tasks of modern healthcare.
- Causes of herpes
- Types
- Manifestations and symptoms in men and women
- Diagnostics
- How to treat during pregnancy
- Is it possible to resort to folk ones?
- Prevention
In total, 8 types of herpes viruses are known: HSV-1, HSV-2, varicella zoster virus, Epstein-Barr virus, cytomegalovirus, HSV-6, HSV-7, HSV-8. The structure of virus particles of different types is practically no different from each other. The virus shell contains antireceptors, thanks to which it can attach to almost any tissue and affect the skin, mucous membranes, central and peripheral nervous systems, liver, blood vessels and blood cells. In addition, in some cases, HSV can lead to malignant transformation of cells.
Genital herpes is caused by herpes simplex virus type 2 (HSV-2), and less commonly by herpes simplex virus type 1 (HSV-1). Previously, it was believed that HSV-1 manifested itself exclusively as rashes on the face, but it has now been established that each of these two types of viruses can also infect the genitals.
What is genital herpes
The content of the article
Genital herpes is one of the most commonly diagnosed sexually transmitted diseases in both men and women. The causative agent is the herpes simplex virus type HSV-1 and HSV-2. In many people, the disease is completely asymptomatic, so the likelihood of infection through sexual contact is very high.
Symptoms of genital herpes are easy to recognize by visual examination. Mild pain and changes appear on the skin of the genitals and perineum, resembling blisters. The first wave of the disease can last from 2 to 3 weeks, sometimes less. When the disease relapses, the symptoms of GG are usually less disturbing than the first time.
Special antiviral drugs alleviate the condition. Patients whose symptoms of genital herpes appear regularly are forced to take medications every day.
Reasons for appearance
Genital herpes can be transmitted through any sexual contact (oral, anal, vaginal). The source is people suffering from a similar disease, or those who have hidden symptoms. It is almost impossible to become infected through household means. The incubation period for this disease ranges from 1 to 26 days.
Modern medicine distinguishes between primary and recurrent types of the disease. The causes of relapse of the disease can be hypothermia, infections, alcohol consumption, and stress. True, such rashes heal faster - within one week.
The causative agent of the disease
Herpes (from the Greek ἕρπης - creeping, spreading skin disease). Genital herpes is a viral infection that affects the penis in men (penile herpes) and the external genitalia and vagina in women (herpes vaginalis, labia), as well as the area around the genitals, usually the perineum. Infection is manifested by the appearance of blisters on the skin. Sometimes they can occur on the buttocks and anus.
The causative agent of the disease is the human herpes virus. There are two types of AI virus: herpes virus type 1 and herpes simplex virus type 2.
- AI virus type 1 most often leads to the appearance of herpes on the lips. Causes half of the cases of genital herpes.
- AI virus type 2 is responsible almost exclusively for the development of genital herpes. Very rarely it can also cause herpes on the lips.
Herpes on the lips
Clinical features of herpetic infection in women
Herpes of the urethra and bladder
Herpetic urethritis in women is subjectively manifested by pain and cramping at the beginning of urination, and a frequent urge to urinate. With herpetic cystitis, hematuria, pain at the end of urination, blood in the urine, and pain in the bladder area appear.
Herpetic cystitis
In a woman, the first and only sign of HSV infection may be in the genitourinary tract. It often occurs in the first 1-3 months after the start of sexual activity or a change of sexual partner.
Herpes of the anal area and rectum
The lesion in the anal area usually represents a recurrent fissure, which is often a reason for diagnostic errors. Such patients with an erroneous diagnosis of “anal fissure” end up with surgeons. The itchy form of herpes anus and herpetic lesions of hemorrhoids are also difficult to diagnose.
The list of diseases etiologically associated with HSV is constantly growing. According to the literature, in 3.6% of women suffering from treatment-resistant colpitis and cervical leukoplakia, HSV is one of the etiological factors of the disease. A new form of latent intrauterine HSV-II infection with localization of the pathological process in the glandular epithelium of the endometrium is described. It has been proven that HSV can cause the development of endometritis and salpingoophoritis.
The asymptomatic form of herpes of the internal genitalia is detected in 20-40% of women suffering from herpes of the buttocks and thighs. This important circumstance must be taken into account when planning pregnancy in women with this form of GC due to the existing likelihood of developing complications of HSV infection during pregnancy.
The etiopathogenetic role of HSV in cervical cancer has been established. The above emphasizes the growing etiological role of HSV in the structure of diseases of the pelvic organs in women.
Herpes and pregnancy
The prevalence of HSV among pregnant women in the United States is 22-36%, in Europe 14-19%. Viremia in women during pregnancy can cause fetal death, stillbirth, and premature birth. Herpes viruses cause up to 30% of spontaneous abortions in early pregnancy and over 50% of late miscarriages; they are second only to the rubella virus in terms of teratogenicity (the development of fetal deformities).
The most severe forms of neonatal herpes develop when a newborn is infected with the herpes simplex virus during childbirth. With primary herpes in the mother, from 30% to 80% of children are infected, with recurrent herpes – 3–5%. Infection of the fetus during delivery, if the mother had herpetic eruptions at the end of pregnancy, occurs in 50% of women with RGG; however, 60–80% of infected children develop encephalitis.
Ways of infection with genital herpes
Genital herpes is transmitted primarily through sexual contact with a person who is already a carrier of the virus. The thin, delicate mucous membranes of the mouth, genitals and anus are very vulnerable to viruses and infections. This allows the virus to pass from one person to another during sexual intercourse, including oral and anal sex.
Transmission of the virus from the lips to the genitals occurs during oral sex, when one of the partners has signs of herpes on the lips. The herpes simplex virus can also enter the body of another person through wounds or cracks in the skin on other parts of the body: fingers, palms, knees, etc., provided that the surface comes into contact with the infected area of the skin. Re-infection with your own virus through accidental touch is unlikely.
Local immunomodulators for HPV and HSV
Among the “universal” drugs that can be prescribed for various viral infections - from common respiratory infections to herpes and human papillomavirus - are interferons. In particular, preparations of human recombinant interferon alpha-2b.
Interferon alpha-2b has antiviral, immunomodulatory and antiproliferative properties. It suppresses the replication of RNA and DNA viruses, enhances the activity of macrophages, and increases the cytotoxicity of lymphocytes to target cells. The use of drugs containing interferon alpha-2b is accompanied by an increase in the level of immunoglobulins type A and normalization of IgE [5]. However, these therapeutic effects are fully manifested when the drug is administered systemically.
when its high concentration in the blood is reached. It should be noted that quite powerful side effects can develop, including fever, loss of appetite, headaches, muscle pain, joint pain and many other adverse reactions.
Due to the specific safety profile, injectable interferon preparations are prescribed only in very serious cases, when the risk of side effects is justified - for example, in the treatment of hepatitis, a number of oncological diseases, etc. HSV and HPV infections do not apply to such situations and are not indications for systemic interferon administration. At the same time, the Russian Federation has registered a very impressive list of local forms of interferon alpha-2b, including ointments/creams for treating mucous membranes with genital herpes.
Theoretically, local interferon preparations should have all the advantages of injectable ones and not have their side effects, since local forms are either very slightly absorbed into the systemic circulation or do not penetrate into the blood at all. However, today there is no sufficiently reliable evidence of the effectiveness of interferons when applied topically. However, in domestic practice they are quite often prescribed as part of the complex treatment of recurrent genital herpetic infections.
Along with local forms containing only interferon alpha-2b, several combination drugs are also registered in the Russian Federation:
- Interferon alpha-2b + acyclovir + lidocaine, ointment. Indications: HSV.
- Interferon alpha-2b + taurine + benzocaine, vaginal and rectal suppositories, prescription. Indications: HSV, HPV. Taurine, according to the instructions, acts in combination as a reparative, antioxidant and anti-inflammatory component.
+
High safety profile.
!
The feasibility of using local forms of acyclovir for genital herpes is subject to serious doubts due to insufficient activity, which is confirmed in Western recommendations [3]. Interferon alpha-2b preparations, both mono- and combined, are available with or without a prescription, depending on the indications of the dispensing rules in the instructions for a particular drug. It is important to draw the visitor’s attention to the fact that the first-line treatment for HPV - oral forms of acyclovir and valacyclovir - must be prescribed by a doctor, so you should be advised to immediately consult a doctor.
Asymptomatic course of the disease
The first infection with the herpes simplex virus is often called the primary infection. Such an infection can cause symptoms of the disease, but this does not occur in all cases. After the primary infection, the virus is not eliminated from the body; it lives in it in the form of an inactive form (in sleep mode).
In some people, the virus “wakes up” from time to time and enters the surface of the skin. This, in turn, causes a relapse of the viral disease on both the genitals and lips.
For most people, infection with the herpes virus in intimate areas is not a cause for concern. At least 8 out of 10 people with genital herpes don't even know they have it. Sometimes only very mild symptoms may appear that are difficult to associate with genital herpes. Such symptoms may include a slight burning sensation or slight redness that quickly disappears.
In such people, the virus remains dormant and never causes a wave of symptoms to return. However, even those who develop the disease asymptomatically are dangerous to their sexual partners. It is in such cases that infection with the herpes virus occurs.
Why does herpes appear on the pubis?
In addition to infection during sex, other ways of contracting the disease cannot be ruled out, for example, through close contact of a healthy person with a sick person.
But if herpes appears on the pubis, then this most likely means that sexual intercourse has taken place.
Reproduction of the virus begins at the site of penetration of the pathogen into the mucous membrane or skin.
At this point, vesicles containing clear liquid begin to form.
After this, the pathogen penetrates the bloodstream and affects the nerve endings.
It remains in them forever and periodically provokes relapses.
The virus leads to a decrease in the body's immune defense.
The disease can differ in various forms.
In approximately half of the cases the disease is accompanied by relapses.
After the process has completely subsided, a herpetic infection may make itself known several months or even years later.
Signs of genital herpes
At the initial stage of the disease, a person is worried about a slight increase in body temperature, general malaise and poor health. Small groups of blisters, often painful, appear around the genitals and/or anus. There may be visible changes on the skin of the labia, as well as the clitoris, in the area of the vaginal opening, on the thighs around the anus.
Herpes blisters
The blisters grow for one to two weeks before bursting and turning into small, painful sores. Lymphatic inguinal nodes are enlarged and identified, palpated as compactions, lumps in the upper thighs. Painful urination is often a concern.
Women may experience unusual vaginal discharge. The herpes virus in women affects the cervix, first blisters appear on it, then ulcers appear. Typically, blisters and ulcerative lesions develop within 10-20 days, after which they gradually disappear without leaving scars.
The first symptoms of genital herpes may appear months or even years after infection. Therefore, the first wave of symptoms may occur while a person is married or in a long-term relationship with a reliable partner.
It is not entirely known why some people experience symptoms of infection and others do not. It is also not fully understood why the first wave of symptoms occurs months or years after the actual infection. This may have to do with how the immune system responds to the virus in individuals.
Folk remedies
Herpes in an intimate place is treated with folk recipes in combination with medications. It is imperative to coordinate the chosen treatment with a specialist.
- Compresses with arnica. A decoction of arnica inflorescences is prepared from 12 g of herb and 400 ml of water. The product is infused for an additional 2 hours, pieces of natural fabric are soaked in it and applied to the inflamed areas.
- This recipe is for women. Candles made from beeswax with the addition of aloe and kalanchoe are very useful. Making them at home is not difficult. The plants are crushed, vitamins are added in ampoules B1 or B12, poured with molten wax and mixed thoroughly. The resulting product is laid out on a piece of bandage and a small candle is formed. Inserted into the anus or vagina. Depending on which organs the rash has formed on: in the back of the perineum or on the labia, you need to approach use specifically for each place.
- Infusion of birch buds. The drug is prepared from 25 g of phyto-raw materials and 1 glass of 70% alcohol. It is infused in the dark for 2 weeks, then filtered and used to rub herpes blisters.
- There is an effective folk method to strengthen the immune system. You need to extract juice from apples and onions. The proportions are taken 1/1. Dilute the liquid with pumpkin juice and consume a tablespoon 3 times a day. These products contain vitamins that have a positive effect on the immune system.
The simplest and most affordable recipe at home is aloe juice. The plant leaf is washed, cut and applied to the areas of infection. If there is a rash on the labia. You can grind aloe into a paste, apply it to the affected area, secure it with a bandage, and put on underwear on top. Compresses are changed after 1-3 hours.
Development of disease relapses
Some people sometimes experience recurrences of genital herpes. Scientists are unable to explain why, after the latent stage, the virus is activated from time to time, that is, the reasons for the relapse have not been established. Factors that contribute to the development of the virus and relapse of the disease are known:
- influenza, ARVI, other diseases with high body temperature;
- local damage to the external genitalia, as well as the mouth and lips;
- decreased defense mechanisms, immunodeficiency;
- ultraviolet radiation, a side effect of radiation therapy;
- changes in a woman’s immune system during menstruation;
- hypothermia;
- stress;
- excessive alcohol consumption.
ARVI
Stress
Relapses are often milder and last shorter than the first wave of the disease. In case of relapses, symptoms usually occur within 7 to 10 days. Most people do not complain of either elevated body temperature or poor health. A relapse of the disease may be indicated by a slight tingling sensation or itching of the genitals for 12-24 hours.
Over time, relapses of genital herpes appear less frequently. The frequency of their occurrence may vary. For some people they occur six or more times during the year, for others much less often. As a rule, during the first 2 years from the first wave of symptoms, relapses occur 4 to 5 times. Some people do not relapse at all.
Causes of relapses of herpes
The risk of relapse is often associated with:
- with high sexual activity
- with the last days of menstruation in women
- with what types of virus cause damage. The second type of virus provokes the development of relapse more often than the first
The occurrence of relapses can be influenced by factors that provoke a decrease in the body’s immune defense.
The most common influences on a disease outbreak are:
- changes in hormonal levels
- alcohol abuse
- presence of chronic infections
- hypothermia of the body, especially the lower torso and legs
- abuse of exposure to sunlight
The manifestation of pathology is often local in nature.
When the pubic area is primarily affected, a rash occurs in this area of the skin.
In some cases, the infection spreads to other areas of the skin and mucous membranes, involving the internal organ systems, including the brain.
If an exacerbation of the process occurs no more than one episode within 3 months, then such a course of the infectious process is considered favorable.
More frequent exacerbations are associated with a decrease in immune defense at the cellular level, which is characteristic of HIV.
In such patients, the appearance of new elements occurs against the background of old rashes.
The incidence of relapses in patients of both sexes is approximately the same.
But in men, the duration of the process is longer, and it is characterized by multifocal lesions.
In women, the period of exacerbation is reduced, but the process is more pronounced.
How to diagnose genital herpes
To diagnose the disease, a visual examination is generally sufficient. The type of changes, their location and other symptoms are sufficiently characteristic to make a diagnosis of genital herpes.
In case of doubt and for invasive infections, carry out:
- Isolation of the virus from a cell culture, examining the smear or the content of the bubbles, however, the absence of the virus in dilution (negative result) does not exclude infection;
- The polymerase chain reaction (PCR) method is a more sensitive method of testing a smear or fluid from the rash, but a negative result also does not rule out infection.
- Serological study. Allows the detection of antibodies to the HSV virus, which appear after a few weeks, as well as differentiation of the type of virus that caused the infection.
If antibodies against HSV-2 are detected, genital herpes is diagnosed, which poses a higher risk of relapse of the disease. Antibodies against HSV-1 indicate herpes simplex virus, so there is less chance of recurrence of lesions in the genital area.
Diagnostics
Diagnosis of genital herpes is performed using specific laboratory tests:
- Virological – gives results in 2 days;
- PCR (polymerase chain reaction) - allows you to detect the genetic material of the virus;
- Immunofluorescence analysis - detects pathogen antigens;
- Enzyme immunosorbent - allows you to detect antibodies produced by the body in response to exposure to HSV-2;
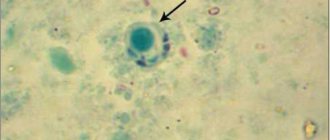
- Cytomorphological – assesses the degree of damage to infected cells.
Tests for genital herpes (urine, blood and scrapings from the vagina, cervix and urethral canal) should be taken a couple of times with an interval of 5-6 days. It is recommended to collect materials from women on days 18-20 of the cycle. This increases the chances of making a correct diagnosis.
Treatment of genital herpes
The use of antiviral drugs does not remove the virus from the body. Their goal is to suppress the reproduction process of the pathogen. The most effective use of medications is during the first manifestation of signs of the disease. Moreover, it is necessary to start therapy within the first five days from the moment the first symptoms appear. This allows not only to stop the spread of lesions, but also to reduce the duration of the disease.
The course of treatment for genital herpes is most often five days; if the rash persists, it is extended. To shorten the duration and relieve symptoms, you should start taking the drug as quickly as possible. The earlier treatment is started, the greater the chances of a rapid cure, effective reduction of symptoms and prevention of relapse of the disease.
In the treatment of relapses of the disease, antiviral drugs are not always used. Therapy is indicated and brings good results in cases of frequent severe symptoms. In case of frequent relapses, it is possible to take an antiviral drug every day. In people who use this form of treatment, relapses will either be completely absent or their frequency will be significantly reduced.
Controlling the cure of herpes in the vagina
After specific treatment, clinical symptoms are assessed.
Laboratory control is not required.
Because herpes infection cannot be cured.
If suppressive therapy is prescribed, the results are also assessed clinically.
After discontinuation of maintenance treatment, its effectiveness is judged by two relapses.
Assess the time intervals at which they occurred and how severe the symptoms were.
Based on the results of monitoring, a decision may be made to resume suppressive therapy.
Drugs for the treatment of genital herpes
Zovirax ®
(Zovirax)
. Original drug. The medicine is manufactured by Glaxo Wellcome, SA. The active ingredient is acyclovir 200 mg. Clinico-pharm. group: antiviral drug. Pharmaceutical therapeutic group: antiviral agent. Pharm. action: a synthetic analogue of purine nucleoside that inhibits the replication of Herpes simplex AI viruses types 1 and 2.
There are known generics of the drug Zovirax - Acyclovir (manufactured by Belupo, Croatia), Acyclovir (manufactured by Akrikhin, JSC Vertex, JSC Sintez, Russian Federation).
Drug for the treatment of genital herpes
Valtrex®. Original drug. The drug is manufactured by Glaxo Smith Kline, SA. Contains the active ingredient valacyclovir hydrochloride 556 mg (= valacyclovir 500 mg). Clinical and pharmacological group: antiviral drug. Pharmacotherapeutic group: antiviral agent. It is an L-valine ester of acyclovir. Valaciclovir is quickly and completely converted into acyclovir and valine in the body.
Immunomodulatory therapy
Another stage of complex treatment is immunomodulatory therapy aimed at strengthening the body's defenses. For this purpose, interferon preparations (Viferon, Genferon) are prescribed, as well as interferon inducers (Amiksin, Cycloferon), which have an antiviral effect and promote the production of interferon in the body.
A good effect is achieved by the use of vitamin therapy, in particular the prescription of calcium, zinc, vitamins B, C, E. In order to reduce the frequency of relapses, the patient may be prescribed subcutaneous administration of immunoglobulins. This treatment regimen helps restore the body's defenses and direct them to fight the viral infection.
Genital Herpes – Symptom Relief at Home
A cold compress (ice cubes wrapped in a towel) placed on the lower abdomen for 5-10 minutes may provide relief. Do not apply ice directly to the skin.
It is important to take in plenty of fluids.
Scented soaps, bath products and other similar products that may irritate the skin should be avoided. The best results are obtained by gently washing the genital area with a cotton swab and water. You cannot share towels, washcloths, or sponges. This minimizes the risk of infection to other family members.
Sexual abstinence is recommended until the blisters and ulcers disappear.
Genital herpes and sexual intercourse
If partners are carriers of the same virus, the possibility of re-infection is excluded. It is recommended to avoid intimate relationships from the moment the first symptoms appear until they disappear completely.
The herpes simplex virus is highly contagious when blistered. Sexual activity in this state is accompanied by a maximum risk of transmitting the virus to a partner. If there are no symptoms of genital herpes, the likelihood of transmitting the virus is reduced. However, this is possible because the virus is present on the surface of the skin of the genitals.
Using a condom during every sexual intercourse helps protect yourself from infection. However, it should be remembered that a condom does not guarantee complete protection against transmission of the virus to a partner, because it only protects the covered area of the body.
People who take antiviral medications for a long time are also less likely to contract the virus.
Genital herpes during pregnancy
To prevent genital herpes from developing in a child, a woman who has ever had symptoms of the disease should see a doctor (sometimes delivery by cesarean section is recommended). Sexual intercourse is prohibited from the third trimester of pregnancy if the woman’s partner not only has signs of genital herpes, but also suffered from the disease in the past. During this period, the risk of fetal infection is very high.
For many years, the development of an effective vaccine against genital herpes has been underway, unfortunately, so far to no avail.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Prevention
Preventive measures to prevent the occurrence of this disease include:
- quitting smoking, caffeine and alcoholic beverages;
- reviewing your diet, enriching it with vitamins A, C, E;
- avoid overheating and hypothermia;
- the microflora of the digestive system should be normal;
- maintaining physical activity;
- do not neglect massage and physiotherapy;
- consumption of bee products.
Vaginal herpes is a rather unpleasant and quite dangerous disease. To prevent its occurrence, it is necessary to follow the rules of personal hygiene and promptly contact a gynecologist when the first symptoms appear.