According to modern concepts, bacterial vaginosis is an infectious non-inflammatory syndrome of polymicrobial etiology, associated with dysbiosis of the vaginal biotope and characterized by a quantitative increase in obligate and facultative anaerobic opportunistic microorganisms and a decrease or complete disappearance of lactobacilli, especially those producing peroxide. The etiological spectrum of bacterial vaginosis is represented by microaerophilic, obligate anaerobic gram-positive and gram-negative bacteria ( Gardnerella vaginalis, Atopobium vaginae , Mobiluncus
spp,
Peptostreptococcus
spp.
, Prevotella
spp
., Bacteroides
spp. and etc.). As a rule, in laboratory studies it is possible to identify associations of various microorganisms that interact according to the principle of symbiosis [1].
According to epidemiological studies [2], bacterial vaginosis is one of the most common infectious diseases of the vagina, and the frequency of its detection varies from 12 to 80% and depends on the population of women examined.
Clinically, bacterial vaginosis is manifested by the presence of homogeneous discharge from the genital tract, often with an unpleasant odor, which significantly reduces the quality of life of patients. Symptoms of the disease also include the following: discomfort in the external genital area, pain during sexual intercourse (dyspareunia), and less commonly, itching and/or burning in the genital area.
Bacterial vaginosis is detected mainly in women of reproductive age. The disease does not pose an immediate threat to a woman’s life, but is a risk factor for the development of pregnancy complications: spontaneous abortion, intra-amniotic infection, premature rupture of amniotic fluid, premature birth. Also, bacterial vaginosis can potentiate the development of postoperative infectious complications, inflammatory diseases of the pelvic organs, peritonitis, abscesses of the pelvic organs with the introduction of intrauterine contraceptives. The long course of the disease is one of the risk factors for the development of cervical neoplasia, and also increases susceptibility to sexually transmitted infections (STIs), especially HIV infection and genital herpes [3, 4].
According to modern domestic and foreign recommendations, drugs from the 5-nitroimidazoles (5-NIMZ) group and clindamycin are used in the treatment of bacterial vaginosis [5, 6]. 5-NIMZ derivatives are drugs with a bactericidal action and selective activity against infectious agents. The targets of 5-NIMZ action in microbial cells are DNA, RNA and cellular proteins. Of all the representatives of the 5-NIMZ group, metronidazole, ornidazole and tinidazole are currently widely used.
Metronidazole is the most commonly used drug in the 5-NIMZ group in the treatment of infectious diseases. However, in recent years, studies have appeared demonstrating a decrease in the sensitivity of the etiological agents of urogenital trichomoniasis and bacterial vaginosis to metronidazole, which does not allow achieving the desired effectiveness of therapy. Numerous side effects are also known when using this drug, especially from the gastrointestinal tract.
Despite the possible cross-resistance of infectious agents to nitroimidazoles, the problem of their resistance to metronidazole can be most effectively solved by using other drugs of this group, for example, ornidazole. It should be taken into account that the effectiveness of therapy largely depends on the quality of the prescribed drug. One of the most important characteristics that determines the identity of pharmaceutically equivalent drugs according to the main pharmacokinetic parameters in vivo
, is bioequivalence. In this case, drugs are equivalent if they provide the same bioavailability of the drug substance. Most original drugs (as opposed to generics) are manufactured in accordance with GMP standards and, in addition to pharmacokinetic studies under various conditions, undergo extended clinical studies up to phase IV.
Tiberal is an original high-quality preparation of ornidazole, which has confirmed a high profile of efficacy and safety of use in numerous studies on the treatment of patients with bacterial vaginosis [7-9]. Tiberal, like other drugs of the 5-NIMZ group, is active against gram-negative and gram-positive anaerobic bacteria and protozoa. However, when developing the drug, the already known disadvantages of metronidazole were initially taken into account, which made it possible to improve its pharmacological properties. Thus, after taking Tiberal, the effective concentration in the blood is maintained much longer, which is associated with the half-life of the drug, which is 13-14 hours (for metronidazole - 8.5 hours), and the maximum concentration of Tiberal in the blood is observed already 3 hours after its oral administration administration, while less than 15% of the drug is bound to plasma proteins (metronidazole - more than 20%).
The purpose of the study was to study the effectiveness, safety and tolerability of the use of tiberal (ornidazole) tablets in the treatment of patients with bacterial vaginosis in comparison with the effectiveness of therapy with trichopolum (metronidazole) in the same form.
Material and methods
The study included 60 patients aged from 18 to 42 years (average age - 20.6 years) with a diagnosis of bacterial vaginosis, established in accordance with the Amsel criteria (presence of homogeneous - creamy vaginal discharge with a characteristic “fishy” odor, detection of “key cells" upon microscopic examination, pH value of vaginal contents >4.5, positive amino test result). All patients excluded sexually transmitted infections, candidiasis of the vulva and vagina, and the presence of opportunistic microorganisms - Ureaplasma
spp
., M. hominis
.
The complex of laboratory tests included: microscopic examination of biological material from the urethra, lateral and posterior vaginal vaults, and cervical canal; bacteriological examination to identify opportunistic and non-pathogenic ( Lactobacillus
spp
.
) microorganisms;
polymerase chain reaction (PCR) study to identify N. gonorrhoeae
,
T. vaginalis, Ch . trachomatis , M. genitalium , Ureaplasma
spp
., M. hominis, A. vaginae , G. _ vaginalis
; serological testing for syphilis and HIV.
After clinical and laboratory studies, all patients were divided into two groups according to the prescribed therapy:
Group 1 - 30 patients who were prescribed therapy with Tiberal (ornidazole) orally in tablets of 500 mg 2 times a day for 5 days; Group 2 - 30 patients who were prescribed therapy with Trichopolum (metronidazole) orally in tablets of 500 mg 2 times a day for 7 days.
A comparative assessment of the effectiveness of the use of prescribed drugs was carried out 14 days after the end of therapy according to the following parameters: the presence/absence of subjective symptoms of the disease (patient complaints), the presence/absence of objective symptoms of the disease, the presence/absence of laboratory signs of the disease, assessment of the effectiveness of therapy by the patient, assessment of the effectiveness of therapy doctor.
The intensity of subjective and objective symptoms was assessed on a 4-level scale: 0—absent, 1—weak, 2—moderate, 3—strong.
Safety parameters included adverse drug events, physical examination findings, and vital signs.
Giro
Ornidazole should be taken orally after meals with a small amount of water.
Trichomoniasis
Adults:
1 tablet 2 times a day (morning and evening) for 5 days.
Women must additionally be prescribed ornidazole in the form of vaginal tablets. If necessary, you can repeat the course of treatment. Between courses you should take a break of 3-4 weeks with repeated control laboratory tests.
An alternative treatment regimen is to prescribe 2 g once to the patient and his sexual partner.
Treatment is carried out simultaneously for both sexual partners.
Children:
The daily dose for children is 25 mg/kg body weight and is prescribed in one dose.
| Amoebiasis Possible treatment regimens: Duration treatment | Daily dose | |
| Adults and children weighing more than 35 kg | Children weighing up to 35 kg | |
| a) 3 days | 3 tablets at a time in the evening. For body weight over 60 kg - 4 tablets (2 tablets morning and evening). | 40 mg/kg body weight in one dose |
| b) 5-10 days | 2 tablets (1 tablet morning and evening) | 25 mg/kg body weight in one dose |
Adults:
For asymptomatic amebiasis, 500 mg (1 tablet) 2-3 times a day for 5-7 days.
For chronic amebiasis, 500 mg (1 tablet) 3 times a day for 5-10 days.
For acute amoebic dysentery, 1.5 g (3 tablets) 1 time per day.
For liver abscess, the maximum daily dose is 2.5 g in 1 or 2-3 doses, for 3-5 days, in combination with antibiotics (tetracyclines) and other treatment methods.
Giardiasis
Adults and children weighing more than 35 kg: 3 tablets once in the evening.
Children weighing less than 35 kg: 40 mg/kg once daily.
The duration of treatment is 1-2 days.
Infections caused by anaerobic bacteria
Adults:
500 mg (1-2 tablets) 3 times a day during or after meals.
Ornidazole can be used in monotherapy or in combination with other antibacterial drugs.
Children:
The daily dose for children is 10 mg/kg body weight and is prescribed 2 times a day. The average treatment period should not exceed 7 days.
Prevention of infections caused by anaerobic bacteria (before abdominal surgery, in gynecology and obstetrics)
First, 1 g (2 tablets of 500 mg) in a single dose, then 1 tablet of 500 mg 2 times a day for 3-5 days.
Helicobacter pylori eradication
500 mg 3 times a day for 7 days (as part of combination therapy, for example, with amoxicillin 2.25 g/day).
results
The main subjective manifestations of bacterial vaginosis in the examined women were pathological discharge of a creamy homogeneous nature from the genital tract, which was observed in 30 (100.0%) patients of the 1st group and in 29 (96.7%) patients of the 2nd group. Also, patients of the 1st and 2nd groups complained of an unpleasant “fishy” smell of discharge from the genital tract - 28 (93.3%) and 27 (90.0%), respectively, discomfort in the genital area - 16 (53, 3%) and 14 (46.7%) patients, respectively, and pain during sexual intercourse - 10 (33.3%) and 11 (36.7%) patients, respectively.
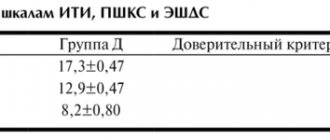
In all examined patients, microscopic examination of the vaginal contents revealed “key cells.” A positive amino test result was determined in 29 (96.7%) patients of the 1st group and in 30 (100%) of the 2nd group. Also, most patients showed an increased pH value of the vaginal contents - more than 4.5. Both groups were comparable in terms of clinical signs of bacterial vaginosis (Fig. 1).
Rice. 1. Results of clinical examination of patients before prescribing therapy (p>0.05).
The average severity of pathological discharge according to patients of the 1st group was 2.4, according to patients of the 2nd group - 2.2; unpleasant odor of discharge from the genital tract - 1.7 and 1.7; discomfort in the genital area - 1.2 and 0.8; pain during sexual intercourse – 0.6 and 0.6, respectively. According to the results of an objective examination, the average severity of pathological discharge in patients of the 1st group was 2.3, in patients of the 2nd group - 2.2.
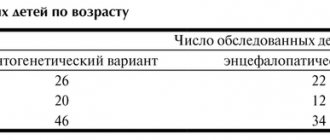
When analyzing the qualitative composition of vaginal microflora, the following results were obtained :
A. vaginae
was identified in 12 (40.0%) patients of group 1 and 16 (53.3%) of group 2
, G. vaginalis
- in 28 (93.3%) and 29 (96.7%) patients, respectively.
Other microorganisms associated with bacterial vaginosis were also identified: Mobiluncus , Leptotrix
(Fig. 2).
Rice.
2. Results of laboratory tests of patients before prescribing therapy. According to the bacteriological study, the majority of the examined patients (83.3% of patients of the 1st group and 80.0% of the 2nd group) had representatives of the Lactobacillaceae
were not determined, in 3 (10%) and 3 (10%) patients of the study groups, respectively, the number of lactobacilli was at the level of 102-103 CFU/ml, and in 2 (6.7%) and 3 (10%) patients, respectively - at the level of 104-105 CFU/ml (Fig. 3).
Rice.
3. Results of assessing the lactobacillary component of the vaginal microflora before prescribing therapy in patients of the examined groups. After establishing that the clinical and laboratory data of the examined patients met the criteria for inclusion in the study, all patients were prescribed therapy according to the regimens given in the “Material and Methods” section.
14 days after the end of therapy, subjective and objective clinical indicators were assessed, and laboratory tests were performed.
According to the results of a survey of patients, it was found that 1 (3.3%) patient of the 1st group and 5 (16.6%) patients of the 2nd group complained of discharge from the genital tract. Also, 1 (3.3%) patient of the 1st group and 4 (13.3%) patients of the 2nd group complained of an unpleasant “fishy” smell of pathological discharge. Discomfort in the genital area bothered 4 (13.3%) patients of the 2nd group, pain during sexual intercourse was noted by 1 (3.3%) patient of the 2nd group.
When assessing the nature of vaginal discharge, the following data were obtained: in 1 (3.3%) patient of the 1st group and 4 (13.3%) of the 2nd group, the vaginal discharge had a creamy character and an unpleasant “fishy” odor, characteristic of a bacterial vaginosis; in 1 (3.3%) patient of group 2, vaginal discharge was cheesy and accompanied by hyperemia and swelling of the vaginal mucosa. A positive amino test result was determined in 4 (13.3%) patients of the 2nd group, a vaginal pH value of more than 4.5 - in 1 (3.3%) patient of the 1st group and 3 (13.3%) of the 2nd group. th group. Microscopic examination of the vaginal contents in 1 (3.3%) patient of the 1st group and 4 (13.3%) of the 2nd group revealed “key” cells, which also confirmed the diagnosis of bacterial vaginosis in the examined women (Fig. 4 ).
Rice. 4. Results of clinical examination of patients after therapy (p<0.05).
The severity of pathological discharge according to the patient of the 1st group was 2.0, according to the patients of the 2nd group - 2.2; unpleasant odor of discharge from the genital tract - 1.0 and 1.6, respectively; discomfort in the genital area - 0 and 1.6, respectively; pain during sexual intercourse - 0 and 1.0, respectively. According to the results of an objective examination, the severity of pathological discharge in the patient of the 1st group was 2.0, in the patients of the 2nd group - 2.2.
A qualitative assessment of the vaginal microflora revealed that
A. vaginae
and
Mobiluncus
were identified in the vaginal contents only in patients of group 2 in 3 (10.0%) and 2 (6.7%) subjects, respectively.
G. _ vaginalis
were detected in 1 (3.3%) patient of group 1 and 2 (6.7%) patients of group 2 (Fig. 5).
Rice.
5. Results of bacterioscopic examination of vaginal contents in patients of the examined groups after therapy (p<0.05). When assessing the lactobacillary component of the vaginal microflora after therapy, it was found that normalization of indicators (the number of lactobacilli at the level of 105-107 CFU/ml) was achieved in 21 (70.0%) patients of group 1 and in 14 (46.7% ) patients of group 2. It was noteworthy that 10 (33.3%) patients of group 2 had representatives of the Lactobacillaceae
were not determined; in group 1 this figure was 10% (Fig. 6).
Rice.
6. Results of assessment of the lactobacillary component of the vaginal microflora in patients of the examined groups after therapy (p<0.05). There was no significant difference in the ease of use of the drugs. However, when analyzing adverse drug events, it was revealed that 6 (20.0%) patients of group 2 experienced side effects from the gastrointestinal tract (nausea, metallic taste in the mouth, pain in the epigastric region, diarrhea) during treatment with metronidazole ). In 1 (3.3%) patient of group 1, discomfort in the epigastric region was recorded during treatment, which resolved spontaneously after completion of therapy.
When monitoring vital signs, no clinically significant deviations were identified in any of the examined patients.
Gairo 500 mg No. 10 tab.
Instructions for medical use of the drug GAYRO Trade name Gayro International nonproprietary name Ornidazole Dosage form Film-coated tablets 500 mg Composition One tablet contains the active substance: ornidazole 500 mg, excipients: microcrystalline cellulose, lactose, colloidal silicone dioxide, povidone (K-30 ), sodium lauryl sulfate, purified talc, magnesium stearate, croscarmellose sodium film coating: hypromellose (HPMC E-15), polyethylene glycol 400, purified talc, quinoline yellow, brilliant blue, titanium dioxide, polyethylene glycol 6000 Description Biconvex, green, oblong tablets , covered with a film shell with a fault line on one side and a smooth surface on the other. Pharmacotherapeutic group Antimicrobial drugs for systemic action. Imidazole derivatives. ATC code J01XD03 Pharmacological properties Pharmacokinetics After oral administration, ornidazole is rapidly absorbed from the gastrointestinal tract. On average, absorption is 95%. Maximum plasma concentrations are achieved within 3 hours. Blood protein binding is about 13%. The active substance penetrates into the cerebrospinal fluid, into breast milk, passes through the blood-brain barrier (BBB) and the placenta. The concentration of the drug in blood plasma varies between 6-36 mg/l. Ornidazole is metabolized in the liver by hydroxylation, oxidation and glucuronidation to form 2-hydroxymethyl and alpha-hydroxymethyl metabolites. Both metabolites are less active against Trichomonas vaginalis and anaerobic bacteria than unchanged ornidazole. The half-life is approximately 13 hours. After a single dose, 85% of the dose is excreted through the kidneys during the first five days, mainly in the form of metabolites. Pharmacodynamics Gairo is an antiprotozoal, bactericidal and antimicrobial drug, a derivative of 5-nitroimidazole. The mechanism of action is the biochemical reduction of the 5-nitro group of ornidazole by intracellular transport proteins of anaerobic microorganisms and protozoa. The reduced 5-nitro group of ornidazole interacts with the DNA of microorganisms and inhibits the synthesis of their nucleic acids, which leads to the death of bacteria. Active against Trichomonas vaginalis, Gardnella vaginalis, Giardia intestinalis, Entamoeba histolytica, Lamblia spp., as well as obligate anaerobes Bacteroides spp., (including Bacteroides fragilis, Bacteroides distanosis, Bacteroides ovatus, Bacteroides thetaiotaomicron, Bacteroides vulgatus), Fuso bacterium spp., Veillonela spp., Prevotella (P.bivia, P.buccae, P.disiens). Indications for use: trichomoniasis in women and men: trichomonas vulvovaginitis, urethritis, bartholenitis, cervicitis, prostatitis, adnexitis, etc. - amebiasis: amoebic dysentery, extraintestinal amebiasis (including amoebic liver abscess) - giardiasis - infections caused by anaerobic bacteria: septicemia, meningitis, peritonitis, abscesses in ophthalmology - postoperative infections in coloproctology, gynecology, surgery, maxillofacial surgery: endometritis , septic abortion, suppurative processes after tooth extraction, etc. - peptic ulcer of the stomach and duodenum associated with H. Pylori - bacterial vaginosis - prevention of anaerobic infections after surgical and gynecological interventions - treatment of demodicosis in dermatology and ophthalmology. Directions for use and dosage: Tablets are taken orally after meals. In the treatment of trichomoniasis in adults, two combination therapy regimens are used. Course of treatment: 1 regimen 2 regimen Single dose 1.5 g (3 tablets) orally 1 g (2 tablets) orally + 1 vaginal tablet (Gayro) before bedtime 5 days 500 mg ( 1 tablet) in the morning and 500 mg (1 tablet) in the evening orally 500 mg (1 tablet) in the morning and 500 mg (1 tablet) in the evening orally + 1 vaginal tablet. (Gayro) before bedtime For children, the dose is set at the rate of 25 mg/kg body weight/day. For amoebic dysentery, adults and children weighing over 35 kg are prescribed 1.5 g (3 tablets) orally 1 time/day. In the evening; adults weighing more than 60 kg - 2 g/day. (2 tablets in the morning and 2 tablets in the evening). For children weighing less than 35 kg, the drug is prescribed 1 time/day at the rate of 40 mg/kg body weight. The course of treatment is 3 days. For other forms of amebiasis, adults and children over 35 kg are prescribed 500 mg orally 2 times a day. (1 tablet in the morning and 1 tablet in the evening). The course of treatment is 5-10 days. For giardiasis, adults and children weighing over 35 kg are prescribed 1.5 g (3 tablets) orally 1 time/day. in the evening for 1-2 days, or 500 mg 2 times a day. (1 tablet in the morning and 1 tablet in the evening) for 5-10 days. For children weighing less than 35 kg, the drug is prescribed 1 time/day at the rate of 40 mg/kg body weight when taken for 1-2 days. To treat infections caused by anaerobic bacteria, adults are prescribed 500 mg 2 times a day. (1 tablet in the morning and 1 tablet in the evening) for 5-10 days. The daily dose for children is set at 25 mg/kg body weight. For prophylaxis, 500 mg is prescribed before surgery and 500 mg 2 times a day after surgery for 1-5 days. Side effects - headache, dizziness - impaired consciousness, hand tremors, impaired coordination of movements - convulsions, sensory or mixed peripheral neuropathy - nausea, vomiting, diarrhea - leukopenia (with long-term treatment) Contraindications - hypersensitivity to ornidazole and other nitroimidazole derivatives - pregnancy (I trimester), lactation period - diseases of the central nervous system. Drug interactions When Gayro is used concomitantly with other 5-nitroimidazole derivatives, peripheral neuropathy, depression and epileptoform seizures may occur. Gairo does not inhibit aldehyde dehydrogenase and therefore does not interact with alcohol. Concomitant use with microsomal enzyme inducers (barbiturates, benzodiazepines, rifampicins, etc.) reduces the half-life of ornidazole in serum. Inhibitors of microsomal enzymes (cimetidine, macrolides, etc.) increase the half-life of ornidazole. Gairo enhances the effect of anticoagulants, which requires adjustment of their dose. The combination of Gayro with neurotoxic and hematotoxic drugs is not recommended. Special instructions For trichomoniasis, simultaneous treatment of the sexual partner should be carried out to avoid re-infection. Application in pediatrics. This dosage form is not used in children under 6 years of age. Pregnancy and lactation The use of the drug during pregnancy (III trimester of pregnancy) and lactation (breastfeeding) is possible only after assessing the benefits/risks. Effect of the drug on the ability to drive vehicles No effect. Overdose Symptoms: epileptiform seizures, depression, peripheral neuritis. Treatment: symptomatic (for convulsions, diazepam). Release form and packaging Tablets of 500 mg No. 1x10 in blister packaging are included together with instructions for medical use in a cardboard package. Cardboard packaging No. 10 is included together with instructions for medical use in cardboard packaging No. 10x1x10. Storage conditions Store in a dry place, protected from light, at a temperature below +30°C. Keep out of the reach of children! Shelf life: 36 months Do not use after the expiration date stated on the package. Conditions for dispensing from pharmacies By prescription Manufacturer Panacea Biotech Ltd. Malpur, Baddi, Tehsil Nalagarh District Solan (H.P.) - 173205 India
Discussion
According to the data obtained, clinical signs of bacterial vaginosis after treatment were significantly more often recorded in patients of group 2 compared with those in patients of group 1: in 4 (13.3%) and 1 (3.3%) patients, respectively . In 1 (3.3%) patient of the 2nd group, in addition, clinical signs of vulvovaginal candidiasis were identified.
Normalization of lactobacillary microflora indicators was established in 83.3% of patients in group 1, which significantly exceeded these indicators in patients in group 2 (56.7%). At the same time, the absence of representatives of the Lactobacillus
in laboratory studies, it was observed in 10 (33.3%) patients treated with Trichopolum (metronidazole), and only in 3 (10.0%) patients treated with Tiberal (ornidazole). However, the results obtained may be a consequence of the patient sample and dictate the need for further research to study the effect of drugs on the lactobacillary microflora of the vagina.
Against the background of the therapy, it was possible to achieve a decrease in the intensity of the average severity of pathological discharge (as assessed by patients) by 16.7% in patients of the 1st group, while there was no dynamics in patients of the 2nd group, the unpleasant “fishy” smell of discharge from the genital tract - by 41.2 and 5.9%, respectively, discomfort in the genital tract - by 100% in patients of the 1st group with an increase of 62.5% in patients of the 2nd group, the severity of pain during sexual intercourse - by 100% in patients of the 1st group with an increase in the indicator by 40% in patients of the 2nd group, the severity of pathological discharge according to the doctor’s assessment - by 13.0% in patients of the 1st group with no dynamics in patients of the 2nd group (Fig. 7 and 8).
Rice. 7. Dynamics of the level of severity of symptoms of the disease in patients of group 1 before and after treatment.
Rice. 8. Dynamics of the level of severity of symptoms of the disease in patients of group 2 before and after treatment.
When assessing the overall effectiveness of therapy by the patient, the following results were obtained: “marked improvement” was indicated by 29 (96.7%) patients of the 1st group and 20 (66.7%) patients of the 2nd group, “minor improvement” - 1 (3.3%) and 5 (16.7%) patients, respectively, about “condition without changes” - 3 (10.0%) patients of group 2, about “deterioration” - 2 (6.7%) patients 2nd group.
When assessing the overall effectiveness of therapy by a doctor, clinical recovery was registered in 29 (96.7%) patients of group 1 and 20 (66.7%) patients of group 2, significant improvement - in 2 (6.7%) patients 2 group, improvement - in 3 (10%) patients of group 2, condition unchanged - in 1 (3.3%) patient of group 1 and 2 (6.7%) patients of group 2, deterioration — in 3 (10.0%) patients of group 2.