Author
Petrova Evgenia Yurievna
Leading doctor
Gynecologist
until December 31
We are giving 1000 rubles for all services for a visit in December More details All promotions
Diagnostic laparoscopy
is a minimally invasive surgical operation that allows the doctor to see with his own eyes the condition of the abdominal organs. In many cases, it is necessary to confirm or correct the diagnosis. The use of diagnostic laparoscopy allows the doctor to obtain maximum information with a minimum level of surgical intervention.
Laparoscopy: what is it?
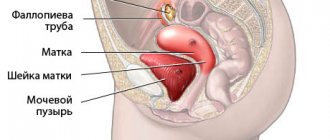
Laparoscopy is a minimally invasive surgical method for diagnosing and treating diseases of internal organs. The operation is performed using modern equipment—a laparoscope. This is an optical device in the form of a thin tube with a camera and illumination.
The camera transmits clear images in an enlarged format to the screen, and with the help of manipulators the doctor is able to perform surgical manipulations. Instruments are inserted into the abdominal wall through 3-4 small punctures.
Before the procedure, the abdominal cavity is filled with carbon dioxide. This improves visibility of internal organs and eliminates mechanical obstacles during the procedure.
The woman herself is under anesthesia during the operation and does not experience any discomfort or pain.
Laparoscopy in gynecology does not require the creation of large incisions on the body, since the doctor performs all surgical procedures using very thin instruments with a diameter, as a rule, no more than 5 mm. The procedure is quite easy for patients to understand: after the operation there are no voluminous scars left on the body - only invisible changes on the skin after punctures.
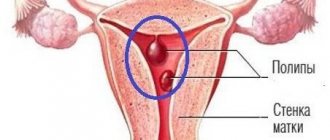
Laparoscopy for uterine fibroids
Uterine fibroids, which are quite large in size, can deform its cavity and negatively affect the condition of the mucous membrane, thereby contributing to the development of infertility. Laparoscopy allows you to remove superficial myomatous nodes, the diameter of which does not exceed 5-6 cm. As a rule, in the presence of larger uterine fibroid nodes, especially in cases where access to them is difficult, abdominal surgery (laparotomy) is required. In any case, the method of removing uterine fibroids is determined individually.
When performing a myomectomy using the laparoscopic method, the risk of developing an adhesive process is lower, however, with a large size of myomatous nodes, one must take into account the fact that it is better to suture the incisions on the uterus with direct access to it, that is, during abdominal surgery. Thus, the risk that the uterine scar will rupture is more significant than the risk of adhesions forming.
Treatment of gynecological pathologies
In addition to visual examination and taking a biopsy for research, laparoscopy is also used to eliminate pathological processes in the reproductive system. For this purpose, new hardware technologies are used: • Laser destruction, laser vaporization - the use of a laser to remove pathological areas of affected organs (the “evaporation” effect); • Electrocoagulation is a method of cauterizing pathological areas with electric current; • Radio wave method is a non-contact method of cutting and coagulating soft tissues using high frequency radio waves • Ultrasound scalpel is a device for cutting and coagulating (cauterizing) tissues using ultrasound, with minimal thermal damage to tissues.
Their use minimizes the risk of complications and accelerates healing, as well as reduces blood loss during and after surgery.
After the procedure, the punctures are sutured or taped if their diameter is less than 5 mm.
Laparoscopy for tubal obstruction
In this case, different methods can be used.
It is possible to perform salpingostomy - an operation whose purpose is to restore the patency of the fallopian tube. As a rule, it is effective for mild adhesions. However, in some cases, salpingostomy does not have a positive effect: even if the doctor manages to return the pipe to its correct anatomical shape, in the presence of chronic salpingitis the pipe is unable to function normally.
Salpingectomy (tubectomy) – removal of one or both fallopian tubes. This operation, in particular, is recommended when preparing a patient for IVF with tubo-peritoneal factor infertility in the event that attempts to restore the patency and function of the tubes are futile. If the tubes are not removed, there is a high risk of developing an ectopic pregnancy.
Indications for laparoscopy
Diagnostic laparoscopy is performed for visual examination and collection of biomaterial for examination.
Laparoscopy provides full visual and contact access to the internal organs, so it is often used for these procedures:
- Surgeries for ectopic pregnancy;
- Surgeries for ovarian cysts;
- Acute inflammatory processes in the body (tubovarial tumors, purulent tumors of the ovaries, fallopian tubes);
- Oncological (malignant) tumors of the uterine appendages (usually the ovaries);
- Correction of developmental defects of the reproductive organs;
- Research into the causes of infertility;
- Creation of artificial obstruction of the fallopian tubes for the purpose of contraception (surgical sterilization);
- Treatment of genital (external) endometriosis;
- Removal of pelvic organs (uterus, fallopian tubes, ovaries, etc.);
- Identifying the causes of pain in the lower abdomen of unknown etiology (chronic pelvic pain).
The capabilities of laparoscopy are expanding every year, which increases the scope of its application. This allows us to treat a wide range of gynecological diseases in a less traumatic way.
Preparation for diagnostic laparoscopy
Since diagnostic laparoscopy is an operation, it requires appropriate preparation. A set of studies is carried out in advance, including a general blood test, a general urinalysis, an ultrasound of the pelvic organs, an electrocardiogram, and a chest x-ray.
Before the procedure, you should abstain from food for at least 8 hours, preferably not smoking. Immediately before the operation you need to go to the toilet.
Features of the use of laparoscopy in gynecology
The frequent use of laparoscopy is due to the following features of the method:
- Low probability of adhesions
- Low invasiveness—using miniature instruments, the doctor performs the operation with minimal damage to the anterior abdominal wall
- Minimum pain - pain disappears within a day after the procedure. This is a better indicator compared to a surgical incision, when pain is observed throughout the healing period of the scar.
- Absence of postoperative scars - in the future, such formations interfere with the healthy functioning of the reproductive system and, in some cases, pregnancy.
- Quick recovery, short rehabilitation period - in some cases, the woman does not even need hospitalization in a 24-hour hospital after surgery. In just a few hours she can go home. And 2-3 weeks after treatment, the woman can return to sports.
"FIRST GYNECOLOGICAL CLINIC" conducts a comprehensive examination of the female genital organs. If indications for laparoscopy are identified, we refer the patient for the operation to the medical institution necessary for this pathology.
LAPAROSCOPY
Make an appointment for a consultation What is laparoscopy Types of operations
Dear ladies, before reading the information about the operations, we advise you to go to the Preoperative Preparation section.
Laparoscopy is a minimally invasive intervention that is performed through small punctures in the anterior abdominal wall and has significant advantages compared to traditional operations:
• there are no contraindications for laparoscopy; • there are no scars after the operation; • almost complete absence of pain; • rapid recovery after laparoscopy; • minimal risk of complications.
The operation is performed under endotracheal anesthesia using modern drugs that ensure the absence of side effects after anesthesia, so the most unpleasant moment is the installation of a dropper; all other manipulations are carried out during anesthesia sleep. After the painkillers have taken effect, three punctures about 4 mm long are made on the skin of the abdomen in the area of the umbilical ring and the lower parts of the abdominal wall on the left and right, through which an optical tube (laparoscope) with a video camera and microsurgical instruments are inserted into the abdominal cavity.
During laparoscopy, a gynecological surgeon can easily detect foci of endometriosis on the peritoneum of the pelvic cavity and ovaries, endometrioid ovarian cysts (endometriomas), endometriosis of the retrouterine space, sometimes extending to the walls of the rectum or sigmoid colon, endometriosis of the bladder and appendix, and adhesions. Laparoscopy allows you to check the patency of the fallopian tubes, remove endometrioid foci and ovarian cysts with minimal damage and preserve the so-called “ovarian” reserve,” dissect adhesions in the fallopian tubes, greatly reducing the likelihood of relapse of the disease, remove endometrioid infiltrates if neighboring organs are affected, and, if necessary, perform removal uterus (hysterectomy) if it is completely affected by endometriosis. The operation ends with thorough washing of the abdominal cavity, control of hemostasis and removal of contents, as well as the introduction of anti-adhesive gel, so the risk of adhesions is minimal. Cosmetic sutures are placed on the skin at the incision sites. The removed tissues are sent for histological examination. To create good visibility, carbon dioxide is injected into the abdominal cavity using a special device (insuflator). On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying pathology.
The operation is performed without incisions and with minimal tissue damage, so the course of the postoperative period differs significantly from traditional techniques. Recovery comes much faster. In the postoperative period after laparoscopy, the patient is active from the first day: gets up, walks.
A laparoscopic hysterectomy, or simple hysterectomy, is the removal of the entire uterus and its cervix. This operation is one of the most frequently performed in the world - more than 600 thousand operations are performed annually in the USA alone. Discharge from the hospital in uncomplicated cases is made on the second day with recommendations for rehabilitation therapy in the postoperative period. Laparoscopic hysterectomy
This operation can be performed with or without removal of appendages. If the ovaries remain, they continue to secrete hormones and no hormonal changes occur. Indications for removal of the uterus: • oncological diseases; • multiple symptomatic fibroids in combination with cervical pathology; • common endometriosis of the uterus.
The peculiarity of LAVG consists of two stages of the operation - laparoscopic and vaginal. Their combination makes it possible to carry out those stages of the operation that are impossible with the isolated use of each access. The operation is the same as the laparoscopy described above with the introduction of 3 or 4 trocars. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying pathology. Bloodlessly and carefully, the surgeon, using microsurgical instruments, dissects the adhesions, isolates from the surrounding tissues all the vessels supplying the uterus and carefully seals them with a special instrument. Large vessels, if necessary, are additionally sutured with absorbable sutures. After this, the doctor separates the uterus from surrounding tissues using special low-traumatic techniques. After the cervix is separated from the vaginal walls, the uterus is removed and removed through the vagina. The vaginal walls are sutured laparoscopically with absorbable sutures. Laparoscopically assisted vaginal hysterectomy (LAVH)
First, laparoscopy is performed according to the method described above, with the introduction of 3 or 4 trocars. The surgeon examines the abdominal organs on a monitor under cold lighting and at multiple magnifications. The doctor clarifies and adjusts the planned scope of the operation, and then proceeds to the laparoscopic stage of hysterectomy.
Laparoscopic supracervical hysterectomy is the removal of the body of the uterus without the cervix. If the appendages are not removed during the operation, the ovaries will continue to secrete hormones, that is, hormonal changes will not follow. Indications for removal of the uterine body: • multiple symptomatic fibroids without cervical pathologies; • submucosal fibroids, the size of which exceeds 5 cm; • bilateral benign ovarian tumors in premenopause. Laparoscopy is performed as described above. On the monitor screen, the surgeon examines the abdominal and pelvic organs, accurately identifying pathology. Bloodlessly and carefully, the surgeon, using microsurgical instruments, dissects the adhesions, isolates from the surrounding tissues all the vessels supplying the uterus and carefully seals each vessel with a special instrument. Large vessels, if necessary, are additionally sutured with absorbable sutures. After this, the doctor separates the uterus from surrounding tissues using special low-traumatic techniques. The uterus is removed without the cervix, crushed using a special device (marcellator) and removed from the abdominal cavity. The cervical stump is sutured with absorbable threads. Cosmetic sutures are placed on the skin at the incision sites. The removed uterus is sent for histological examination. Bloodlessly and carefully, the surgeon uses microsurgical instruments to cut through adhesions and remove foci of endometriosis. Then the gynecologist surgeon carefully coagulates and crosses the blood vessels supplying the uterus with a special instrument. The doctor then cuts the ligaments that support the uterus. The next stage of the operation is carried out through the vagina. After dissecting the walls of the vagina, the surgeon sutures the large vessels supplying the uterus, separates it from the surrounding tissues, removes it and removes it from the abdominal cavity through the vagina. The vagina is sutured with absorbable sutures. If necessary, vaginal plastic surgery can be performed. The operation ends with laparoscopic peritonization of the wound. Cosmetic stitches are placed on the skin at the puncture sites. The removed organ is sent for histological examination. Laparoscopic supracervical hysterectomy (supravaginal uterine amputation)
Laparoscopic sacrogamopexy or promontofixation (sacrocolpopexy) is a modern operation that is considered the “gold standard” for the surgical treatment of pelvic organ prolapse throughout the world. The purpose of the operation is to replace damaged ligaments that support the uterus with an artificial ligamentous apparatus in the form of a special, thin elastic mesh that fixes the uterus and vagina in the correct anatomical position. The advantage of this technique is the Method of execution: Laparoscopy is performed with the introduction of 3 trocars in typical places according to the method described above. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying the condition of the fallopian tubes and their pathologies. After this, the gynecologist surgeon begins the stage of removing the pathologically altered fallopian tube. The fallopian tube is fixed with atraumatic clamps and, after coagulation of the vessels, is bloodlessly intersected in the isthmic region. Then, after crossing the mesosalpinx, the tube is removed from the abdominal cavity in a special container. Indications for sacrovaginopexy: · prolapse, incomplete and complete prolapse of the vagina and uterus; · cystocele; · rectocele. The operation is the same as the laparoscopy described above with the introduction of 3 or 4 trocars. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying defective areas of prolapse. Bloodlessly and carefully, the surgeon, using microsurgical instruments, separates the uterus from the walls of the bladder and rectum and restores the natural position of the organs. Then the gynecologist surgeon sews two sheets of thin polypropylene mesh to the walls of the vagina, ligaments and muscles of the pelvic floor, which are then fixed together to the ligament of the promontory of the sacral bone. The mesh cavities will soon be covered with connective tissue, which will ensure a strong ligament of organs. The operation ends with laparoscopic peritonization of the wound. Cosmetic stitches are placed on the skin at the puncture sites. Sacrovaginopexy
Despite the fact that total hysterectomy is a radical operation, it is not recommended for young women or those who wish to preserve the uterus and reproductive function. We widely carry out such organ-preserving operations, regardless of age. Indications for myomectomy may include infertility and miscarriage with uterine fibroids as the only cause. Conservative myomectomy can be performed either by laparotomy, that is, through an incision in the anterior abdominal wall, or by laparoscopic method. The approach to myomectomy depends on the number, size and location of myomatous nodes. Regardless of the chosen method, a prerequisite for performing this operation is layer-by-layer suturing of the uterus after removal of the nodes. Especially if pregnancy and childbirth are planned in the future. Conservative myomectomy Laparoscopic conservative myomectomy
First, laparoscopy is performed with the introduction of 3 or 4 trocars according to the method described above. A gynecological surgeon examines the organs of the abdominal region on a monitor under cold lighting and multiple magnification, accurately identifying the pathology. Bloodlessly and carefully, the surgeon makes an incision in the uterine wall in the projection of the myomatous node, after which he carefully isolates the node from the surrounding tissues, suturing the blood vessels. The incision on the uterus is sutured in layers with absorbable threads. Today, absorbable Swiss thread with V-loc notches is widely used for suturing the uterus. It allows you to connect the edges of the wound on the uterus without tying knots. The removed node is crushed using a special marcellator device and removed from the abdominal cavity. The operation ends with thorough washing of the abdominal cavity, control of hemostasis and removal of contents, and the introduction of anti-adhesion gel. These measures minimize the risk of adhesions. Cosmetic sutures are placed on the skin at the incision sites. The removed tissues are sent for histological examination. REHABILITATION In the postoperative period after conservative myomectomy, the patient is active from the first day - gets up, walks. Discharge from the hospital in uncomplicated cases is made on the second day with recommendations for rehabilitation therapy in the postoperative period. Salpingotomy is a section of the fallopian tube. The main indication for salpingotomy is surgical treatment of ectopic pregnancy without removal of the fallopian tube. Laparoscopic salpingotomy
Laparoscopic salpingectomy or tubectomy is a radical operation to remove the fallopian tube. The main indications for laparoscopic salpingectomy: • ectopic pregnancy with the inability to perform organ-preserving surgery; • chronic salpingitis with the formation of hydrosalpinx or sactosalpinx. First, laparoscopy is performed using the method described above. On a monitor screen in cold light under magnification, a gynecologist surgeon examines the abdominal and pelvic organs. The doctor diagnoses the location of the ectopic pregnancy and the condition of the second fallopian tube, determining the optimal scope of surgical intervention. The gynecologist surgeon, having made sure that there are no contraindications for the operation, bloodlessly and extremely carefully, using microsurgical instruments, makes a small longitudinal mini-incision in the wall of the fallopian tube. Using an irrigator, a flow of liquid under pressure separates the fertilized egg from the wall of the tube and removes it from the abdominal cavity. The incision in the area of the pipe wall is not sutured and heals well on its own, without subsequently deforming the lumen of the pipe. The operation ends with thorough washing of the abdominal cavity and removal of the contents. Anti-adhesion gel is applied to the uterus and appendages. Cosmetic sutures are placed on the skin at the incision sites. REHABILITATION In the postoperative period after salpingotomy, from the first day the patient is active - gets up, walks. Discharge from the hospital in uncomplicated cases is made on the second day with recommendations for rehabilitation therapy in the postoperative period. Planning a pregnancy after the operation is possible next month. Laparoscopic salpingectomy Laparoscopy is performed with the introduction of 3 trocars in typical places according to the method described above. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying the condition of the fallopian tubes and their pathologies. After this, the gynecologist surgeon begins the stage of removing the pathologically altered fallopian tube. Execution method:
This is a minimally invasive operation to remove the appendages, during which the ovaries and tubes are cut off on one or both sides. An adnexectomy can be a separate operation or performed during a hysterectomy. Indications for laparoscopic adnexectomy: • tumor-like formations of the ovaries; • pronounced inflammatory changes in the appendages with the formation of inflammatory tumors; • age over 45 years when performing hysterectomy. Laparoscopy is performed with the introduction of 3 trocars in typical places according to the method described above. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying the pathology and condition of the fallopian tubes. Then the gynecologist-surgeon begins the stage of removing the pathologically altered uterine appendages. REHABILITATION In the postoperative period after salpingectomy, the patient is active from the first day - gets up, walks. Discharge from the hospital in uncomplicated cases is made on the first or second day with recommendations for rehabilitation therapy in the postoperative period. Laparoscopic adnexectomy The fallopian tube is fixed with atraumatic clamps and, after coagulation of the vessels, is bloodlessly intersected in the isthmic region. Then, after crossing the mesosalpinx, the tube is removed from the abdominal cavity in a special container.
Laparoscopy is performed with the introduction of 3 trocars in typical places according to the method described above. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying the pathology and condition of the fallopian tubes. Then the gynecologist-surgeon begins the stage of removing the pathologically altered uterine appendages. The ovary and fallopian tube are fixed with atraumatic clamps and, after coagulation of the vessels, are bloodlessly separated from the uterus and surrounding tissues. The proper and infundibulopelvic ligaments of the ovary, the isthmic section of the tube and the mesosalpinx are intersected. The appendages are removed from the abdominal cavity in a special container, after which they are sent for histological examination. Laparoscopic coagulation of endometrioid lesions is the removal of small forms of endometriosis discovered during laparoscopy with further histological examination. Removal is performed using a laser, radio wave or argoplasma coagulator. Laparoscopic coagulation of endometriotic lesions
Laparoscopic removal of endometrioid cysts and benign ovarian tumors
Laparoscopy is performed with the introduction of 3 trocars according to the method described above. On the monitor screen under cold lighting under magnification, the surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying pathology. After eliminating signs of a malignant process, the doctor proceeds to the stage of removing the cyst or benign tumor. Bloodlessly and extremely carefully, using microsurgical scissors and an electric knife, the surgeon removes the cyst capsule from the surrounding ovarian tissue, preserving the functional ovarian tissue as much as possible. This is especially important in patients with unrealized reproductive function and reduced ovarian reserve. The cyst bed is sutured laparoscopically with absorbable atraumatic threads. The cyst capsule in a container is ablastically removed from the abdominal cavity. The operation ends with thorough washing of the abdominal cavity, control of hemostasis and removal of contents, so the risk of adhesions is minimal. Cosmetic sutures are placed on the skin at the incision sites. You can learn about the indications for surgery in these articles (Endometriosis, Cysts and benign ovarian tumors). Laparoscopic removal of paraovarian cyst
Laparoscopy is performed with the introduction of 3 trocars according to the method described above. On a monitor screen under cold lighting under magnification, a gynecologist surgeon examines the abdominal and pelvic organs, accurately identifying pathology. After excluding signs of a malignant process, the stage of removal of the paraovarian cyst begins. Bloodlessly and extremely carefully, with the help of microsurgical scissors and an electric knife, the mesosalpinx leaf is dissected, the cyst is isolated from the surrounding tissues, it is removed and extracted from the abdominal wall. Negative effects on the tube and ovary are completely excluded during this operation. You can find out about the indications for surgery in this article (Ovarian Cysts). The main indication for laparoscopic surgery to restore the patency of the fallopian tubes is the tubo-peritoneal factor of infertility. The operations are performed laparoscopically using modern, low-traumatic instruments. These operations include: • salpingolysis (freeing the fallopian tubes from adhesions that deform them); • fimbryoplasty (restoration of the entrance to the funnel of the fallopian tube); • salpingostomy (creation of a new hole in the ampullary section of the fallopian tube closed by adhesions); Laparoscopic operations to restore patency of the fallopian tubes
Dentistry
The main indication for laparoscopic surgery to restore the patency of the fallopian tubes is the tubo-peritoneal factor of infertility. The operations are performed laparoscopically using modern, low-traumatic instruments. These operations include: • salpingolysis (freeing the fallopian tubes from adhesions that deform them); • fimbryoplasty (restoration of the entrance to the funnel of the fallopian tube); • salpingostomy (creation of a new hole in the ampullary section of the fallopian tube closed by adhesions); Adhesions are the result of the body’s attempt to protect itself from the spread of infection. The reasons for the formation of adhesions in the uterus are previous inflammatory processes, intestinal diseases in the area of the uterus and appendages. Involving neighboring organs in the process, adhesions lead to deformation of the fallopian tube - the egg cannot move normally through the fallopian tube, which often leads to the impossibility of conception. Salpingolysis can be both the main stage in the treatment of tubo-peritoneal factor of infertility, and it can precede another type of surgical intervention - tubal plastic surgery (stomatoplasty) after checking the patency of the fallopian tubes - hydrosalpingoscopy - during diagnostic laparoscopy. Indications for salpingo-ovariolysis are pronounced adhesions, obstruction of the fallopian tubes, and tubo-peritoneal infertility. Salpingo-ovariolysis
Salpingo-ovariolysis
Laparoscopic oophorectomy is the removal of the ovary. Most often, the ovary is removed in the presence of pathology during the menopausal period. Indications for oophorectomy: • tumors and tumor-like formations of the ovary; • pronounced inflammatory process of the ovary with the formation of an abscess. The operation is performed under general anesthesia using modern drugs that ensure the absence of side effects after anesthesia. The patient is placed on the operating table in the form of a gynecological chair. After the painkillers have taken effect, the gynecologist inserts a manipulator probe into the uterine cavity, which allows you to check the patency of the fallopian tubes during the operation. Three punctures about 4 mm long are made in the area of the umbilical ring and lower abdomen on both sides, through which a laparoscope with a video camera and microsurgical instruments are inserted. Carbon dioxide is injected into the abdominal cavity using a special device (insuflator) to visualize the abdominal cavity. On a monitor screen under cold lighting and multiple magnification, a gynecologist surgeon examines the abdominal and pelvic organs, accurately identifying pathology. A sterile solution is injected into the uterine cavity and the patency of the fallopian tubes is visually assessed. Bloodlessly and as carefully as possible, using atraumatic instruments, the surgeon dissects the adhesions between the fallopian tubes and ovaries (salpingo-ovariolysis), in the area of the fimbrial sections of the tubes (fimbryolysis). Then the doctor carefully coagulates the bleeding vessels and monitors the patency of the fallopian tubes. If the fallopian tubes are impassable in the area of the ampullary sections, stomatoplasty (neostomatoplasty) is performed - restoring the patency of the fallopian tube due to a newly formed stoma (an artificially created opening in the ampullary section of the tube). The operation ends with thorough washing of the abdominal cavity and removal of the contents. If necessary, an anti-adhesion gel is injected into the appendage area. Cosmetic sutures are placed on the skin at the incision sites. REHABILITATION In the postoperative period after salpingolysis, from the first day the patient gets up and walks. Discharge from the hospital in uncomplicated cases is made on the second day with recommendations for rehabilitation therapy in the postoperative period. Planning a pregnancy is usually possible in the near future after surgery. Laparoscopic oophorectomy
Laparoscopy is performed with the introduction of 3 trocars according to the above method. On the monitor screen under cold lighting under magnification, the surgeon examines the abdominal and pelvic organs and accurately identifies pathology. After examining the organs and excluding signs of a malignant process, the doctor proceeds to the stage of removing the ovary. Bloodlessly and extremely carefully, using microsurgical scissors and an electric knife, the native ovarian ligament and infundibulopelvic ligament are dissected, removed and removed from the abdominal wall of the ovary in a special container.
Drilling or diathermopuncture (diathermocautery) of the ovaries is a technique by which several incisions are made on the lining of the ovary. In the future, the notches will allow the follicles to “break through” the dense membrane of the ovary, and the egg will be able to be fertilized. The main indication for ovarian drilling is polycystic ovary syndrome (PCOS), you can learn more about it here (Infertility). Laparoscopy is performed with the introduction of 3 trocars in typical places according to the method described above. On the monitor screen, a gynecological surgeon examines the organs of the abdominal cavity and pelvis, accurately identifying pathology. Bloodlessly and as carefully as possible, using atraumatic instruments, the ovaries are fixed one by one, after which several small incisions are made on each using a radiofrequency scalpel. The operation ends with thorough washing of the abdominal cavity and removal of the contents. Cosmetic sutures are placed on the skin at the incision sites. REHABILITATION In the postoperative period after removal of the ovary, already from the first day the patient gets up and walks. Discharge from the hospital in uncomplicated cases is made on the first or second day with recommendations for rehabilitation therapy in the postoperative period. Laparoscopic ovarian drilling
Process
Before diagnostic laparoscopy, a comprehensive examination of the patient is performed by the attending physician and anesthesiologist.
Stages of preparation for surgery:
- Connecting the patient to an IV and a monitor that monitors the heart.
- The use of general anesthesia, intravenous or combined with endotracheal.
- Administration of drugs intravenously to completely relax the body.
- Insertion of an endotracheal tube and further connection to a ventilator.
The surgical intervention itself is carried out in the following sequence:
- The Veress needle enters the cavity, after which carbon dioxide or nitrous oxide penetrates into the space.
- Insertion of hollow tubes, the needle is removed.
- Dissection of skin tissue and puncture with a trocar.
- After removing the trocar, the laparoscope is inserted.
- Removal of found formations/suppurations, biopsy. This stage may be skipped in the case of pure diagnosis or detection of a cancerous tumor.
- Removing instruments from the cavity.
Positions of the operated patient during diagnostic laparoscopy:
- raised pelvis above the upper body;
- the torso is raised above the pelvis;
- on the side.
Possible complications
The laparoscopy technique is extremely complex; it requires an experienced specialist with well-developed skills. Adverse consequences may occur due to incorrect insertion of trocars. In this case, there may be injuries to internal organs such as the intestines, bladder, ureters, and blood vessels. Most of these complications are resolved immediately during surgery; sutures are placed on the affected organs. If organ injuries cannot be eliminated by laparoscopy, the doctor is forced to perform a laparotomy - opening the anterior wall of the abdomen.
Improper preparation of the patient increases the risk of negative consequences. Thus, a full bladder is very often damaged when instruments are inserted. In this case, in addition to the main operation, the patient is urgently given two rows of sutures on the affected organ. If the patient took medications before the procedure and did not warn the doctor about this, the composition of these drugs can unpredictably affect anesthesia. In some cases, the invasion has to be completed urgently. However, such consequences occur with any surgical intervention.
With laparoscopy, the risk of infection, suture dehiscence, and adhesions is significantly lower.
4.Risks and well-being after surgery
Risks of laparoscopy
Today, laparoscopy is a well-studied and proven surgical procedure. And the likelihood of any problems arising is very small. However, as with any surgery, there are always risks.
During laparoscopy, there is a possibility of such problems
How:
- Bleeding from incisions;
- Infections;
- Damage to an organ or blood vessel. This may lead to more bleeding and another operation will be needed.
Laparoscopy cannot be done due to the high likelihood of complications if you:
- Abdominal tumor.
- Abdominal hernia.
- Have had abdominal surgeries in the past.
Recommendations after the procedure
Rest is recommended in the first few hours after the infestation. The duration of bed rest depends on the degree of complexity of the operation, the presence of complications, and the patient’s condition. The attending physician will determine the time of the rehabilitation period and the date of discharge and give recommendations. At home, it is important to fully follow your doctor’s advice. Recommendations may include nutritional rules, if laparoscopy was performed on the gastrointestinal tract, in which case you will have to follow one of the Pevzner diets for 2 weeks. Within a month after the invasion, regardless of its type and purpose, alcohol, too fatty and spicy foods, spicy, and canned foods are excluded.
Personal hygiene is very important. You can swim in the shower, take baths only after 14 days. After each exercise, you need antiseptic treatment of the sutures and a dressing or bandage. For wound treatment it is allowed to use:
- hydrogen peroxide 3%;
- fucorcin;
- alcohol solution of brilliant green.
The sutures are removed on the day determined by the doctor, usually after 7-14 days. This should only be done by a health worker in the dressing room. In the first month after the procedure, you need to limit physical activity, exclude sports and heavy lifting. Leisurely strolls are allowed. You should also abstain from sex for the first 14-30 days, depending on the illness. After examination by a doctor and with his permission, you can return to your normal lifestyle.
If during the rehabilitation period frequent abdominal pain appears, consciousness becomes confused, vomiting occurs, and bowel movements are disrupted, you should inform your doctor about this. It is also important to monitor the condition of the stitches; there should be no swelling, redness, itching, or any discharge.
Endoscopic surgery at GUTA CLINIC
Since 2001, GUTA CLINIC has its own surgical hospital, in which more than 90% of operations are performed using endoscopic techniques without incisions and the need for sutures.
Thanks to the use of endoscopic techniques
the average time a patient stays in hospital is no more than one and a half days, which is 5 times shorter than the standard time of stay after abdominal surgery.
Spectrum of endoscopic operations
performed in the surgical department of GUTA CLINIC is enormous:
- General surgery.
- Urology.
- Traumatology and orthopedics.
- Phlebology.
- Gynecology.
- Otorhinolaryngology.
- Proctology, etc.
In our work, we managed to combine the latest medical technologies, modern design and customer-oriented service. Experienced surgeons at GUTA CLINIC have undergone training in leading clinics in Europe and the USA.
Thanks to the use of ultrasound diagnostics (ultrasound) and surgical laser techniques during surgery, we achieve the highest efficiency and quality of treatment that meets the most stringent international standards.
Possible consequences
The likelihood of complications with minimally invasive interventions is extremely low - 1-3 per 1000 cases. The risk group consists of women with a high body mass index, concomitant diseases, and a history of surgery on the pelvic organs.
Most often, intervention leads to the following consequences:
- allergic reaction to painkillers;
- re-development of the underlying disease;
- damage to nearby organs;
- bleeding;
- thromboembolism.
During the recovery period, infection and poor healing of wounds, divergence of postoperative sutures are possible. To minimize the likelihood of complications, you need to strictly follow your doctor’s recommendations. In Moscow, in paid clinics, such a minimally invasive intervention for diagnostic purposes can be done for 40,000 - 60,000 rubles. As complexity increases, the cost increases.
3.Feelings during laparoscopy
With general anesthesia, you will sleep and not feel anything. After your laparoscopy and when you wake up, you will feel sleepy for several hours. You may experience fatigue and some pain for a few days after laparoscopy. You may have a slight sore throat from the breathing tube. Use lozenges and gargle with warm salt water.
With other types of anesthesia, slight pain may occur for several days.
About our clinic Chistye Prudy metro station Medintercom page!