Hydatidiform mole (MH) is a fatal disease for the fetus concerning the pathological development of the fetal egg and associated with the transformation of the chorion into cysts (protective membranes formed due to unfavorable conditions in certain life cycles, in the form of bubbles containing fluid) and the proliferation of the villi epithelium outer germinal membrane.
This pathological condition is accompanied by the following negative manifestations:
- bleeding;
- early toxicosis;
- enlargement of the uterus relative to the gestational age of the fetus.
PZ is diagnosed using a vaginal examination, ultrasound, fetal phonocardiography, and determination of the content of human chorionic gonadotropin (β-hCG).
Treatment includes techniques such as vacuum aspiration, curettage of the uterine cavity, and removal of the organ (hysterectomy).
What is a hydatidiform mole?
Hydatidiform mole is a pathology that is characterized by modification of the membrane tissue (chorionic hyperplasia) into peculiar cysts. These are cavities, bubbles filled with liquid contents. Next, the growth of such chorionic villi occurs, which is accompanied by the death of the embryo developing in utero.
This pathology belongs to trophoblastic diseases. The incidence of such a diagnosis is about 0.5%. Characteristic features of the pathological condition are swelling and a sharp proliferation of villi tissue, the formation of bubble-like formations. In its form, this process resembles a bunch of grapes. The size of these bubbles is quite impressive. Can be about 2-2.5 centimeters in diameter. There is practically no blood flow in such bubbles.
Laboratory research
To confirm the diagnosis, a woman submits:
- blood for hCG, the level of which is significantly increased in PZ;
- analysis of thyroid hormones, the function of which is disrupted when pregnancy has developed;
- blood chemistry. With this disease, the functioning of the liver and kidneys is disrupted, the level of creatinine, residual nitrogen, proteins, urea, bilirubin, transaminases, and alkaline phosphatase changes.
A transvaginal ultrasound of the uterus is required.
Reasons for the development of the anomaly
There are several reasons for the formation of such a pathological condition as hydatidiform mole:
- Chromosomal abnormalities resulting from the prenatal period. With the complete variant of the pathology, there is a complete loss of maternal genetic material. The same situation can arise when two male reproductive cells fertilize an inferior egg without a nucleus.
- Viral or bacterial infection of the chorionic villi, leading to the above changes.
- Multiparous women, as well as young primigravidas, are at risk of developing the process.
- Immunodeficiency states.
- Thyrotoxicosis.
Types of hydatidiform mole
- Complete hydatidiform mole is a condition in which all chorionic villi are subject to pathological changes in the form of stromal edema, trophoblast hypertrophy and the formation of vesicles, while the signs of a developing embryo are completely absent. All tissue is affected. This pathology is most often detected at 10-12 weeks of gestation. Such a hydatidiform mole contains a diploid number of chromosomes: 46 XX. It is worth saying that all chromosomes are paternal. There may be a karyotype of 46 XY, however, both X and Y are also paternal. The danger of this pathology is that in twenty percent of cases this process can become malignant with the formation of many metastases.
- Partial hydatidiform mole is characterized by the presence of some intact tissue. Intact parts of the embryo and placenta may be identified. The chromosome set is defined as 69 XXX, 69 XXX. The set contains 1 maternal chromosome. The frequency of transition to a malignant form of the process is about five percent.
- Invasive hydatidiform mole. This pathology is a process in which chorion grows into the myometrium of the uterus. This is a severe pathology that can lead to massive bleeding during removal of hydatidiform mole tissue.
According to histological structure, pathology is also divided into:
- Syncytial type;
- Cytotrophoblastic;
- Mixed form of hydatidiform mole.
Forecast
Complete cure is possible in most cases. Only 1% of women may experience a recurrence of the disease in the future. After a second molar pregnancy, the risk of developing a third is much higher - up to 15-20%.
In rare cases, benign neoplasms become malignant. But even with this option, chemotherapy leads to complete recovery in 90% of women.
Emotional complications
Termination of pregnancy is a difficult experience. The desire to grieve and cry is completely natural and should not be suppressed. A frank conversation with loved ones is sometimes necessary to further restore mental strength. The child's father may also experience the loss very painfully. Each parent should not close themselves off, but share their feelings with each other and try to overcome difficulties together. If the period of despondency drags on, you should consult a psychologist. All fears and concerns about future pregnancies, if any are planned, should be discussed with your gynecologist. Almost all women respond well to treatment. And the next pregnancy can be interrupted by a hydatidiform mole with a very low probability.
Symptoms
There are several signs for the clinical picture of hydatidiform mole:
- Dark bloody discharge from the genital tract, which contains bubbles rejected from the site of hydatidiform mole. The volume of such bleeding can vary significantly, ranging from spotting to massive bleeding.
- If the bleeding is large or prolonged, the woman may develop anemia. Its symptoms include weakness, fatigue, pale skin, rapid heartbeat, and sometimes episodes of loss of consciousness.
- In the invasive form of this pathology, when chorionic villi grow into the wall of the uterus (myometrium), pain in the lower abdomen may occur. When a perforation of the uterine wall occurs, massive bleeding into the abdominal cavity may occur, which is accompanied by acute abdominal pain and loss of consciousness.
- The size of the uterus is not commensurate with gestational age. When such a pathological condition develops, the uterus is larger than the period calculated from the first day of the last menstruation.
- Toxicosis during hydatidiform mole is often several times more pronounced. Symptoms quickly increase, nausea and vomiting are debilitating, and liver and kidney failure may occur. This quickly leads a woman to a moderate or even severe state.
Where to get checked during pregnancy in St. Petersburg
To maintain your health and not lose the opportunity to have children in the future, you need to be vigilant. During pregnancy, which causes terrible early toxicosis and a rapid increase in the size of the abdomen, you need to visit a gynecologist and do an ultrasound.
You can undergo an expert examination inexpensively in St. Petersburg at the Diana gynecological clinic. The examination will not cost much, for example, an expert pelvic ultrasound using a new machine with Doppler costs only 1,000 rubles.
Diagnostics
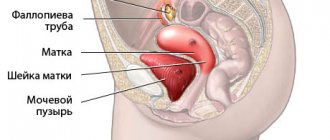
Gynecological examination.
- When examined in the doctor's chair, you should be alert to the uterus, which is revealed to be much larger in size than the expected gestational age based on the date of the last menstruation.
- Dense consistency of the uterus with areas of strong softening.
- Bloody discharge from the genital tract with blisters.
Ultrasound examination, which is the most informative method for diagnosing this pathological condition. Ultrasound signs of hydatidiform mole include:
- Increased size of the uterus, which does not correspond to the timing of menstruation;
- The presence of a fine-grained tissue structure in the uterine cavity, reminiscent of a “blizzard”. This is a characteristic sign of a hydatidiform mole. This ultrasound picture is also sometimes called a “bunch of grapes”.
- A frequent occurrence during ultrasound diagnosis of the uterine appendages with such pathology is the presence of thecal lutein cysts.
- Blood sampling to determine hCG levels. Indeed, with hydatidiform mole, its level may exceed the borderline norms.
- If there is a suspicion of metastasis of a hydatidiform mole, a computed tomography or MRI is prescribed.
Trophoblastic disease
Trophoblastic disease
is a group of benign and malignant neoplasms originating from elements of the placenta. Trophoblastic disease is relatively rare. Thus, per 1000 births there is 1 observation of hydatidiform mole, per 100,000 births or abortions there are 2 cases of choriocarcinoma.
According to the International Classification of Diseases of Oncology (1995), trophoblastic disease includes: hydatidiform mole (complete or partial), invasive hydatidiform mole, choriocarcinoma or chorionepithelioma, choriocarcinoma in combination with teratoma or embryonal cancer, malignant trophoblastic teratoma and trophoblastic tumor of the placental site.
Among the causes of trophoblastic disease, the viral theory, immunological theory, enzymatic theory, and protein deficiency are considered.
Risk factors for the occurrence of trophoblastic disease are: the age of patients over 40 years old (the risk of the disease is 5 times higher than for women aged 21 to 35 years); a history of early spontaneous abortions; the likelihood of the disease is higher in multipregnant women; the disease is more common in Eastern countries compared to Western countries.
Hydatidiform mole
Hydatidiform mole is a pathologically altered villous chorion in the form of many bubbles of various sizes, filled with clear liquid, which completely (complete mole) or partially (partial mole) replace placental tissue. These vesicles are increased in volume due to pronounced swelling of the chorionic villi with the formation of cavities containing mucus-like fluid in the central sections of some of these villi. Elements of a hydatidiform mole can be freely located in the uterine cavity and be associated with its wall.
Complete hydatidiform mole is observed in the first trimester of pregnancy, and the embryos die in such cases. With a partial hydatidiform mole, pregnancy can progress until delivery of a viable fetus, however, more often, fetal death occurs at 14-16 weeks, or premature birth occurs with fetal death in the ante- or intrapartum period. Fragments of vesicular villi, independently or when removing a mole from the uterine cavity, can enter the venous bed and reach the pulmonary vessels, causing acute pulmonary hypertension, pulmonary edema and even death of the pregnant woman. The most severe outcome is the development of choriocarcinoma from the remnants of a hydatidiform mole in 3.8-5% of cases. A rare variant of hydatidiform mole (frequency 5-6%) is invasive hydatidiform mole.
There are several risk factors that serve as a background for the transition of hydatidiform mole to choriocarcinoma: age over 40 years; discrepancy between the size of the uterus (enlargement) and the duration of pregnancy; presence of ovarian luteal cysts; persistent increase in the level of human chorionic gonadotropin, which does not decrease after removal of the hydatidiform mole.
The risk of malignant degeneration of hydatidiform mole increases in those patients who have three or more of these signs. In such patients, as well as with recurrent hydatidiform mole, progression of the disease is observed in half of the cases, and in the presence of less than three signs - in a third.
Chorionic carcinoma or chorionepithelioma
Chorionic carcinoma (synonym - chorionepithelioma) is a malignant form of trophoblastic disease that arises from the chorionic epithelium after hydatidiform mole (up to 40% of cases), after a normal abortion (25%) or after childbirth (22.5%). Isolated cases of simultaneous development of chorionic carcinoma and hydatidiform mole have been described. It is rare and is not always associated with a previous pregnancy, terminated at different times, or with a hydatidiform mole. Chorionic carcinoma that occurs outside of pregnancy is classified as a teratogenic tumor. Often there is not one tumor node, but two or more. The sizes of tumor nodes vary - from a few millimeters to the head of an adult. Most often, chorionic carcinoma is located in the body of the uterus (in the area of implantation of the fertilized egg). May also be located near the uterine openings of the tubes. Choriocarcinoma of the ovaries and fallopian tubes is rare - 1-4%. It is possible to develop chorionic carcinoma from ectopic pregnancy (2.5%). Growing into the body of the uterus, tumor masses can penetrate into the pelvis without causing clinical manifestations of compression of surrounding tissues, vessels and nerve trunks, but causing mild pain.
Choriocarcinoma is rare during pregnancy. More often it appears during 4-6 month pregnancy, less often during full-term pregnancy. Chorionic carcinoma during pregnancy usually leads to metastatic damage to various organs. When chorionepithelioma occurs during pregnancy, it is difficult to recognize the neoplasm even in situations where the process has taken a widespread form. The disease may not produce any symptoms for a long time and has a poor prognosis. The interval between the end of pregnancy and the first manifestation of this form of trophoblastic disease varies widely. The duration of the latent period is usually 6-12 months, more often - 3 months. There are cases of a very long latent period - 10 - 20 years.
It should be noted that there is not a single symptom that is specific only to chorionic carcinoma. More or less clear clinical symptoms are observed only if the primary node of chorionic carcinoma is located in the uterus and communicates with its cavity. The predominant symptom in patients with trophoblastic disease is bleeding from the genital tract of various types. In many cases, this symptom is also the first manifestation of the disease. Bleeding may not stop after the first curettage and requires repeated manipulation. Recurrence of bleeding, as well as the need for repeated curettage, is typical for patients with trophoblastic disease. The timing of the onset of bleeding in relation to the outcome of a previous pregnancy or menstruation also varies. The different nature of bleeding and the time of its onset is explained by the different location of tumor nodes (chorionic carcinoma) in the uterine cavity.
Along with bloody discharge or in the intervals between them, in many patients one can also observe other discharges of different nature: serous, purulent, sometimes with an unpleasant odor, which is associated with necrotization, decay and infection of tumor nodes. Prolonged, repeated bleeding, often accompanied by significant blood loss, as well as intoxication of the body by decay products of tumor masses, often lead to anemia in the patient, sometimes with a significant decrease in hemoglobin.
Signs of trophoblastic disease
One of the signs of trophoblastic disease is a discrepancy between the size of the uterus and the expected gestational age. More often, the size of the uterus is greater than the expected gestational age, in 20% it corresponds to the gestational age, and in 16% it is less than the gestational age. An important sign of trophoblastic disease is the formation of ovarian luteal cysts (50% of cases). In most patients with luteal cysts, they are bilateral, reach large sizes, and fill the entire pelvis. With hydatidiform mole, luteal cysts may appear within the first two weeks. Their presence is an unfavorable prognostic sign. Regression of luteal cysts is possible within 3 months after removal of a hydatidiform mole. The pain felt by the patient in the lower abdomen and lower back is explained by the presence of tumor masses in the uterine cavity, especially when the last germination of the uterine walls reaches the serous layer.
In some cases, pain occurs due to the location of metastatic tumor masses in the parametrium and their compression of the nerve trunks. The presence of acute paroxysmal abdominal pain can be explained by perforation of the uterus or, in some patients, torsion or perforation of luteal cysts. Pain can also be caused by the localization of chorionic carcinoma metastases in various organs of the abdominal cavity: pain in the chest area is a consequence of pulmonary metastases, headaches are a consequence of metastases in the brain, etc.
There may be clinical symptoms associated with the metastasis process: symptom complex of intestinal obstruction, intestinal bleeding, cough with bloody sputum, paresis, cachexia, etc. The course of trophoblastic disease is characterized by early and intense metastasis, especially with chorionic carcinoma. In some cases, the disease is first diagnosed based on the detection of metastases. The sites most commonly affected by metastases from trophoblastic tumors, mainly chorionic carcinomas, are the lungs, vagina, and brain. Less commonly, the liver, kidneys, spleen, and small intestine are affected.
Diagnosis of trophoblastic disease
In diagnosing the disease, great importance is attached to the correct collection of anamnesis, taking into account the patient’s complaints and gynecological examination. However, based on these data, trophoblastic disease can only be suspected. It is impossible to accurately determine the nature of a trophoblastic tumor even if metastases are detected in the vagina or cervix. To clarify the diagnosis, ultrasound is used. In some women with partial hydatidiform mole, an image of the fetus can be identified. Ultrasound diagnosis of partial hydatidiform mole is difficult, especially with a small amount of degenerative changes in the chorion. With careful examination, luteal cysts can be visualized, usually bilateral, multi- or single-chamber, located on the side of the uterus. Characteristic ultrasound criteria for hydatidiform mole are more often detected after 12 weeks of pregnancy. In earlier stages, echographic signs of the disease are not informative enough.
For a more reliable diagnosis, it is advisable to use color Doppler mapping, which makes it possible to identify tumor nodes even when conventional ultrasound cannot clearly visualize the contours of the pathological focus in the structure of the myometrium. Color Doppler mapping makes it possible to assess the state of the vascular bed in trophoblastic tumors of the uterus, as well as the effectiveness of the therapy. Clear visualization of the tumor focus in the thickness of the myometrium can significantly reduce the number of unnecessary repeated diagnostic curettages of the uterus. To diagnose the disease, instrumental research methods are also used: X-ray examination, hysteroscopy, pelvic angiography (indicated for patients with suspected chorionic carcinoma and invasive form of mole, as well as for a more precise diagnosis if it is necessary to prescribe chemotherapy to monitor its effectiveness), chest radiography (establishes the presence and nature of metastases in the lungs, which allows one to judge the extent of the disease, although it does not specify the nature of the trophoblastic tumor).
Laboratory tests determine the level of human chorionic gonadotropin (hCG) in urine and blood serum, placental lactogen, estriol, human chorionic thyrotropin, alpha-fetoprotein.
Histological verification is one of the main diagnostic methods, which makes it possible to establish not only the presence of trophoblastic disease, but also to clarify the nature of the tumor.
Treatment of trophoblastic disease
Since the introduction of antimetabolites into clinical practice, chemotherapy has become the main treatment method for malignant trophoblastic disease.
Indications for chemotherapy are:
histological diagnosis of chorionic carcinoma; presence of metastases; stable or increasing levels of serum β-hCG after removal of a hydatidiform mole; an increase in the level of β-hCG after its preliminary return to normal. The regimen and type of chemotherapy are selected individually depending on the nature of the disease. Chemotherapy is continued until serum β-hCG levels fall to normal levels. After this, another 1-3 cycles are performed. Recently, a sensitive response to β-CG has been used, and these additional courses may not be necessary in low-risk patients. For high-risk patients, 2-6 additional cycles of chemotherapy are recommended.
Surgical methods are also used for treatment: curettage of the walls of the uterine cavity, and in rare cases, supravaginal amputation or hysterectomy.
Indications for surgery are:
resistance to chemotherapy or toxicity in disease limited to the uterus, vaginal bleeding, uterine perforation, infection. Radiation therapy can also be used in treatment when patients with metastases to the liver or brain may develop hemorrhages due to tumor necrosis during chemotherapy.
All patients should be monitored monthly with hCG levels tested for at least the first year. After one year, high-risk patients should be examined twice a year for 5 years and then annually thereafter. β-hCG levels are checked at each visit.
The optimal period for pregnancy is at least 1 year after the last preventive course of chemotherapy for patients with stages I - II of the disease and 1.5 years for patients with stages III - IV. An option for protection against unwanted and untimely pregnancy for women who have had trophoblastic disease is hormonal contraception. At the same time, ovarian function, impaired as a result of the disease and/or chemotherapy, is regulated and normalized. The drugs used to treat trophoblastic disease do not affect the chromosome composition of the mother and child.
Chemotherapy can cure 100% of patients with non-metastatic disease and 70% or more of patients with high-risk disease. Ovarian chorionic carcinoma does not respond well to chemotherapy, and the prognosis is almost always poor. The presence of metastases worsens the prognosis of the disease.
Trophoblastic tumor of the placental site
Recently, trophoblastic tumor of the placental site has been identified as a separate histogenetic form. The tumor is rare. The clinical course of the tumor is generally assessed as benign, however, it is potentially metastatic and requires urgent removal of the uterus. The incidence of metastasis is 15%. The most common locations of metastases are the vagina, lungs, liver, abdominal cavity, and brain. A favorable outcome is observed in 85% of women after hysterectomy.
Make an appointment with specialists by calling a single call center:
+7(495)636-29-46 (metro stations “Schukinskaya” and “Street 1905 Goda”). You can also make an appointment with a doctor on our website, we will call you back!
Treatment
The treatment tactics for hydatidiform mole are based on the evacuation of pathological tissue from the uterus (removal of hydatidiform mole). This can be done using the method of vacuum aspiration of the contents of the female reproductive organ. And then curettage of the uterine cavity is performed. If there is a condition that threatens the patient's life, for example, bleeding from an invasive mole, then doctors may decide to remove the uterus.
After evacuation of the contents from the uterine cavity, mandatory monitoring of the level of hCG in the blood is carried out weekly. If the hCG level does not fall over time, then chemotherapy treatment is necessary. Once every two weeks, ultrasound diagnostics of the uterine cavity and appendages is performed.
If no signs of chorionepithelioma are found, then chemotherapy is not performed, and the woman is prescribed clinical observation for a period of two years.
Complications
In some cases, the unremoved cells do not die, but continue to multiply, forming more and more cysts (recurrent hydatidiform mole). The worst option is the transformation of the tumor into malignant choriocarcinoma. Cancer cells penetrate the tissue of the uterus, sometimes growing through it and causing internal bleeding. When tumor cells grow into blood vessels, they spread through the blood to organs and form metastases, most often in the lungs, brain or liver.
Chemotherapy is highly effective if choriocarcinoma and recurrent hydatidiform mole are detected in time. Relapse after treatment occurs in approximately 1-3% of women. It is imperative to monitor the level of hCG, since this indicator helps to notice the re-development of the disease in time and begin a course of chemotherapy in a timely manner.
New pregnancy after hydatidiform mole
The most pressing question after a case of hydatidiform mole is whether pregnancy can occur after a hydatidiform mole.
The diagnosis of hydatidiform mole is not a death sentence. With proper and timely diagnosis and proper treatment, pregnancy is possible. An important point is the timely administration of chemotherapy after a hydatidiform mole in the absence of a drop in hCG levels.
Pregnancy after a hydatidiform mole simply needs to be planned. If chemotherapy was not prescribed after such a pathological condition, then the minimum period of absence of pregnancy is 6-12 months. If chemotherapy was nevertheless prescribed, then the recommended break is 12-24 months. The main point in planning such a pregnancy is the appointment of competent contraception by the obstetrician-gynecologist who is caring for you.
Subsequent pregnancies
Repeated pregnancy should be planned only after the entire period of monitoring hCG levels has been completed. In the future, a woman has a good chance of conceiving, bearing and giving birth to a healthy child. The doctor leading the pregnancy must know about previous hydatidiform moles, as well as other features of previous pregnancies. Since women who have already been diagnosed once are at a slightly higher risk of developing it, they may be recommended to have their first ultrasound scan earlier than with the standard examination regimen.