Flu is an acute viral infection. The main routes of transmission are airborne droplets and household contact. From the moment of infection with the virus until signs of the disease appear, 1 to 4 days pass.
The need for timely treatment is due to the seriousness of the complications that the flu can cause. Among them: bronchitis, tonsillitis, pneumonia, otitis media, sinusitis, pulmonary or cerebral edema, swelling of the vocal cords, meningitis, myocarditis.
That is why it is important to prevent ARVI, be attentive to changes in your health, and if the disease begins, take action immediately.
What it is
Influenza A is a respiratory viral infection that primarily affects the respiratory system. It has a short incubation period, rapid spread and a high risk of complications.
During the disease process, the pathogen multiplies on the mucous surface of the epithelial tissue of the pharynx, trachea, and nasal cavity. Depending on the location of the virus, characteristic symptoms develop in the form of a severe cough, sore throat, nasal congestion and other signs.
A high body temperature is noted against the background of the accumulation of decay products of affected cells and tissues, the remains of which enter the bloodstream. Vascular permeability also increases due to endothelial damage. Therefore, it is possible to develop a slight hemorrhage in the respiratory organs, including the brain.
The causative agent of influenza has a general negative effect on the immune and circulatory systems. This can cause secondary pathologies of a viral or infectious nature, which significantly aggravate the course of the disease and lead to complications.
ARVI and acute respiratory infections: what is the difference
First, let's understand the terms. ARVI is an acute respiratory viral infection that can be caused by a large number of different viruses. ARI – acute respiratory diseases. Previously, this was the designation for all respiratory diseases of both a viral and viral-bacterial nature. And ARI (acute respiratory infections) is a term that replaced acute respiratory infections. These infections can also be caused by viruses and bacteria. There is no big difference between the presented groups of diseases. One abbreviation assumes that the causative agents of diseases are only viruses, which is what happens in most cases; another name does not exclude a bacterial component. Clinically, these infections are very similar, which made it possible to combine them into groups.
When do outbreaks of acute respiratory infections occur?
As a rule, an increase in the incidence of ARVI and ARI is observed in the cold season, and the prevalence of infection is widespread - colds and flu are familiar firsthand not only to children, but also to adults in all countries of the world. According to WHO, during periods of peak incidence, these infections are diagnosed in almost 30% of the world's population.
But any cold and flu viruses that have entered the human body do not immediately make themselves felt. There are many varieties of acute respiratory viral infections, the type of which determines the timing of the development of clinical symptoms when a person realizes that he is sick. Runny nose, cough, sore throat and other similar symptoms can be caused by various types of influenza viruses, parainfluenza, adenoviruses, rhinoviruses, reoviruses, ECHO and Coxsackie viruses.
Routes of transmission and causes
The cause of influenza is damage to the body by type A viral strains.
The main sources of the infectious process are people, patients or carriers, as well as animals and birds.
Infection is carried out by air, the period from the penetration of the virus into the body until the appearance of the first signs is no more than 2 days. Therefore, the disease is characterized by a high degree of contagiousness.
Contributing factors to viral infection are a decrease in the immune system, close contact with sick people and the presence of concomitant pathologies.
People at risk for developing influenza A include:
- Women during pregnancy.
- Small children of preschool age.
- Health care workers.
- People exposed to frequent stress, having neoplasms, vitamin deficiencies, and following a strict diet.
Antiviral drug VIFERON
In children, the level of antiviral protection is significantly lower than in adults. This is primarily determined by the low ability of leukocytes and lymphocytes to induce their own interferons - proteins with similar properties, secreted by body cells in response to virus invasion. This, among other reasons, explains the predisposition of the child’s body to frequent ARVI. Antiviral drugs can compensate for this feature. When treating children, special attention should be paid to antiviral drugs, which cover the entire etiological spectrum of acute respiratory infections, including influenza.
The obvious advantages of drugs containing interferon over other antiviral drugs is their high non-selective antiviral activity. This means that such drugs are able to fight all types of acute respiratory viral infections, without additional tests or specifying the strain of the influenza virus.
To prevent undesirable consequences of acute respiratory viral infections in a child, in consultation with a doctor, you can use the antiviral drug VIFERON Suppositories.
It can be used to treat children from the first days of life and expectant mothers from the 14th week of pregnancy.1
How do VIFERON Candles work?
The drug VIFERON Suppositories (suppositories) contains human recombinant interferon alpha-2b and has antiviral and immunomodulatory properties. It prevents the multiplication of the virus in the human body, which ensures the prevention and treatment of viral and other diseases.
Since the drug VIFERON Suppositories (suppositories) has a wide spectrum of antiviral activity, it is a universal remedy against influenza and ARVI. This drug helps fight infection at any stage of the disease. VIFERON provides a powerful antiviral effect and allows you to shorten the overall duration of the disease, quickly cope with the manifestations of infection (runny nose, cough, weakness, fever, etc.), and also reduces the likelihood of developing complications and subsequent diseases. 2
You can also use the drugs VIFERON Gel and VIFERON Ointment to treat children.
For the treatment of ARVI in children from 1 year to 2 years old, VIFERON Ointment 2500 IU (1 pea with a diameter of 0.5 cm) is used 3 times a day, for children from 2 to 12 years old - ointment 2500 IU (1 pea with a diameter of 0.5 cm) 3 times a day. .5 cm) 4 times a day, for children from 12 to 18 years old - ointment 5000 IU (1 pea with a diameter of 1 cm) 4 times a day. The duration of treatment is 5 days.
VIFERON Gel can be used for the prevention and treatment of children from the first days of life. In order to protect your child from colds and flu, it is necessary to apply a strip of gel approximately 0.5 cm long to the nasal mucosa 2 times a day as a preventive measure. Course duration is 2-4 weeks. For the treatment of ARVI, including influenza, including those complicated by a bacterial infection, the application of VIFERON gel must be repeated 3-5 times a day for 5 days.
Reference and information material
Author of the article
Belyaev Dmitry Alexandrovich
General doctor
- VIFERON Suppositories are approved for use by children from the first days of life and pregnant women from the 14th week of pregnancy, VIFERON Gel - by children from the first days of life, there are no restrictions for use during pregnancy, VIFERON Ointment - from 1 year, there are no restrictions for use during pregnancy.
- Nesterova I.V. “Interferon drugs in clinical practice: when and how,” “Attending Physician,” September 2021.
Loading...
Take other surveys
Influenza A virus
Influenza A virus belongs to the group of orthomyxoviruses. It is dangerous and has a high degree of mutation. This is the only type capable of causing a pandemic and rapid spread in society.
It is most active in the autumn and spring seasons. Various animals, birds, and people can act as potential hosts of the pathogen. Thanks to this, the virus quickly adapts and changes genetic information in a short period of time.
Due to the presence of 2 proteins in their structure: hemagglutinin and neuraminidase, doctors are able to differentiate the pathology from other infectious viral diseases.
As a rule, the main cause of influenza A in humans is not considered to be the pathogen itself, but its subtypes H1N1 and H3N2.
Influenza: history, clinical picture, pathogenesis
The term "flu" is derived from it. greifen and french. gripper (grab, paralyze), becoming widespread in Europe during the epidemic of 1742–1743. In Russia, the term “flu” began to be used only at the beginning of the 19th century - for example, in the first volume of L. N. Tolstoy’s novel “War and Peace” we find: “Anna Pavlovna coughed for several days, she had the flu, as she said (the flu was then a new word, used only by rare people).
Etiology of influenza
Influenza is an acute respiratory viral disease, etiologically associated with representatives of three genera - Influenza A virus (influenza A viruses), Influenza B virus (influenza B viruses) and Influenza C virus (influenza C viruses) - from the family Orthomyxoviridae [2, 26].
Influenza A virus was first isolated from pigs by American virologist Richard Shoup (1901–1966) in 1930; from people - three years later by a group of English scientists: Wilson Smith (1897–1965), Christopher Andrews (1896–1987) and Patrick Laidlaw (1881–1940) [26].
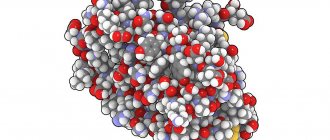
| Rice. 1. Structure of the influenza A virus virion (Orthomyxoviridae, Influenza A virus) |
On the surface of the virion (viral particle) of the influenza A virus there are two functionally important molecules (Fig. 1): hemagglutinin (with the help of which the virion attaches to the surface of the target cell); neuraminidase (which destroys the cellular receptor, which is necessary during the budding of daughter virions, as well as to correct errors due to incorrect binding to the receptor) [2, 24, 26].
Currently, 16 types of hemagglutinin (designated as H1, H2, ..., H16) and 9 types of neuraminidase (N1, N2, ..., N9) are known. The combination of hemagglutinin type and neuraminidase (for example, H1N1, H3N2, H5N1, etc.) is called a subtype: out of 144 (16 × 9) theoretically possible subtypes, 115 are known today [24].
The natural reservoir of the influenza A virus is wild birds of the aquatic ecological complex (primarily dabbling ducks, gulls and terns), but the virus is able to overcome the interspecies barrier, adapt to new hosts and circulate in their populations for a long time [9–12]. Epidemic variants of the influenza A virus cause an annual increase in incidence and dangerous pandemics every 10–50 years [1, 11, 16].
The influenza B virus was discovered in 1940 by American virologist Thomas Francis Jr. (1900–1969). Influenza B virus does not cause a pandemic, but is the causative agent of large epidemic outbreaks [26].
Influenza C virus was discovered in 1947 by American virologist Richard Taylor (1887–1981). Influenza C virus causes local epidemic outbreaks in children's groups. The infection is most severe in young children [26].
Influenza viruses occupy an important place in the structure of the incidence of acute respiratory viral infections (ARVI), which account for up to 90% of all other infectious diseases. According to the World Health Organization (WHO), 3–5 million people worldwide fall ill with severe forms of influenza alone every year. Every year, 25–35 million people fall ill with influenza and other acute respiratory viral infections in the Russian Federation, of which 45–60% are children. The economic damage to the Russian Federation from seasonal epidemic influenza amounts to up to 100 billion rubles/year, or about 85% of economic losses from infectious diseases [2–8, 20–23].
History of influenza pandemics
Hippocrates' (460–377 BC) description of influenza as the "Perinthian cough" is considered the first scientific description of the disease (412 BC). In the 9th–18th centuries, influenza was known as “peasant fever”; warm foot baths and heated red wine with spices were recommended as treatment. From the beginning of the 16th century, with an increase in population density, epidemic “waves” began to roll across all of Europe. In the 17th century, five major epidemics were recorded in Europe, and three in the 18th century. During the epidemic of 1675, the famous English physician Thomas Sydenham (1624–1689) suggested that the “English prickly heat” was of an infectious nature and described a version of this disease, which he called febris comatosa, which was accompanied by the development of symptoms from the central nervous system (CNS).
In 1889–1892 The first documented influenza A(H2N2) pandemic occurred. The Spanish flu (H1N1) pandemic (1918–1919) sickened 600 million and killed 50–100 million1 (i.e., 30% and 5% of the world's population, respectively). The Asian influenza (H2N2) pandemic (1957–1959) killed more than 1 million; Hong Kong flu pandemic (1968–1970) - about 1 million; major epidemic of “Russian flu” (H1N1) (1977–1978) - about 300 thousand people.
A feature of the pandemics of 1889–1892. and the Spanish Flu of 1918–1919. there was a lack of information about the etiological agent of the disease (doctors of that time considered the Afanasyev-Pfeiffer bacillus, Haemophilus influenzae, as the causative agent of the infection). The number of severe and fatal cases of infection sharply declined during subsequent pandemics, which is associated primarily with the advent of influenza vaccines, the strain composition of which is determined annually by WHO based on data from the Global Influenza Monitoring Program (operating since 1947), etiotropic antiviral drugs Amantadine and Rimantadine (1963), as well as antibiotics (1941) for the treatment of secondary pneumonia.
The modern pandemic of “swine flu” (H1N1) swl2 (2009–2010) began as a result of the emergence of epidemic potential in one of the variants of the swine influenza A (H1N1) virus [16]: in mid-March 2009 there was a sharp jump in incidence in the city La Gloria (Mexico, Veracruz state), at the end of March the first laboratory-confirmed cases appeared in the United States, at the end of April - in Canada, and then in Europe. In the Russian Federation, the identification of the first case of the disease and isolation of the strain were carried out by employees of the Federal State Institution Research Institute of Virology named after. D.I. Ivanovsky” Ministry of Health and Social Development of Russia May 21, 2009 [13, 15, 25]. The WHO announced the beginning of the next influenza pandemic on June 11, 2009, and its end on August 10, 2010. During this period, influenza caused the death of 18.5 thousand people worldwide.
In the first post-pandemic epidemic season of 2010–2011. pandemic influenza A(H1N1) swl caused more than 70% of ARVI cases in the world, influenza A(H3N2) - 1-5%, influenza B - 10-20%.
Composition of influenza vaccines in the 2011–2012 epidemic season. (same as 2010–2011): A/California/07/2009 (H1N1) swl; A/Perth/16/2009 (H3N2); B/Brisbane/60/2008.
The pandemic influenza A(H1N1) swl virus is resistant to Remantadine and Amantadine, but sensitive to Tamiflu, Relenza, Ingavirin, Arbidol and Ribavirin [13–16, 18, 19, 23].
Highly virulent avian influenza A(H5N1) is a possible causative agent of the next pandemic.
The likelihood of the influenza A virus crossing the interspecies barrier and entering the human population with dangerous consequences increases sharply during epizootic periods3. Therefore, the highly virulent avian influenza A(H5N1) virus, which has caused a modern large-scale epizootic among wild and domestic birds of the Old World and has an increased ability to reproduce in mammalian cells, is considered as the most likely causative agent of the next influenza pandemic [10, 11, 17]. Further spread of this virus could have catastrophic consequences if it develops epidemic potential (the ability to be transmitted from person to person), since, firstly, humanity does not have collective immunity to influenza A (H5) viruses, and secondly, because 563 laboratory-confirmed cases of human disease in 15 countries as a result of infection with the influenza A(H5N1) virus of avian origin during 2003–2011. 330 died, i.e., the mortality rate is approaching 60% [11, 24].
In the Russian Federation, no human cases of influenza A(H5N1) virus of avian origin have been detected. However, Russian researchers continue to regularly monitor this dangerous infection (si vis pacem, para bellum) and have made a significant contribution to reducing the likelihood of unfavorable developments: the main features of the development of the epizootic process were predicted, prototype viral strains were deposited in the State Collection of Viruses of the Russian Federation, their biological properties were studied (in particular, it has been shown that strains of highly virulent avian influenza A(H5N1) virus are sensitive to commercial anti-influenza chemotherapy drugs: Remantadine, Amantadine, Tamiflu, Relenza, Ingavirin, Arbidol, Ribavirin), at the Federal State Institution "Research Institute of Virology named after. D.I. Ivanovsky" Ministry of Health and Social Development of Russia received Russian patents for the vaccine strain, and developed domestic veterinary (which is actively used) and medical (which is waiting in the wings) vaccines [10, 11, 17, 24].
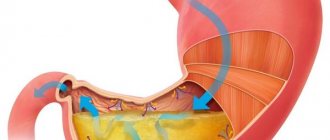
Pathogenesis of influenza
In humans, influenza viruses infect epithelial cells of the mucous membrane of the respiratory tract, as well as goblet cells (secreting mucus), alveolocytes and macrophages [3, 4, 7]. All these cells have on their surface a receptor to which the viral hemagglutinin binds (Fig. 1), the terminal residue of sialic, or N-acetylneuraminic acid (Neu5Ac) (Fig. 2), as part of the polysaccharide chains that are part of gangliosides and glycoproteins. The terminal sialic acid residue can bind to the next monosaccharide in two ways: via an alpha2-3 or alpha2-6 linkage (Fig. 2) [14, 18].
| Rice. 2. Structural formulas of sialic or N-acetylneuraminic acid (Neu5Ac) and two ways of covalent bonding with the following monosaccharide (in this case galactose, Gal): alpha2-3- or alpha2-6-bond |
Epithelial cells of the human upper respiratory tract contain mainly alpha2-6-sialosides; lower sections - alpha2-3-sialosides (Fig. 3). Therefore, epidemic strains of influenza viruses, having alpha2-6 specificity, easily reproduce in the upper parts of the human respiratory tract, are actively released into the environment when speaking, sneezing, coughing, and effectively infect other people through airborne droplets.
Variants of influenza A virus adapted to birds have alpha2-3 specificity (Fig. 3). Terminal alpha2-3-sialosides are found in birds mainly on the surface of epithelial cells of the intestinal mucosa, therefore in birds influenza occurs in the form of enteritis; the virus is released into the external environment with feces, and infection occurs through the nutritional route. The alpha2-3 specificity of avian variants of influenza A virus explains their inability to effectively infect the epithelium of the upper parts of the human respiratory tract and, as a result, be transmitted by airborne droplets in the human population. At the same time, if a highly virulent avian influenza A virus somehow manages to cause a productive infection in the human body, then it will effectively infect the lower parts of the respiratory tract, causing severe primary viral pneumonia (according to WHO, in 60% of cases - fatal) .
Epithelial cells of pigs simultaneously contain both alpha2-6- and alpha2-3-sialosides (Fig. 3), therefore, both epidemic and avian variants of the influenza A virus can simultaneously circulate in the body. As a result, in pig populations, firstly, the formation of reassortants4 of human and avian strains with new biological properties; secondly, strains with mixed alpha2-6/alpha2-3 specificity are selected. It is precisely this mixed alpha2-6/alpha2-3 specificity that strains of the pandemic influenza A(H1N1) swl virus possess, and, as a result, they have the ability to spread by droplet airborne routes and cause severe pneumonia [13–15, 18, 19, 23 ].
| Rice. 3. Sialoside receptors of influenza A viruses on the surface of epithelial cells of humans (alpha2-6 - on the mucous membrane of the upper, alpha2-3 - on the mucous membrane of the lower parts of the respiratory tract), pigs (alpha2-6 / alpha2-3 mixture on the mucous membrane of the respiratory tract) and birds (alpha2-3 - on the intestinal mucosa) |
Infection of epithelial cells results in a rapid increase in the viral load, apoptosis, degeneration and necrosis of this type of cell with the subsequent development of toxic and toxic-allergic reactions. In humans, damage to the columnar epithelial cells of the trachea and bronchi is typical. The main link in the pathogenesis of influenza A is damage to the vascular and nervous systems that occurs as a result of the toxic effect of the virus. At the same time, one of the main mechanisms of the influence of the influenza A virus on the vascular system is the formation of reactive oxygen species that interact with phospholipids of cell membranes, causing lipid peroxidation in them, disruption of membrane transport and barrier functions, contributing to the further development of viral infection. Lysosomal enzymes additionally damage the capillary epithelium and the basement membrane of cells, which contributes to the spread of influenza infection and viremia. Increased vascular permeability, fragility of their walls, and impaired microcirculation are the cause of hemorrhagic manifestations - from nosebleeds to hemorrhagic pulmonary edema and hemorrhages in the brain. Circulatory disorders, in turn, cause damage to the central nervous system: the pathomorphological picture is characterized by the presence of lymphomonocytic infiltrates around small and medium veins, hyperplasia of glial elements and focal demyelination, which indicates the toxic-allergic nature of the pathological process in the central nervous system during influenza [3–8, 23] .
An important factor in the pathogenesis of influenza is the production of the viral protein PB1-F2, which causes apoptosis of tissue macrophages of the lungs and thereby contributes to the development of secondary bacterial pneumonia (in the modern pandemic variant of the influenza A(H1N1) swl virus, the production of PB1-F2, fortunately, is absent, which reduces - but does not eliminate! - the likelihood of developing secondary pneumonia, leaving the danger of primary viral pneumonia intact - see below) [2, 26].
Clinical picture of influenza in humans
The onset is acute, with chills, a rapid rise in temperature to high numbers, and a sharp increase in symptoms of intoxication. The temperature reaches maximum values (39.0–40.0 °C) on the first day of the disease. During the same period, signs of intoxication increase: chills, severe headache, dizziness, myalgia, arthralgia, severe weakness. On external examination: the face is hyperemic, puffy, the vessels of the sclera are injected, hyperemia of the conjunctiva, cyanosis of the lips and mucous membrane of the oropharynx are detected, pinpoint hemorrhages on the soft palate are possible. Cyanosis in general is an important symptom of influenza: you should pay attention not only to cyanosis of the lips, but also to the cyanotic tint of the uvula, tonsils, palatine arches against the background of bright hyperemia of the oropharyngeal mucosa; the mucous membrane of the soft palate also has a cyanotic tint, fine granularity, vascular injection and pinpoint hemorrhagic elements are clearly visible; on the posterior wall of the pharynx - moderate hyperplasia of lymphoid tissue.
Localization of headache: in the frontotemporal region and in the eyeballs (with light pressure on them or when they move). Meningeal signs are often detected, which gradually disappear with a decrease in intoxication and a decrease in body temperature. The range of clinical manifestations from the nervous system is quite wide: from functional disorders to serous meningitis and severe meningoencephalitis.
Damage to the respiratory tract during influenza is the leading one: catarrhal symptoms in the form of nasal congestion or slight rhinitis are observed in all patients; cough (dry, painful, with pronounced rumbles and “roars”, dry wheezing in the lungs), which develops by the end of the first day of illness, is very characteristic of influenza A - due to tracheitis common with influenza - and can serve as a differentiating clinical sign. In the pandemic (2009–2010) and post-pandemic (2010–2011) periods, a long (8–10 days) cough was recorded, with symptoms of bronchitis, which in some patients persisted for several weeks (which indicated involvement in the pathological process small airways); During auscultation of the lungs, hard breathing was heard, often dry scattered wheezing. In addition, in 2009–2011. Some patients experienced diarrhea in the first two days of the disease: 5% of moderate and 10% of severe patients [8, 18, 23].
Pneumonia is one of the most dangerous complications of influenza. There are three types of pneumonia: 1) primary viral; 2) secondary viral-bacterial; 3) secondary bacterial (or “day 14 pneumonia”) [3–8, 23].
Primary viral pneumonia develops in the first days of the disease (2–5 days) and is characterized by severe intoxication, often hemorrhagic manifestations (nosebleeds, streaks of blood in the sputum), a rapid increase in respiratory failure (feeling of lack of air, shortness of breath, increased cyanosis). Auscultation during inspiration reveals characteristic crepitating rales. Bilateral lung damage and severe respiratory failure are consistent with acute lung injury (ALI). Developing acute respiratory distress syndrome (ARDS) is characterized by significant arterial hypoxemia and diffuse alveolar infiltrates. Computed tomographic examination is characterized by uneven thickening of the interalveolar and interlobular septa (“reticular lung”) and a decrease in the transparency of the lung fields like “ground glass”. Signs of active bacterial infection, as a rule, cannot be detected. Most patients have leukopenia, thrombocytopenia, high levels of lactate dehydrogenase, creatine phosphokinase.
With the development of secondary pneumonia against the background of a viral infection, signs of bacterial exposure are determined, confirmed by the detection of bacteria Streptococcus pneumoniae, Staphylococcus aureus, etc. in the sputum. As a rule, secondary pneumonia develops after 5–7 days of influenza and is characterized by a repeated rise in temperature to febrile values, increased cough, the appearance of mucopurulent sputum, often streaked with blood, radiologically - focal and focal-confluent infiltrates, often with signs of destruction and abscess formation. After 10 days, pneumonia usually has a bacterial etiology and is most often associated with gram-negative microflora.
One of the main factors contributing to the severe course of influenza is concomitant pathology. In particular, in patients who died during the last two epidemic seasons of 2009–2011, heart and vascular diseases, diabetes mellitus, metabolic syndrome (obesity), alcoholism and tobacco smoking predominated. A special risk group is pregnant women, in whom pneumonia can develop rapidly, and therefore they require special attention from clinicians and immediate treatment.
An analysis of fatal outcomes showed that outpatient doctors are gradually losing their wariness regarding pandemic influenza A(H1N1) swl: there were cases of late hospitalization due to underestimation of the severity of the patient’s condition and the risk of developing rapidly progressing pneumonia. All patients require urgent etiotropic therapy according to the principle “the sooner the better”: the first 36–48 hours of illness are optimal. The use of antiviral drugs within the specified time frame significantly reduces the duration and severity of the disease, as well as the frequency of complications. In future epidemic seasons, lessons need to be learned from previous experiences.
Literature
- Gendon Yu. Z. Influenza pandemic: is it possible to fight it // Questions of Virology. 1998. No. 1. P. 43–46.
- Kaverin N.V., Lvov D.K. Orthomyxoviridae. In the book: Medical virology. Hand-in. Ed.: Academician of the Russian Academy of Medical Sciences D.K. Lvov. M.: MIA, 2008. pp. 176–183.
- Ketiladze B. S., Ivanova L. A., Eliseeva I. Ya. et al. The importance of various respiratory viruses in the development of chronic nonspecific bronchopulmonary processes // Questions of Virology. 1986. No. 3. P. 310–314.
- Kolobukhina L.V. Viral infections of the respiratory tract // Breast Cancer. 2000. T. 8. No. 13–14. pp. 559–564.
- Kolobukhina L.V. Clinic and treatment of influenza // Breast Cancer. 2001. T. 9. No. 16–17. pp. 710–713.
- Kolobukhina L.V. Viral infections of the respiratory tract. In the book: Respiratory medicine: a guide. Ed.: Academician of the Russian Academy of Medical Sciences A. G. Chuchalin. M.: GEOTAR-Media, 2007. T. 1. P. 449–474.
- Kolobukhina L.V., Lvov D.K., Burtseva E.I. Gripp. In the book: Medical virology. Hand-in. Ed.: Academician of the Russian Academy of Medical Sciences D.K. Lvov. M.: MIA, 2008. pp. 382–393.
- Kolobukhina L.V., Shchelkanov M.Yu., Merkulova L.N. et al. Etiotropic therapy of influenza: lessons from the last pandemic // Bulletin of the Russian Academy of Medical Sciences. 2011. No. 5. pp. 35–40.
- Lvov D.K. Possible significance of natural biocenoses in the variability of influenza A virus // Questions of Virology. 1974. No. 6. P. 740–744.
- Lvov D.K. Population interactions in a biological system: influenza A virus - wild and domestic animals - humans; causes and consequences of the penetration of the highly pathogenic influenza virus A/H5N1 into the territory of Russia // ZhMEI. 2006. No. 3. P. 96–100.
- Lvov D.K. Ecology of viruses. In the book: Medical virology. Hand-in. Ed.: Academician of the Russian Academy of Medical Sciences D.K. Lvov. M.: MIA, 2008. pp. 101–118.
- Lvov D.K., Ilyichev V.D. Migrations of birds and transfer of infectious agents. M.: Nauka, 1979. 270 p.
- Lvov D.K., Burtseva E.I., Prilipov A.G. et al. Isolation on May 24, 2009 and depositing in the State Collection of Viruses (GKV No. 2452 dated May 24, 2009) of the first strain A/IIV-Moscow/01/2009 (H1N1) swl, similar to swine virus A (H1N1) from the first patient identified on May 21, 2009 in Moscow // Questions of Virology. 2009. T. 54. No. 5. P. 10–14.
- Lvov D.K., Burtseva E.I., Prilipov A.G. et al. Possible connection of lethal pneumonia with mutations of the pandemic influenza virus A/H1N1 swl in the receptor-binding site of the HA1 subunit of hemagglutinin // Questions of Virology. 2010. T. 55. No. 4. P. 4–9.
- Lvov D.K., Burtseva E.I., Shchelkanov M.Yu., Prilipov A.G., Kolobukhina L.V., Malyshev N.A., Bazarova M.V., Merkulova L.N., Deryabin P. G., Kuzmichev A. G., Fedyakina I. T., Grebennikova T. V., Usachev E. V., Sadykova G. K., Shevchenko E. S., Trushakova S. V., Lavrishcheva V. V. ., Alkhovsky S. V., Samokhvalov E. I., Belyakova N. V., Ivanova V. T., Oskerko T. A., Latyshev O. E., Belyaev A. M., Belyaev A. L., Feodoritova E. L. Spread of the new pandemic influenza virus A(H1N1) v in Russia // Questions of Virology. 2010. T. 55. No. 3. 4–9.
- Lvov D.K., Malyshev N.A., Kolobukhina L.V. et al. Influenza caused by the new pandemic virus A/H1N1 swl: clinical picture, diagnosis, treatment. Guidelines. M.: Moscow Department of Health, 2009. 18 p.
- Lvov D.K., Fedyakina I.T., Shchelkanov M.Yu. et al. Effect of in vitro antiviral drugs on the reproduction of highly pathogenic strains of influenza A/H5N1 virus that caused an epizootic among poultry in the summer of 2005 // Questions of Virology. 2006. T. 51. No. 2. P. 20–22.
- Lvov D.K., Shchelkanov M.Yu., Bovin N.V. et al. Correlation between the receptor specificity of strains of the pandemic influenza A(H1N1) pdm09 virus isolated in 2009–2011, the structure of the receptor-binding site and the likelihood of development lethal primary viral pneumonia // Questions of virology. 2012. No. 1.
- Lvov D.K., Yashkulov K.B., Prilipov A.G. et al. Detection of amino acid substitutions of aspartic acid with glycine and asparagine in the receptor-binding site of hemagglutinin in variants of the pandemic influenza A(H1N1) swl virus from patients with a fatal outcome and with a moderate form of the disease // Questions of Virology. 2010. T. 55. No. 3. P. 15–18.
- Sadov A. A. Epidemic influenza. L., 1927. 60 p.
- Smorodintsev A. A. Influenza and its prevention. M.: Medicine, 1984. 384 p.
- Supotnitsky M.V. The Spanish Flu pandemic of 1918–1920. in the context of other influenza pandemics and “bird flu” // Medical records. 2006. No. 11. P. 31–34; 2006. No. 12. P. 15–22; 2007. No. 1. pp. 16–22.
- Chuchalin A. G. Influenza: lessons from the pandemic (clinical aspects) // Pulmonology. 2010. Appendix 1. pp. 3–8.
- Shchelkanov M. Yu., Lvov D. K. Genotypic structure of the genus Influenza A virus // Bulletin of the Russian Academy of Medical Sciences. 2011. No. 5. pp. 19–23.
- Shchelkanov M. Yu., Lvov D. N., Fedyakina I. T. et al. Dynamics of the spread of pandemic influenza A(H1N1) swl in the Far East in 2009 // Questions of Virology. 2010. T. 55. No. 3. P. 10–15.
- Shchelkanov M. Yu., Fedyakina I. T., Proshina E. S. et al. Taxonomic structure of Orthomyxoviridae: current state and immediate prospects // Bulletin of the Russian Academy of Medical Sciences. 2011. No. 5. pp. 12–19.
M. Yu. Shchelkanov, Doctor of Biological Sciences, Associate Professor L. V. Kolobukhina, Doctor of Medical Sciences, Professor D. K. Lvov, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Medical Sciences
Federal State Institution "Research Institute of Virology named after. D. I. Ivanovsky", Moscow
Contact information for authors for correspondence
1 For comparison, 8.3 million people died as a result of hostilities during the 5 years of the First World War (1914–1918).
2 The abbreviation “swl” refers to the English. the phrase “swine-like”, i.e. strains “similar to swine”.
3 Epizootic is the process of spreading an infectious disease in animal populations.
4 The influenza A virus has a genome consisting of 8 individual RNA molecules. Reassortment is the formation of a strain in which the source of different genetic segments was different parental strains that simultaneously infected the same cell.
Symptoms of the disease
The first symptoms of the pathology appear 2 days after infection, rarely after 4 days.
In the initial stages, the disease is accompanied by high fever up to 39 C, weakness, malaise, slight runny nose with continued nasal breathing and sore throat.
As the pathogen acts in the body, the following obvious signs are noted:
- Headache.
- Chills alternating with fever.
- Painful sensations in the throat.
- Cough, often dry.
- Severe runny nose, possible nasal congestion.
- Severe weakness.
- Drowsiness.
- Aches and pain throughout the body.
As a rule, temperature recovery occurs within a week without medical intervention. In the absence of complications, the cough goes away after 7-10 days.
If a viral infection occurs in a particularly severe form and is accompanied by pallor of the skin, the development of cyanosis, prolonged elevated body temperature, pain in the chest area and disruption of the cardiovascular system, it is necessary to call an ambulance.
Contagiousness during the acute period of influenza
It doesn’t matter whether the patient is suffering from the infection “on his feet” or lying in bed, he can transmit the virus to others with the greatest ease precisely at the height of the disease. Acute clinical symptoms: nasal discharge, coughing, increased breathing and sneezing contribute to the spread of pathogens around. From the moment the first signs of flu appear until they disappear completely, a person is extremely contagious. The virus can be found not only on its mucous membranes:
- skin and hair are also dangerous, since the infection settles on them, released with droplets of sputum from the respiratory tract;
- pathogenic particles remain for several hours on linen, clothing, objects and surfaces touched by the patient;
- from 15 minutes to 5 hours, the influenza virus is present in the air of the room where the infected person is located: in aerosol particles of sputum, water vapor, dust.
At the acute stage of the disease, a person with influenza can transmit the infection not only respiratoryly, but also through contact. You can get infected from him by taking his comb, pen, plate or phone. And after being in an unventilated room or hospital ward, you can catch the virus even from a patient, even in his absence.
Changes in health during illness do not affect the risk of transmitting infection to them. All precautions must be taken until the symptoms disappear completely. Usually this is a period from 7 to 12 days. But in some cases, due to the weakness of the immune response, the disease drags on for 3–4 weeks.
Treatment methods
Treatment measures begin after confirmation of the diagnosis based on clinical data and examination of the patient.
People who are at risk and have a severe form of pathology should undergo treatment in a hospital. In other cases, the necessary treatment procedures can be carried out at home.
Methods to combat influenza are as follows:
- Limiting contact between a sick person and healthy people.
- Preventive measures.
- Pharmacological therapy.
The main goal in case of infection is to relieve the symptoms and cause. Therefore, the main groups of drugs for influenza A are antiviral, anti-inflammatory, antipyretic, and vasoconstrictor drugs. Additionally, antihistamines, antitussives, hormones and vitamins are prescribed.
The course and duration of treatment is determined by the doctor based on the patient’s condition.
For greater effectiveness of treatment, it is important to keep a distance from other people, use individual things, maintain bed rest and the necessary nutrition. It is preferable to enrich the diet with fiber, fruits, vegetables and protein products. It is recommended to drink at least 1.5 liters of liquid per day.
Prevention of bird flu
To minimize the likelihood of contracting bird flu, you should take the following precautions:
- Handle poultry and eggs thoroughly. To do this, you need to heat the food to 55-65 degrees for half an hour.
- After treatment, you need to wash your hands well with soap for 15-20 seconds.
- It is better to have a separate board for cutting meat. Dishes should be washed under hot water and detergents.
- Use a food thermometer to ensure the desired temperature is maintained.
- Don't eat raw eggs.
- Do not communicate with people who are suspected of having the flu. If contact does occur, then you should monitor your health and immediately consult a doctor when the first symptoms appear.
- Take antiviral medications and vitamin complexes.
- During an epidemic, wear a gauze mask.
- When traveling to a country where cases of bird flu infection occur, it is worth getting vaccinated, and if possible, it is better to reschedule the trip.
WHO activities
WHO, through the WHO GISRS system and in collaboration with other partners, monitors influenza activity globally, makes recommendations on seasonal influenza vaccine formulations twice a year for the northern and southern hemispheres, and assists countries with tropical and subtropical climates in the selection of vaccine products (for northern and southern hemispheres) and decisions regarding the timing of vaccination campaigns and supports Member States in developing prevention and control strategies.
WHO works to strengthen national, regional and global capacity to respond to influenza (including diagnosis, antiviral susceptibility monitoring, disease surveillance and outbreak response), increase vaccination coverage in high-risk populations and ensure preparedness for next influenza pandemic.
(1) Estimates of US influenza-associated deaths made using four different methods. Thompson WW, Weintraub E, Dhankhar P, Cheng OY, Brammer L, Meltzer MI, et al. Influenza Other Respi Viruses. 2009;3:37-49
(2) Global burden of respiratory infections due to seasonal influenza in young children: a systematic review and meta-analysis. Nair H, Abdullah Brooks W, Katz M et al. Lancet 2011; 378: 1917–3 (3) WHO recommended surveillance standards, Second edition.
Is it possible to get infected from someone who has had the flu?
If a person has coped with the disease, his fever has passed and all signs of the flu are absent, he is safe for others. Influenza does not have an asymptomatic course, unlike some other acute respiratory viral infections, and does not become chronic. Elimination - the final elimination of the infection in the body occurs along with the symptoms. But the final conclusion whether the patient has recovered or not can only be made by a doctor. Those who have the flu themselves often treat their condition subjectively: they do not notice residual wheezing in the bronchi, irregularly record their body temperature, or suppress the signs of infection with antipyretics.
Before going out into the public, a person who has recovered from the disease must wait 2-3 days without using NSAIDs and other medications, then consult with a specialist who will assess his condition. Only then can you return to normal life.
Diagnostics
In most cases, human influenza is clinically diagnosed. However, during periods of low activity of influenza viruses and in the absence of epidemics, infection caused by other respiratory viruses, such as rhinovirus, respiratory syncytial virus, parainfluenza virus, and adenovirus, may also present as influenza-like illness, making it difficult to clinically differentiate influenza from other pathogens.
Adequate respiratory samples must be collected and a laboratory diagnostic test performed to make a definitive diagnosis. The first critical step for laboratory detection of influenza viral infections is the proper collection, storage, and transportation of respiratory specimens. Typically, laboratory confirmation of influenza viruses in secretions from the throat, nose, and nasopharynx or in aspirates or tracheal washings is performed by direct detection of antigens, virus isolation, or detection of influenza-specific RNA by reverse transcriptase polymerase chain reaction (RT-PCR). There are a number of laboratory manuals published and updated by WHO (3).
Rapid diagnostic tests are used in clinics to detect influenza, but they have low sensitivity compared to RT-PCR methods and the reliability of their results depends largely on the conditions in which they are used.
Epidemiology
People get the flu at any age, but there are groups of people at increased risk .
- Those at increased risk of developing severe illness or complications from infection are pregnant women, children under 59 months of age, older adults, and people with chronic health conditions (such as chronic heart, lung, and kidney disease, metabolic disorders, neurodevelopmental disorders, liver disease, and blood) and people who are immunocompromised (as a result of HIV/AIDS, chemotherapy or steroid treatment, or due to malignancy).
- Healthcare workers are at high risk of becoming infected with influenza virus during their contact with patients and may contribute to further transmission, especially to people at risk.
Transmission of seasonal influenza infection occurs easily and quickly, especially in crowded areas, including schools and boarding schools.
When an infected person coughs or sneezes, small droplets containing the virus (infectious droplets) become airborne and can travel up to one meter and infect nearby people who inhale them. The infection can also be transmitted through hands contaminated with influenza viruses. To prevent transmission of infection when coughing, cover your mouth and nose with a tissue and wash your hands regularly. In temperate climates, seasonal epidemics occur primarily during the winter season, while in tropical regions, influenza viruses circulate throughout the year, resulting in less regular epidemics. Seasonal epidemics and disease burden
The period of time from infection to the development of the disease, known as the incubation period , lasts about 2 days, but can vary from 1 to 4 days.
Recovery from influenza in adults
After an influenza infection, most patients experience increased weakness, lethargy, and sleep disturbances for a long time. All these are manifestations of asthenic syndrome. As a rule, asthenia is expressed in increased exhaustion of mental and physical strength. The main symptoms in this case will be increased fatigue, tiredness and weakness.
After the disease, the patient often feels emotional instability, which is expressed in frequent mood swings and irritability. A feeling of anxiety, restlessness, and internal tension appears. The ability for prolonged mental and physical stress is lost. Autonomic disorders may also appear. Frequent headaches are a concern, sweating increases, appetite worsens, there is a feeling of interruptions in the functioning of the heart, memory deteriorates, and sleep is disturbed. Daytime sleepiness may occur.
With asthenic syndrome, it is necessary to take care of an organized work and rest schedule and minimize stress. It is necessary to adhere to a daily routine, do not forget about moderate physical activity, and try to spend more time in the fresh air. The diet must be balanced, contain the required amount of proteins, fats, carbohydrates, vitamins and microelements with the obligatory inclusion of fresh vegetables and fruits in the menu. On the recommendation of a doctor, you can take vitamin and mineral complexes.
Reference and information material
Author of the article
Gerasimenko Igor Olegovich
General doctor
- R.Z.Gatich, L.V. Kolobukhina, E.I. Isaeva, E.I. Burtseva, T.G. Orlova, F.V. Voronina, V.V. Malinovskaya “Efficacy of Viferon for influenza in adult patients”, Russian Medical Journal No. 14, 2004.
Sources:
https://cyberleninka.ru/ [ii]https://umedp.ru/ [iii] https://www.influenza.spb.ru/ [iv] https://ru.wikipedia.org/ [v] https://eduherald.ru/ [vi] https://rospotrebnadzor.ru/
Loading...
Take other surveys