Types of leukocytes
The leukocyte formula reflects the ratio of five main types: lymphocytes, monocytes, neutrophils, basophils, eosinophils. Different types of white blood cells are different in structure and purpose. Depending on whether they contain granules that are capable of perceiving color, leukocytes are of two types: granulocytes, agranulocytes.
Granulocytes include:
- basophils - can perceive alkaline color;
- eosinophils – acidic;
- neutrophils - both types of dyes.
Agranulocytes include:
- two types of lymphocytes (B- and T-lymphocytes);
- monocytes.
What is the difference between KAK and OAK?
General blood test and clinical analysis are one and the same. One set of parameters of shaped elements is studied. Blood for both studies is taken from both a vein and a finger.
A referral for analysis is issued almost every time a person appears in the hospital, since it allows you to collect comprehensive basic information about the functioning of the body, and then, if a problem is detected, refer the patient to a specialist. Typically, a general examination is prescribed by a general practitioner.
The difference between a general blood test and a clinical one is in the name. The first to appear was clinical analysis, however, due to the dissonant abbreviation - HOW, over time it was replaced by OAK, which sounds more decent.
Functions of white cells
Lymphocytes. T lymphocytes destroy foreign microorganisms and cancer cells. B lymphocytes are responsible for producing antibodies.
Monocytes. They participate in phagocytosis, directly neutralizing foreign bodies, as well as the immune response and tissue regeneration.
Eosinophils. Capable of active movement and phagocytosis. They actively participate in the formation of inflammatory and allergic reactions, capturing and releasing histamine.
Basophils. They ensure the migration of other types of leukocytes into tissues to the site of inflammation and take part in allergic reactions.
Neutrophils. The main purpose is phagocytic protection, that is, the absorption of foreign bodies. In addition, they release bactericidal substances.
What is studied in general KLA?
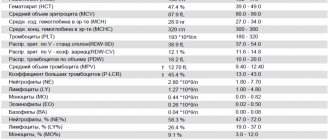
KLA includes the study of the following parameters:
- Hemoglobin level. Responsible for saturating the body with oxygen and transfers it from the lungs to the rest of the cells of the body, nourishing them. If the reading is low for no obvious reason, then the patient has anemia, or anemia.
- Erythrocytes are red blood cells that contain hemoglobin. If their number is less than normal, anemia is possible.
- The color index is a way to determine the amount of hemoglobin in red blood cells. It makes them red, so the saturation should be a certain shade, indicating that there is enough hemoglobin.
- Reticulocytes are the “embryos” of red blood cells. “Growing up,” they replace “used up” cells for the full functioning of the system.
- Platelets are formed cells responsible for ensuring that the blood clots at the right time. If there are not enough of them, this indicates a blood clotting disorder. The indicator may fall during menstruation or while a woman is pregnant. Increases after intense exercise.
- ESR is an abbreviation that stands for erythrocyte sedimentation rate. If the indicator is too high, then the patient has an infection, acute inflammation, or has been poisoned.
- Leukocytes are known as white blood cells. They “represent” immunity because they counteract viruses and bacteria. If the level is elevated, then there is an inflammatory process in the body, to which the immune system reacts.
- Band and segmented neutrophils are checked.
- Eosinophils are formed elements from the “squad” of leukocytes. An increase in the number indicates either the presence of parasites or an allergic reaction.
- Basophils are a subtype of leukocytes, indicating an increase in the number in the blood of an inflammatory process.
- Lymphocytes are elements that represent the acquired immune system.
- Monocytes - large white blood cells - are the main “army” of the immune system, fighting large and simple infections of the general spectrum. They take the brunt of the inflammatory process.
Read also: What does a high level of antibodies to thyroglobulin mean and why is it checked?
A general practitioner, studying the indicators of a general, or clinical, blood test, will understand the approximate localization of the problem and refer the patient for examination to a specialist.
Normal leukogram values
The leukocyte formula of the blood of healthy adults is as follows:
| Kinds | Content % | Absolute value (number of cells X 10?/l) |
| Lymphocytes | 19-37 | 1,2-3 |
| Monocytes | 3-11 | 0,09-0,6 |
| Band neutrophils (immature) | 1-6 | 0,04-0,3 |
| Segmented neutrophils | 47-72 | 2-5,5 |
| Basophils | 0-1 | 0-0,065 |
| Eosinophils | 0,5-5 | 0,02-0,3 |
Changes in the leukogram are usually denoted by terms with specific endings. As the level increases, endings such as “oz” (“ez”) or “ia” are added to the name of a particular type of leukocyte. For example: lymphocytosis, eosinophilia, monocytosis, etc. When the level of leukocytes decreases, it is customary to add the ending “singing” to the name: lymphopenia, neutropenia, eosinopenia, etc.
In this case, a distinction is made between relative and absolute change. In the first case, we are talking about a deviation from the norm in the percentage of leukocytes. In the second, they talk about a deviation from the norm both in percentage terms and in absolute terms, which is understood as a change in the total number of cells per unit volume of blood.
Leukocytes differ in their structure and purpose
It should be said that the leukocyte formula depends on age. This must be taken into account when assessing it during examination and diagnosis of diseases in children.
Analysis for tumor markers
Today, comprehensive cancer screening is not possible without laboratory tests, in particular, blood tests for tumor markers. Regular testing allows you to detect a serious disease at an early stage.
Indications for passing
The test is prescribed by a doctor both during a course of treatment to assess its effectiveness and to prevent relapses.
If you conduct an examination yourself, without a doctor’s prescription, its results should be provided to specialists for correct interpretation!
Analysis results
It is important to understand that diagnosing cancer cannot be based solely on the results of laboratory blood tests, since benign neoplasms and inflammatory processes can also provoke an increase in the level of tumor markers.
Only a comprehensive study under the supervision of experienced doctors will help you reliably identify a malignant tumor at an early stage.
Our clinic specialists will provide you with a sufficient set of examinations to monitor your health.
How to determine
The leukocyte formula is calculated by a laboratory assistant by viewing the blood under a microscope (leukogram count per hundred cells).
In addition, a hematology automatic analyzer is used. In case of deviations from the norm, a microscopic examination of the smear is additionally carried out, while the morphology of the cells is described and the leukogram is clarified.
The use of automatic equipment allows you to obtain the most accurate result: more than 2000 cells can be analyzed, while under a microscope - a maximum of 200. When examined using an analyzer, the result is more objective.
Automatic counting also has a drawback: the inability to divide neutrophils into segmented and band neutrophils. But in the case of a large number of young forms, the equipment records a shift to the left.
Why are there multiple tests?
When reading the indicators of a clinical blood test and a general analysis, the difference or similarity is not difficult to understand. Why is there no single study that covers all aspects?
Blood is a multipolar fluid, an indicator of the state of the body. This is a transport and protective system, so it contains cells responsible for human immunity and health. There are also hormones that “manage” the work of organs, waste products of cells, oxygen, and beneficial substances that they feed on. Blood, in addition to its base - plasma, includes hundreds of elements that serve or are removed from the body.
To obtain information about a specific parameter, for example: the amount of insulin, which indicates the functioning of the pancreas, an analysis is needed to study this parameter; there is no point in studying all the blood. Each referral or suspicion of disease requires research only in the required area. The results of a general blood test or clinical blood test refer to one type of research.
Reasons for changes in leukogram
An increase in the level of lymphocytes (lymphocytosis) is observed in the following pathologies:
- acute viral infections: chickenpox, measles, mononucleosis, rubella;
- chronic bacterial infections: syphilis, brucellosis, tuberculosis;
- lymphomas, lymphosarcoma, lymphocytic leukemia;
- hyperthyroidism (thyrotoxicosis);
- adrenal insufficiency;
- folate deficiency anemia;
- aplastic and hypoplastic anemia.
Lymphocytopenia can develop for the following reasons:
- acute infections;
- lymphogranulomatosis;
- systemic lupus erythematosus;
- renal failure;
- immunodeficiency;
- radiation sickness (acute form);
- taking corticosteroids.
An increase in the level of neutrophils in the blood (neutrophilia) is observed in the following conditions:
- bleeding is acute;
- intoxication;
- bacterial diseases in acute forms;
- taking corticosteroids;
- tissue necrosis.
The content of neutrophils decreases for the following reasons:
- bacterial infections: typhoid fever, brucellosis, tularemia;
- viral infections: measles, hepatitis, rubella;
- toxic effects to which the bone marrow is exposed: drugs, ionizing radiation;
- autoimmune diseases;
- hypersensitivity to medications;
- Benign chronic neutropenia is hereditary.
Monocytosis, in which the level of monocytes in the blood is increased, may indicate the following disorders:
- subacute, chronic infections caused by bacteria;
- hemoblastoses;
- systemic autoimmune diseases: rheumatoid arthritis, lupus erythematosus, sarcoidosis;
- parasitic infections.
A low level of monocytes is assessed in combination with lymphocyte indicators, which is important when diagnosing pulmonary tuberculosis.
Basophilia (increased levels of basophils in the blood) is observed in chronic myeloid leukemia and erythremia.
An increased level of eosinophils is observed in the following conditions:
- allergies;
- Loeffler's endocarditis;
- scarlet fever;
- parasitic infections;
- chronic skin diseases: eczema, psoriasis;
- eosinophilic leukemias;
- recovery phase of infectious diseases.
Causes of low eosinophil levels (eosinopenia) may include:
- typhoid fever;
- increased adrenocorticosteroid activity.
Clinical blood test is a laboratory study assessing the quantitative and qualitative characteristics of all classes of blood cells, including a cytological examination of a peripheral blood smear to calculate the percentage of leukocyte varieties and determine the erythrocyte sedimentation rate.
Synonyms Russian
Complete blood count (CBC), hemogram, CAC, complete blood count.
English synonyms
Complete Blood Count (CBC), Hemogram, CBC with White Blood Cell Differential Count, Peripheral Blood Smear, Blood Film Examination.
What biomaterial can be used for research?
Venous blood, capillary blood.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Children under 1 year of age should not eat for 30-40 minutes before the test.
- Children aged 1 to 5 years should not eat for 2-3 hours before the test.
- Do not eat for 8 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
A clinical blood test is performed to diagnose quantitative and qualitative changes in the formed elements - blood cells: red blood cells, leukocytes and platelets. Their changes may be caused by disturbances in the hematopoietic process, but most often they are reactive in nature - they reflect the reaction of hematopoiesis to other pathological conditions and diseases. Therefore, a clinical blood test is one of the most common routine tests and is used by doctors of various specialties; it plays a leading role in the primary diagnostic search.
Both venous and capillary blood can be used for the study, with venous blood being preferable. The collection is performed using a vacuum system, most often from the veins in the elbow. A special tube called a vacutainer already contains an anticoagulant (EDTA), which prevents blood clotting. The volume of blood drawn into the vacutainer must correspond to the mark on it - this way the required concentration of the anticoagulant is achieved, which prevents the formation of microclots and, as a result, incorrect calculation of the number of cellular elements and distortion of their morphological structure.
Currently, a clinical blood test is most often performed on a hematology analyzer - a high-tech device that can detect and automatically calculate more than 30 blood characteristics, including counting formed elements, including the main populations of leukocytes. The operating principle of hematology analyzers is based on the passage of a cell suspension through a sensitive element - a laser beam or electric current. Each cell refracts the laser or changes the resistance of the electric current; these changes are proportional to the size of the cell, which is what the analyzer is based on to distinguish them.
If there are deviations in the results of a study on a hematology analyzer, the laboratory diagnostics doctor performs a morphological study of the blood smear. Smear microscopy was included initially in this study. To visually count the formed elements, one or two drops of blood are dripped onto a glass slide, another glass is used to smear it into a thin layer in one motion and is fixed with special substances. The smears are then stained with dyes to make it easier to distinguish and visualize cells and are examined by a doctor under a microscope. Traditionally, the count is carried out per hundred cells and the resulting numbers are recorded as percentages. Knowing the total number of leukocytes, percentages can be converted into absolute values, which much more objectively reflect the state of the leukocyte population.
Parameters determined in the study
Red blood cells are the most numerous blood cells; their main function is the transport of oxygen, which they perform with the help of a special protein they contain - hemoglobin. The hematology analyzer determines the number of red blood cells, hemoglobin content, hematocrit and, based on this, calculates a number of characteristics - the so-called red blood cell indices.
Red blood cells (RBC, Red Blood Cell) are anucleate cells, formed in the bone marrow from reticulocytes, and have the shape of a biconcave disk, which allows them to achieve the maximum possible surface area for binding oxygen. Red blood cells have a diameter of 7-10 micrometers, they are elastic and can easily change shape to safely pass through the smallest vessels - capillaries. In a blood smear they appear as pale red round elements with a clearing in the center. The unit of measurement is 1012 per liter (trillion cells per liter).
Hemoglobin (HGB) is a protein, the main component of red blood cells, which has an affinity for oxygen, which ensures the transport function of red blood cells. Oxygenated hemoglobin gives red blood cells and blood in general their red color.
Hematocrit (HCT) – characterizes the ratio of the volume of red blood cells and plasma. This is a calculation parameter - the hematology analyzer calculates the volume of red blood cells from their number and the average cell volume (MCV).
Mean Corpuscular Volume (MCV, Mean Corpuscular Volume) – is calculated by the analyzer by dividing the sum of cell volumes by the number of red blood cells. It may have a normal value if both microcytosis and macrocytosis are present in the blood. In such situations, you should pay attention to the RDW parameter. The unit of measurement is femtoliter.
The average hemoglobin content in an erythrocyte (MCH, Mean Corpuscular Hemoglobin) – reflects the degree of saturation of the erythrocyte with hemoglobin. Calculated by dividing the hemoglobin concentration by the number of red blood cells.
The average hemoglobin concentration in an erythrocyte (MCHC, Mean Corpuscular Hemoglobin Concentration) also characterizes the saturation of an erythrocyte with hemoglobin. Calculated by dividing hemoglobin by hematocrit.
Distribution of erythrocytes by volume (RDW, Red Cell Distribution Width) - characterizes the degree of variability of erythrocyte volume - anisocytosis. If there is a population of red blood cells in the blood with an altered, but fairly uniform size, RDW values may remain normal. With pronounced differences in the volume of red blood cells, when MCV, which characterizes the average volume of all cells, is normal, RDW will be increased.
Platelets (PLT, Platelet) are blood cells involved in stopping bleeding by forming blood clots. They are not cells; they are fragments of the cytoplasm of bone marrow megakaryocytes. Diameter 2-4 microns.
Mean platelet volume (MPV, Mean Platelet Volume) – platelet volume decreases as cells age, so an increase in this parameter indicates a predominance of young platelets in the population.
Platelet distribution by volume (PDW, Platelet Distribution Width) – characterizes the variability of platelet sizes.
Leukocytes (WBC, White Blood Cell) are a heterogeneous population of nucleated blood cells, the main function of which is to protect the body from foreign agents. Leukocytes include cells of the granulocytic (eosinophils, basophils, neutrophils), monocyte and lymphoid (T- and B-lymphocytes) series. Modern analyzers can differentiate the main five types of leukocytes, but smear microscopy is still the most accurate method for assessing the leukocyte population, as it allows not only to determine the number of different leukocytes, but also to identify changes in their morphology, as well as detect atypical cells.
The percentage of different types of leukocytes in a blood smear is called the leukocyte formula . Staining of blood smears allows you to differentiate 5 types of leukocytes due to different staining of the nuclei and intracellular space (cytoplasm):
- Neutrophils are granulocytic leukocytes: their cytoplasm contains granules with specific active substances that allow them to perform their protective functions (capture and destroy foreign objects). Neutrophils also have a nucleus, according to the structure of which they are divided into band-nuclear and segmented (this is the final stage of maturation following the band-nucleus, at which the nucleus is divided by constrictions into 4-5 lobes). When stained, neutrophil granules turn purple, which, together with the peculiarity of the nucleus, allows them to be distinguished from other granulocytes.
- Eosinophils are granulocytes involved in allergic reactions and antiparasitic immunity. Their granules contain mediators of allergy and inflammation. Eosinophils have a two-segmented nucleus, and their granules are orange-pink in color.
- Basophils are granulocytes that take an active part in immediate allergic reactions. They have an S-shaped non-segmented nucleus, which is often not visible due to large granules of intense blue color containing allergy mediators.
- Lymphocytes are cells with a large nucleus, practically devoid of cytoplasm. Their nucleus is colored intense purple-violet, and the cytoplasm is blue-blue. Lymphocytes participate in more complex immune reactions associated with the recognition of their own and foreign antigens.
- Monocytes are relatively large leukocytes containing an unsegmented bean-shaped nucleus and, unlike lymphocytes, a large amount of cytoplasm. When stained, the nucleus becomes purplish-red, and the cytoplasm is a cloudy bluish-gray. The main function of monocytes is phagocytosis, that is, the absorption and digestion of microorganisms, their own dying cells, etc.
The above types of leukocytes are found normally in a peripheral blood smear. In some diseases, cells that normally should not be in the smear may enter the blood from the bone marrow: for example, blasts are the morphological substrate of acute leukemia. In the conclusion to the study, the number and, if possible, morphological features of atypical cells must be indicated.
In addition to counting leukocytes, microscopy evaluates the morphological characteristics of red blood cells - their size, shape. These parameters are important in the diagnosis of various acquired and congenital anemias.
Erythrocyte sedimentation rate . The test is based on the ability of red blood cells to settle under the influence of gravity in blood that is deprived of the ability to clot. Normally, red blood cells settle slowly; this process is accelerated by agglutination - the sticking of red blood cells to each other, which leads to an increase in the mass of settling particles. Ordinary red blood cells have a negative charge on the membrane, which helps them repel each other. In infectious-inflammatory, autoimmune and some tumor (especially paraproteinemic hemoblastoses) diseases, the protein composition of the plasma changes towards an increase in the content of proteins (for example, immunoglobulins). All protein molecules reduce the membrane charge of red blood cells, promoting their gluing to each other and increasing the rate of sedimentation. The test is carried out for an hour, the height of the resulting sediment is measured in millimeters.
What is the research used for?
- To assess general health (routine medical examinations, screening examinations, etc.);
- For diagnostics at the first stage of a wide range of diseases that may manifest themselves as changes in the characteristics of peripheral blood;
- Monitoring of peripheral blood parameters in diseases accompanied by quantitative and qualitative changes;
- To monitor the toxicity of treatment if the methods used may affect the composition of peripheral blood (for example, chemotherapy, radiation therapy).
When is the study scheduled?
- During screening examinations;
- As a primary diagnosis for suspected diseases that may be accompanied by changes in the cellular composition of the blood;
- In the presence of hematopoietic diseases;
- To monitor the effectiveness and toxicity of treatment.
What do the results mean?
Reference values
Leukocytes
| Age | Reference values |
| Less than 1 year | 6 - 17.5 *10^9/l |
| 1-2 years | 6 - 17 *10^9/l |
| 2-4 years | 5.5 - 15.5 *10^9/l |
| 4-6 years | 5 - 14.5 *10^9/l |
| 6-10 years | 4.5 - 13.5 *10^9/l |
| 10-16 years | 4.5 - 13 *10^9/l |
| More than 16 years | 4 - 10 *10^9/l |
Red blood cells
| Age | Floor | Red blood cells, *10 ^12/ l |
| 3,9-5,9 | ||
| 14 days – 1 month. | 3,3-5,3 | |
| 1-4 months | 3,5-5,1 | |
| 4-6 months | 3,9-5,5 | |
| 6-9 months | 4-5,3 | |
| 9-12 months | 4,1-5,3 | |
| 1-3 years | 3,8-4,8 | |
| 3-6 years | 3,7-4,9 | |
| 6-9 years | 3,8-4,9 | |
| 9-12 years | 3,9-5,1 | |
| 12-15 years | male | 4,1-5,2 |
| female | 3,8-5 | |
| 15-18 years old | male | 4,2-5,6 |
| female | 3,9-5,1 | |
| 18-45 years old | male | 4,3-5,7 |
| female | 3,8-5,1 | |
| 45-65 years | male | 4,2-5,6 |
| female | 3,8-5,3 | |
| > 65 years old | male | 3,8-5,8 |
| female | 3,8-5,2 |
Hemoglobin
| Age | Floor | Hemoglobin, g / l |
| 134-198 | ||
| 14 days – 1 month. | 107-171 | |
| 1-2 months | 94-130 | |
| 2-4 months | 103-141 | |
| 4-6 months | 111-141 | |
| 6-9 months | 114-140 | |
| 9-12 months | 113-141 | |
| 1-5 years | 110-140 | |
| 5-10 years | 115-145 | |
| 10-12 years | 120-150 | |
| 12-15 years | male | 120-160 |
| female | 115-150 | |
| 15-18 years old | male | 117-166 |
| female | 117-153 | |
| 18-45 years old | male | 132-173 |
| female | 117-155 | |
| 45-65 years | male | 131-172 |
| female | 117-160 | |
| > 65 years old | male | 126-174 |
| female | 117-161 |
Hematocrit
| Age | Floor | Hematocrit, % |
| 41-65 | ||
| 14 days – 1 month. | 33-55 | |
| 1-2 months | 28-42 | |
| 2-4 months | 32-44 | |
| 4-6 months | 31-41 | |
| 6-9 months | 32-40 | |
| 9-12 months | 33-41 | |
| 1-3 years | 32-40 | |
| 3-6 years | 32-42 | |
| 6-9 years | 33-41 | |
| 9-12 years | 34-43 | |
| 12-15 years | male | 35-45 |
| female | 34-44 | |
| 15-18 years old | male | 37-48 |
| female | 34-44 | |
| 18-45 years old | male | 39-49 |
| female | 35-45 | |
| 45-65 years | male | 39-50 |
| female | 35-47 | |
| > 65 years old | male | 37-51 |
| female | 35-47 |
Mean erythrocyte volume (MCV)
| Floor | Age | Reference values |
| Less than 1 year | 71 – 112 fl | |
| 1-5 years | 73 – 85 fl | |
| 5-10 years | 75 – 87 fl | |
| 10-12 years | 76 – 94 fl | |
| Female | 12-15 years | 73 – 95 fl |
| 15-18 years old | 78 – 98 fl | |
| 18-45 years old | 81 – 100 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl | |
| Male | 12-15 years | 77 – 94 fl |
| 15-18 years old | 79 – 95 fl | |
| 18-45 years old | 80 – 99 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl |
Average hemoglobin content in erythrocytes (MCH)
| Age | Floor | Reference values |
| 30 - 37 pg | ||
| 14 days - 1 month. | 29 - 36 pg | |
| 1 - 2 months | 27 - 34 pg | |
| 2 - 4 months | 25 - 32 pg | |
| 4 - 6 months | 24 - 30 pg | |
| 6 - 9 months | 25 - 30 pg | |
| 9 - 12 months | 24 - 30 pg | |
| 1 – 3 years | 22 - 30 pg | |
| 36 years | 25 - 31 pg | |
| 6 – 9 years | 25 - 31 pg | |
| 9-15 years | 26 - 32 pg | |
| 15-18 years old | 26 - 34 pg | |
| 18-45 years old | 27 - 34 pg | |
| 45-65 years | 27 - 34 pg | |
| > 65 years old | female | 27 - 35 pg |
| > 65 years old | male | 27 - 34 pg |
Mean erythrocyte hemoglobin concentration (MCHC)
| Age | Reference values |
| Less than 1 year | 290 – 370 g/l |
| 1-3 years | 280 – 380 g/l |
| 3-12 years | 280 – 360 g/l |
| 12-19 years old | 330 - 340 g/l |
| More than 19 years | 300 – 380 g/l |
Platelets
| Age | Reference values |
| Less than 10 days | 99 - 421 *10^9/l |
| 10 days – 1 month | 150 – 400 *10^9/l |
| 1-6 months | 180 – 400 *10^9/l |
| 6 months – 1 year | 160 - 390 *10^9/l |
| 1-5 years | 150 – 400 *10^9/l |
| 5-10 years | 180 - 450 *10^9/l |
| 10-15 years | 150 – 450 *10^9/l |
| More than 15 years | 150 – 400 *10^9/l |
RDW-SD (red blood cell volume distribution, standard deviation): 37 - 54.
RDW-CV (red blood cell volume distribution, coefficient of variation)
| Age | RDW-CV, % |
| 14,9 — 18,7 | |
| > 6 months | 11,6 — 14,8 |
Platelet distribution by volume (PDW): 10 - 20 fL.
Mean platelet volume (MPV): 9.4 - 12.4 fL.
Large platelet count ratio (P-LCR): 13 – 43%.
Neutrophils (NE)
| Up to 4 years | 1.5 - 8.5 *10^9/l |
| 4-8 years | 1.5 - 8 *10^9/l |
| 8-16 years | 1.8 - 8 *10^9/l |
| More than 16 years | 1.8 - 7.7 *10^9/l |
Lymphocytes (LY)
| Up to 1 year | 2 - 11 *10^9/l |
| 1-2 years | 3 - 9.5 *10^9/l |
| 2-4 years | 2 - 8 *10^9/l |
| 4-6 years | 1.5 - 7 *10^9/l |
| 6-8 years | 1.5 - 6.8 *10^9/l |
| 8-10 years | 1.5 - 6.5 *10^9/l |
| 10-16 years | 1.2 - 5.2 *10^9/l |
| More than 16 years | 1 - 4.8 *10^9/l |
Monocytes (MO)
| Up to 1 year | 0.05 - 1.1 *10^9/l |
| 1-2 years | 0.05 - 0.6 *10^9/l |
| 2-4 years | 0.05 - 0.5 *10^9/l |
| 4-16 years | 0.05 - 0.4 *10^9/l |
| More than 16 years | 0.05 - 0.82 *10^9/l |
Eosinophils (EO)
| Up to 1 year | 0.05 - 0.4 *10^9/l |
| 1-6 years | 0.02 - 0.3 *10^9/l |
| More than 6 years | 0.02 - 0.5 *10^9/l |
Basophils (BA): 0 - 0.08 *10^9/l.
Neutrophils, % (NE%)
| Up to 1 year | 16 — 45 % |
| 1-2 years | 28 — 48 % |
| 2-4 years | 32 — 55 % |
| 4-6 years | 32 — 58 % |
| 6-8 years | 38 — 60 % |
| 8-10 years | 41 — 60 % |
| 10-16 years | 43 — 60 % |
| More than 16 years | 47 — 72 % |
Lymphocytes,% (LY%)
| Up to 1 year | 45 — 75 % |
| 1-2 years | 37 — 60 % |
| 2-4 years | 33 — 55 % |
| 4-6 years | 33 — 50 % |
| 6-8 years | 30 — 50 % |
| 8-10 years | 30 — 46 % |
| 10-16 years | 30 — 45 % |
| More than 16 years | 19 — 37 % |
Monocytes, % (MO%)
| Up to 1 year | 4 — 10 % |
| 1-2 years | 3 — 10 % |
| More than 2 years | 3 — 12 % |
Eosinophils,% (EO%)
| Up to 1 year | 1 — 6 % |
| 1-2 years | 1 — 7 % |
| 2-4 years | 1 — 6 % |
| More than 4 years | 1 — 5 % |
Basophils,% (BA%): 0 - 1.2%.
Erythrocyte sedimentation rate (photometry)
| Male | Up to 15 years | 2 - 20 mm/h. |
| 15-50 years | 2 - 15 mm/h. | |
| More than 50 years | 2 - 20 mm/h. | |
| Female | Up to 15 years | 2 - 20 mm/h. |
| 15-50 years | 2 - 20 mm/h. | |
| More than 50 years | 2 - 30 mm/h. |
A clinical blood test includes a relatively large number of parameters that must be interpreted in combination. Most often, based on the results of the hemogram, the range of studies necessary to clarify the causes of the changes identified in it is determined.
Changes in erythrocyte parameters. A decrease in the level of hemoglobin and erythrocytes are laboratory manifestations of anemia, and changes in erythrocyte indices characterize its pathogenetic variant and help clarify the causes. Increased levels of red blood cells and hemoglobin may indicate a myeloproliferative disorder (polycythemia vera), but also occurs as a compensatory reaction in active smokers, people with respiratory diseases and heart defects.
Changes in platelets. An increase in platelet count may be a manifestation of essential thrombocythemia (a hematological disease characterized by excess production of platelets in the bone marrow), but also occurs as a compensatory reaction after massive bleeding. A decrease in platelet count is observed with an enlarged spleen, immune thrombocytopenia, as well as aplastic anemia, where it will be combined with a decrease in red blood cells and leukocytes.
Changes in leukocytes. Leukocytosis is considered a manifestation of infectious and inflammatory diseases, and the appearance in the blood smear of a large number of young forms of neutrophils - band and even metamyelocytes (this is called a shift of the leukocyte formula to the left) is characteristic. But too high an increase in the level of leukocytes may be a consequence of an oncohematological disease - acute or chronic leukemia. In this case, morphologically changed cells are found in the blood smear, as well as immature forms of leukocytes (blasts), which normally should not enter the peripheral blood. Leukopenia can accompany severe infectious diseases and in this case characterize the depletion of the leukocyte lineage, and be a consequence of inhibition of bone marrow hematopoiesis, for example, against the background of tumor metastases in the bone marrow.
Erythrocyte sedimentation rate. It is a nonspecific parameter indicating changes in the protein composition of plasma. Most often this is caused by infectious-inflammatory, autoimmune and oncological diseases.
Leukogram shift
Modern automatic blood analyzers quickly and accurately calculate the complete leukocyte formula, which greatly facilitates diagnosis
When the leukogram is deciphered, nuclear shifts are taken into account. These are changes in the ratio of mature and immature neutrophils. In the blood formula, the different forms of neutrophils are listed in order from young to mature (from left to right).
There are three types of shifts: left, left with rejuvenation, and right.
With a left shift, myelocytes and metamyelocytes are present in the blood. This change occurs through the following processes:
- acute inflammation: pyelonephritis, prostatitis, orchitis;
- purulent infections;
- acidosis;
- bleeding is acute;
- poisoning with toxins;
- high physical activity.
With a left shift with rejuvenation, forms such as myelocytes, metamyelocytes, promyelocytes, myeloblasts, and erythroblasts can be found in the blood. This is observed in conditions such as:
- leukemia (chronic, acute);
- erythroleukemia;
- metastases;
- myelofibrosis;
- coma.
Video about the types and functions of leukocytes:
With a decrease in the number of band (immature) neutrophils and an increase in the level of segmented (mature forms containing 5-6 segments), they speak of a right shift. With such a change in the leukogram, we can talk about the following pathologies and conditions:
- liver and kidney diseases;
- megaloblastic anemia;
- consequences of blood transfusion;
- radiation sickness;
- vitamin B12 deficiency, folate deficiency anemia.
The degree of shift is assessed using a special index, which is determined by the ratio of the total number of all young neutrophils (myelocytes, metamyelocytes, promyelocytes, band neutrophils) to mature segmented ones. The norms for healthy adults are in the range of 0.05-0.1.
What kind of research is this?
What is a clinical blood test and complete blood count? The answer is simple - the most common studies that cover parameters that allow the doctor to judge the condition of the body.
There are “formed elements” in the blood, which perform basic functions. There should be an amount of each particle depending on the age and gender of the person. If they go beyond the limits, then this indicates that something in the body is not happening as it should.
This analysis is indispensable in the treatment of colds. Often, when characteristic signs appear, a person does not go to the hospital, but goes to the pharmacy, buys an antiviral and takes unnecessary pills, develops complications and goes to the hospital with a “bunch of troubles” that are not easy to cure. The CBC will determine whether bacteria or viruses are to blame for the illness. So what is the difference between clinical and general blood tests?
Read also: Causes of low or high hemoglobin and red blood cells in the blood, methods of diagnosis and therapy
Immunological blood test
Few people know what blood tests there are from the point of view of the human immunological system, since these tests are not so common. As a rule, such a blood test provides information about the immunodeficiency virus in the human body and is anonymous, since it is carried out at the request of the patient. For sampling, blood taken from a vein on an empty stomach is used, from which serum is obtained for testing by centrifugation. In addition, the study of blood serum can detect a number of sexually transmitted diseases (syphilis, herpes, chlamydia), as well as all types of hepatitis, measles, rubella, mumps and toxoplasmosis.
Basically, for ELISA analysis, the biological material being studied is blood, however, cerebrospinal fluid, vitreous contents, amniotic fluid, etc. can be examined.
What is immunoglobulin (antibody)?
Immunoglobulins are immune molecules that can bind to and neutralize most infectious pathogens and toxins in the body. In this case, the most important characteristic of immunoglobulins is their specificity, that is, the ability to bind to a specific antigen. It is this property that is used to conduct a blood test for immunoglobulin.
There are five types of immunoglobulins, but the most studied are immunoglobulins A, M, and G. Immunoglobulins M and G show their activity in the blood. Immunoglobulins A are a kind of barrier on the surface of the mucous membranes, as they are present there in large quantities.
An immunological blood test allows you to determine the type of immunoglobulins, thanks to which ELISA allows you not only to diagnose the disease, but also to determine the stage of the disease and monitor the dynamics of the disease:
- In the first 2 weeks of the disease, only immunoglobulins A are detected.
- From the 2nd to the 3rd week of the disease, immunoglobulins A and M are detected in the blood.
- From 3 to 4 weeks, a blood test for immunoglobulin determines all three types.
- During recovery, immunoglobulins M disappear from the blood, and the amount of A and G decreases by 2–4 times.
- In the presence of a chronic process, immunoglobulins G are necessarily present in the blood, immunoglobulins M are absent, immunoglobulins A may or may not be present.
Advantages of enzyme immunoassay (ELISA):
- Relatively high sensitivity (accuracy).
- Reasonable price.
- Allows for early diagnosis (due to the ability to determine immunoglobulin classes during analysis).
- Allows you to monitor the dynamics of the infectious process (thanks to the ability to determine immunoglobulin classes).
- Ease of use.
- An immunological blood test allows you to get a quick answer.
Disadvantages of ELISA blood test:
- Sometimes enzyme immunoassays give false positive or false negative results.
Scope of application of immunological blood test
- Diagnosis of viral diseases: hepatitis, herpes, Epstein-Barr virus, cytomegalovirus, etc.
- Sexually transmitted infections: chlamydia, gonorrhea, trichomonas, mycoplasma, ureaplasma.
- Syphilis.
- Endocrinology (determination of hormone levels).
- Tumor markers (diagnosis of cancer).
- Immunology (diagnosis of immunodeficiency).
- Allergology (diagnosis and treatment of allergies).
Serological blood test is a laboratory method of blood testing that is used to diagnose infectious diseases and determine the stage of the infectious process. The serological reaction is based on the interaction of antibodies and antigens.
Determination of antigens is used to determine the genus and species of microorganisms. This research method is used in urology and venereology. Blood for a serological blood test is taken in the morning on an empty stomach from a vein.
Definitive blood tests
These types of blood tests are very different from those listed above in that they do not diagnose any disease or health condition of a person, but simply indicate the peculiarity of his circulatory system. These include tests to determine blood type, Rh factor and coagulation. As a rule, these studies are mandatory for people in special professions, as well as for all pregnant women. Blood is taken for analysis from a vein and does not require special preparation of the patient.
Hormonal blood test
This type of study helps determine the general functioning of the organs of the human endocrine system, as well as identify diseases of the pituitary gland, thyroid gland, adrenal glands and other human endocrine organs. Blood is drawn on certain days depending on the production of the hormone that will be tested. This can be an analysis of thyroid hormones (T4, T3), pituitary gland (TSH, LH, FSH), sex glands (testosterone, estriol), adrenal glands (cortisol), as well as pregnancy hormone (hCG). The results will depend entirely on the age and gender of the person, as well as whether there are any diseases in his endocrine system.
Preparing for a hormone test
The amount of hormones in the blood depends on the time of day, since there is a daily rhythm of secretion (release of hormones). Blood for hormonal analysis should be taken in the morning, on an empty stomach.
In women, hormonal levels also depend on the stage of the menstrual cycle. The most favorable days for analysis are days 5-7 of the cycle, starting from the first day of menstruation.
On the eve of the test, you should not drink alcohol, and you should also avoid increased physical activity and stressful situations. It is advisable not to smoke for an hour before the test.
A week before the test, you must stop taking hormonal medications. If you are prescribed medication, discuss this with your doctor; the test may have to be postponed.
How to take a hormone test correctly?
The human hormonal system is connected to all organs and systems of the body. Therefore, the level of hormones in the blood may depend on various external influences and changes in the human body. General recommendations from doctors are as follows: you need to take a blood test for hormones in the morning on an empty stomach. Before donating blood for hormone testing, stop smoking, drinking alcohol and strenuous physical activity. Women need to have many hormones analyzed on certain days of the menstrual cycle. To ensure that the results of your hormone tests are as reliable as possible, consult your doctor and follow his recommendations.
When is a blood test for hormones prescribed?
Hormonal analysis is usually carried out if there is a suspicion of dysfunction of the endocrine glands or if an increase in the size of the glands is detected.
Indications for testing for female sex hormones (estrogens) are:
- menstrual irregularities;
- infertility;
- miscarriage;
- acne;
- overweight;
- fibrocystic mastopathy (breast disease).
Indications for testing for male sex hormones (androgens) are:
- suspicion of the development of tumor processes;
- ovarian dysfunction;
- kidney dysfunction;
- overweight (obesity);
- infertility;
- acne;
- in women – excessive growth of body hair.
Hormonal analysis is prescribed during pregnancy if pathological development of the fetus is suspected. An analysis for the hormone hCG (human chorionic gonadotropin), produced by the cells of the membrane of the embryo, can detect pregnancy already on the 6-10th day after fertilization.
Interpretation of blood test results for hormones
Blood from a vein is used to test hormones.
Depending on the clinical signs indicating a specific pathology, an analysis with tests for specific hormones is usually prescribed.
The most complete picture of your health can be obtained by taking a test for the following hormones.
Thyroid hormones:
- T3 (triiodothyronine) free – stimulates oxygen metabolism in tissues. Normal values: 2.6 - 5.7 pmol/l.
- T4 (thyroxine) – stimulates protein synthesis. Normal values: 0.7-1.48 ng/dl.
- Antibodies to thyroglobulin (AT-TG) are an important parameter for identifying a number of autoimmune diseases. Normal values: 0-4.11 U/ml.
- Some others.
Pituitary hormones:
- TSH (thyroid-stimulating hormone) – stimulates the production of thyroid hormones (T3 and T4). Normal values: 0.4-4.0 mU/l. An elevated TSH value usually indicates decreased thyroid function.
- FSH (follicle stimulating hormone) . Normal values: in women - depends on the phase of the menstrual cycle. Phase I – 3.35-21.63 mU/ml; Phase II – 1.11-13.99 mU/ml; postmenopause – 2.58-150.53 mU/ml; girls under 9 years old 0.2-4.2 mU/ml. In men – 1.37-13.58 mU/ml.
- LH (luteinizing hormone) . Normal values: in women - depends on the phase of the menstrual cycle. Phase I – 2.57-26.53 mU/ml; Phase II – 0.67-23.57 mU/ml; postmenopause - 11.3-40 mU/ml; girls under 9 years old - 0.03-3.9 mU/ml. In men – 1.26-10.05 mU/ml.
- Prolactin . The main function is to stimulate the development of mammary glands and lactation. Normal values: in women (from the first menstruation to menopause) - 1.2-29.93 ng/ml; in men - 2.58-18.12 ng/ml. Increased concentrations of prolactin are called hyperprolactinemia . There are physiological and pathological hyperprolactinemia. Physiological hyperprolactinemia can be caused by breastfeeding, pregnancy, severe physical activity, and stress. An increased concentration of prolactin in women leads to menstrual irregularities and may cause infertility. In men, hyperprolactinemia leads to decreased libido and impotence.
- ACTH (adrenocorticotropic hormone) – stimulates the synthesis and secretion of hormones from the adrenal cortex. Normal values: 9-52 pg/ml.
- Some others.
Sex hormones:
- Testosterone (male sex hormone) is produced by the adrenal glands and in the gonads (in men - in the testicles, in women - in the ovaries). Affects the development of the genital organs, the formation of secondary sexual characteristics, the growth of bones and muscles. Normal values: for men - 4.94-32.01 nmol/l, for women - 0.38-1.97 nmol/l.
- Estrogens (female sex hormones). The main estrogens - progesterone and estradiol - are produced by the adrenal glands and ovaries. Normal values of progesterone in women depend on the phase of the menstrual cycle: Phase I - 1.0-2.2 nM/l; Phase II - 23.0-30.0 nM/l; for postmenopause - 1.0-1.8 nM/l. Similarly for estradiol: phase I - 198-284 pM/l: phase II - 439-570 pM/l; for postmenopause - 51-133 pM/l. Elevated estrogen levels may indicate tumors of the ovaries and adrenal cortex, as well as cirrhosis of the liver. Reduced - for insufficient development and sclerosis of the ovaries.
Adrenal hormones:
- DEA-s (dehydroepiandrosterone sulfate) is necessary for the synthesis of testosterone and estrogens. The range of normal values for the concentration of this hormone: 3591 – 11907 nmol/l; in women - 810 - 8991 nmol/l. However, this is the general picture; when processing analysis data, the patient’s age must also be taken into account.
- Cortisol is involved in many metabolic processes and is actively produced as a result of the body’s response to hunger or stress. Normal values: for children under 16 years of age - 3-21 mcg/dl, for an adult - 3.7-19.4 mcg/dl.
- Aldosterone is responsible for regulating water-salt balance in the body. Normal values: 35 - 350 pg/ml.
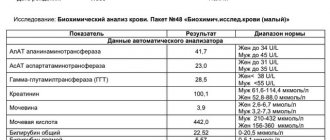
Blood chemistry
It is carried out to assess the functional state of the body, the functioning of its internal organs, as well as metabolism. This blood test can check your blood levels of protein, sugar, iron, cholesterol, bilirubin, triglycerides, various enzymes, calcium, magnesium, sodium, phosphorus and various gases. Any deviation from the norm may signal that some processes may be going on in the body that are invisible from the outside (parasitic infections, tumors, allergies). Patients with poor results of biochemical analysis may have diseases of the thyroid gland, liver, and possible diabetes mellitus and atherosclerosis. Depending on the type of biochemical analysis, preparation for blood sampling may vary, including following a diet for several days.
How to prepare for a biochemical blood test?
One day before taking blood for biochemistry, it is necessary to avoid drinking alcohol, and 1 hour before taking smoking. It is advisable to take blood samples on an empty stomach in the morning. There should be at least 12 hours between the last meal and the blood draw. Juice, tea, coffee, chewing gum are not allowed. You can drink water. It is necessary to exclude increased psycho-emotional and physical stress.
How are the results of a biochemical blood test evaluated?
The use of different diagnostic methods by different clinics leads to different results, and the units of measurement may also differ. Therefore, to correctly decipher the result of a biochemical blood test, a consultation with the attending physician is required.
What indicators are included in a standard biochemical blood test?
1) Glucose (in blood) is the main test in the diagnosis of diabetes mellitus. This analysis is very important when selecting therapy and assessing the effectiveness of diabetes treatment. A decrease in glucose levels is observed in some endocrine diseases and liver dysfunction.
Normal blood glucose levels:
| Age | Glucose level, mmol/l |
| < 14 years | 3,33 — 5,55 |
| 14 – 60 years | 3,89 — 5,83 |
| 60 - 70 years | 4,44 — 6,38 |
| > 70 years | 4,61 — 6,10 |
2) Common bilirubin is a yellow blood pigment that is formed as a result of the breakdown of hemoglobin, myoglobin and cytochromes. The main reasons for the increase in the amount of total bilirubin in the blood: damage to liver cells (hepatitis, cirrhosis), increased breakdown of red blood cells (hemolytic anemia), impaired outflow of bile (for example, cholelithiasis).
Normal values of total bilirubin: 3.4 - 17.1 µmol/l.
3) Direct bilirubin (conjugated, bound bilirubin) - a fraction of total blood bilirubin. Direct bilirubin increases with jaundice, which develops due to a violation of the outflow of bile from the liver.
Normal values of direct bilirubin: 0 - 7.9 µmol/l.
4) Indirect bilirubin (unconjugated, free bilirubin) - the difference between the indicators of total and direct bilirubin. This indicator increases with increased breakdown of red blood cells - with hemolytic anemia, malaria, massive hemorrhages in tissue, etc.
Normal values for indirect bilirubin: < 19 µmol/l.
5) AST (AST, aspartate aminotransferase) is one of the main enzymes synthesized in the liver. Normally, the content of this enzyme in the blood serum is low, since most of it is found in hepatocytes (liver cells). An increase is observed with liver and heart diseases, as well as with long-term use of aspirin and hormonal contraceptives.
Normal AST values:
- Women – up to 31 U/l;
- Men - up to 37 U/l.
6) ALT (ALT, alanine aminotransferase) is an enzyme synthesized in the liver. Most of it is located and works in liver cells, so normally the concentration of ALT in the blood is low. An increase is observed with massive death of liver cells (for example, with hepatitis, cirrhosis), severe heart failure and blood diseases.
Normal ALT values:
- women – up to 34 U/l;
- men – up to 45 U/l.
7) Gamma-GT (gamma-glutamyltransferase) is an enzyme found primarily in the cells of the liver and pancreas. An increase in its amount in the blood is observed with diseases of these organs, as well as with prolonged use of alcohol.
Normal gamma-GT values:
Men < 55 U/l
Women < 38 U/l
 Alkaline phosphatase is an enzyme widely distributed in human tissues. The hepatic and bone forms of alkaline phosphatase are of greatest clinical importance, the activity of which is determined in the blood serum.
Alkaline phosphatase is an enzyme widely distributed in human tissues. The hepatic and bone forms of alkaline phosphatase are of greatest clinical importance, the activity of which is determined in the blood serum.
Normal alkaline phosphatase values: 30-120 U/l.
9) Cholesterol (total cholesterol) is the main blood lipid that enters the body with food and is also synthesized by liver cells.
Normal cholesterol levels: 3.2-5.6 mmol/l.
10) Low-density lipoproteins (LDL) are one of the most atherogenic, “harmful” lipid fractions. LDL is very rich in cholesterol and, transporting it to vascular cells, lingers in them, forming atherosclerotic plaques.
Normal LDL levels: 1.71-3.5 mmol/l.
11) Triglycerides are neutral fats found in the blood plasma, an important indicator of lipid metabolism.
Normal triglyceride levels: 0.41-1.8 mmol/l.
12) Total protein - an indicator reflecting the total amount of proteins in the blood. Its decrease is observed in some diseases of the liver and kidneys, accompanied by increased excretion of protein in the urine. Increased in blood diseases and infectious and inflammatory processes.
Normal values for total protein: 66-83 g/l.
13) Albumin is the most important blood protein, making up approximately half of all serum proteins. A decrease in albumin content can also be a manifestation of certain diseases of the kidneys, liver, and intestines. Elevated albumin is usually associated with dehydration.
Normal albumin values: 35-52 g/l
14) Potassium (K+) is an electrolyte found primarily inside cells. An increase in the level of potassium in the blood is most often observed in acute and chronic renal failure, a sharp decrease in the amount of urine excreted or its complete absence, most often associated with severe kidney disease.
Normal potassium values: 3.5-5.5 mmol/l.
15) Sodium (Na+) is an electrolyte found primarily in extracellular fluid and in smaller quantities inside cells. It is responsible for the functioning of nervous and muscle tissue, digestive enzymes, blood pressure, and water metabolism.
Normal sodium values: 136-145 mmol/l.
16) Chlorine (Cl-) is one of the main electrolytes, which is in the blood in an ionized state and plays an important role in maintaining water-electrolyte and acid-base balances in the body.
Normal chlorine values: 98-107 mmol/l.
17) Creatinine is a substance that plays an important role in the energy metabolism of muscle and other tissues. Creatinine is completely excreted by the kidneys, so determining its concentration in the blood is of greatest clinical importance for diagnosing kidney diseases.
Normal creatinine values:
- men - 62 – 115 µmol/l;
- women - 53 - 97 µmol/l.
18) Urea is a substance that is the end product of protein metabolism in the body. Urea is excreted by the kidneys, so determining its concentration in the blood gives an idea of the functional abilities of the kidneys and is most widely used for diagnosing renal pathology.
Normal urea values: 2.8-7.2 mmol/l
19) Uric acid is one of the end products of protein metabolism in the body. Uric acid is completely excreted by the kidneys. An increase in the concentration of uric acid occurs in kidney stones and other kidney diseases that occur with renal failure.
Normal uric acid values:
- men - 210 - 420 µmol/l;
- women - 150 - 350 µmol/l.
20) C-reactive protein (CRP) is a sensitive element in the blood that reacts faster than others to tissue damage. The presence of reactive protein in blood serum is a sign of an inflammatory process, injury, or penetration of foreign microorganisms into the body - bacteria, parasites, fungi. The more acute the inflammatory process, the more active the disease, the higher the C-reactive protein in the blood serum.
Normal values for C-reactive protein: 0 - 5 mg/l.
21) Iron (serum iron) is a vital microelement that is part of hemoglobin, is involved in the transport and deposition of oxygen and plays an important role in hematopoiesis.
Normal serum iron values:
- women - 8.95 - 30.43 µmol/l;
- men - 11.64 - 30.43 µmol/l.