The ICP monitoring system allows you to conduct a primary screening study of intracranial pressure in newborns and children under 1 year of age in a non-invasive way and see ICP numbers on the screen of a bedside monitor. Includes ICP sensor, amplifier (signal decoder), cable for connection to a bedside monitor (custom made), 2 calibration kits, instructions and recommendations for clinical use. The system is calibrated at the interface between water and air and is intended for reusable use. The measurement error is 2-3 mmHg, due to the anatomy and principle of the study. Considering that the measurement is carried out without a high potential risk for a small patient (non-invasively), the results are interpreted as screening and allow one to assess the risks of developing complications of increased intracranial pressure. For example, if a child’s ICP figures are 20-25 mmHg. and higher, then the existing measurement error can be neglected, since the zero drift is 2-3 mmHg. Art. in such conditions it has no clinical significance; urgent measures are required to reduce intracranial pressure in the child. The measurement error of ICP monitors designed for invasive ICP measurement through the burr hole or subdural ranges from 1 to 2 mmHg. (depending on the brand of monitor).
Currently, this technique is successfully used in the Russian Federation and the CIS and is available for both public health facilities and private clinics. The system can be used both in a hospital and on an outpatient basis. The system is manufactured in the UK.
What is increased intracranial pressure?
Inside the brain there is a system of interconnected ventricles, which are also filled with cerebrospinal fluid (CSF). This protects the human brain from injuries, concussions, as much as possible. The pressure of cerebrospinal fluid on brain structures is called intracranial pressure. Exceeding the permissible norms entails a number of consequences.
The main question for parents is what are the signs of intracranial pressure in a child, and what threat does this pose to the child?
What complications can there be in children? If left untreated, increased intracranial pressure can lead to the following consequences: the occurrence of epileptic syndrome, blurred vision, mental disorders, strokes, disorders of consciousness, breathing problems, weakness in the limbs, etc.
What should parents of a child with this diagnosis know? ICP is not a disease, but only a symptom, a consequence of various diseases. There are several misconceptions among parents regarding increased intracranial pressure. For example, the fact that this is an incurable condition. However, with timely treatment, the child’s recovery is possible. The main thing that needs to be done is to consult a specialist in time and follow the doctor’s instructions.
Types of neonatal hypertension and causes of their occurrence
In pediatrics, there are 3 types of hypertension:
- Arterial.
- Pulmonary.
- Intracranial.
Depending on the type of pathological phenomenon, the clinical picture, complications, treatment methods and causes will vary.
- Symptomatic arterial hypertension
Arterial hypertension
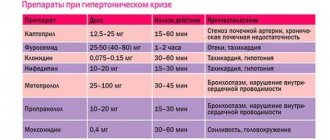
This is a secondary disease, which most often manifests itself against the background of other pathologies of the child. For a baby born at 38-42 weeks of gestation (full-term baby), the diagnosis of arterial hypertension is made when the systolic pressure level is more than 90 mmHg. Art., diastolic - more than 60. For premature babies, the level of indicators for diagnosis is reduced to 80 and 50 mm Hg. Art. respectively.
Possible causes of arterial hypertension in newborns:
- coarctation of the aorta;
- blockage or blood clots in the renal arteries;
- pyelonephritis;
- renal failure;
- kidney tumor or hyperplasia of renal tissue.
Kidney pathologies occupy a significant place in the development of hypertension and account for about 70% of all cases of the disease in children. Also, the pathological condition in question may occur against the background of an unsuccessful blood transfusion to the baby.
You can learn from this video what a disease such as arterial hypertension is, how it is characterized and why it can occur in children.
Pulmonary hypertension
This is a syndrome in which an infant experiences increased pressure in the pulmonary arteries. The syndrome manifests itself in 2 forms: primary and secondary.
Primary hypertension occurs in 0.3% of cases in both full-term and post-term infants. Causes of primary hypertension:
- pathologies that lead to hypoxia and asphyxia;
- diaphragmatic hernia;
- neonatal sepsis.
Secondary syndrome is the result of congenital diseases affecting the lung parenchyma. Possible causes of the disease:
- meconium aspiration syndrome;
- distress syndrome;
- pneumonia in a newborn.
Premature babies are less susceptible to this disease, which is due to the anatomical features of the development of smooth muscle tissue that surrounds the arterioles and appears by the 30th week of the gestational period.
- Purulent conjunctivitis in children: how to recognize and treat?
This video talks about the features of pulmonary hypertension in children: forms, symptoms, diagnosis, and other nuances.
Intracranial hypertension
Hypertension is characterized by increased intracranial pressure. This condition is a manifestation of another pathology that cannot occur independently.
Diseases that can cause the development of hypertension:
- intrauterine hypoxia;
- birth of a child at 22-30 weeks of pregnancy;
- tumor, the presence of other foreign tissues compressing the tissue of the cerebral hemispheres;
- injuries to the head and neck vessels that occurred during passage through the birth canal.
An increase in intracranial pressure occurs due to an increase in fluids, such as tissue, cerebrospinal fluid, and blood, which compress the brain tissue.
Symptoms of increased intracranial pressure
Increased intracranial pressure in children, symptoms of which can appear in the first minutes and hours after birth, often leads to the development of serious complications.
When parents may suspect something is wrong:
In young children:
- The baby constantly cries and does not calm down;
- Lack of thirst in the child, reluctance to drink;
- The baby is irritated by bright lights and sharp sounds;
- The child burps frequently and profusely;
- The baby's fontanel bulges;
- The baby's chin is shaking;
- Rapid head growth (this is due to stagnation of venous blood);
- The child throws his head back.
In older children
- Severe headaches;
- Nausea, vomiting;
- Increased fatigue, weakness;
- Drowsiness;
- Tearfulness, irritability;
- Apathy;
- Double vision.
Knowing the key signs of the disease, you can establish the correct diagnosis in the early stages and prescribe the correct treatment for your child. Even if you have only one of the listed symptoms, you need to immediately contact a neurologist! The sooner your baby receives help, the fewer consequences it will have for the child’s body in the future.
ABOUT INTRACRANIAL PRESSURE IN A CHILD. TREATMENT.
We often hear the phrase “My child has ICP .” And this is a true statement - all living creatures on the planet that have a skull also have intracranial pressure. But what then worries parents of children?
The correct way to talk about the problem is increased intracranial pressure. Let’s make a reservation right away - this is not a diagnosis, but a description of one of the links in the development of many different diseases (that is, a symptom ). Intracranial pressure (ICP) increases with hydrocephalus, brain tumors, neuroinfections (encephalitis, meningitis), traumatic brain injury, intracranial hemorrhage, some rare hereditary diseases, etc.
Attention! If a child really has increased intracranial pressure, then he really needs medical help, since the question is about developmental disorders of the child in the future, and in some cases - even a threat to life!
Indirect signs of increased ICP are:
- — sleep and behavior disorders;
- - hyperactivity, attention deficit;
- — disorders of mental, speech and motor development, low learning ability;
- - “marble” skin pattern (including on the head);
- - nosebleeds;
- - “finger impressions” on a skull x-ray;
- - tremor (shaking) of the chin;
- - walking on tiptoes
The cause of the condition lies in the excessive accumulation of cerebrospinal fluid in the ventricles of the brain, where this fluid is produced, and the difficulty of its movement or absorption in the subarachnoid space.
Sometimes doctors give such children syndromic diagnoses: “hydrocephalic syndrome” , “increased intracranial pressure” , “dilatation of the ventricles of the brain” (symmetric or asymmetric), “Graefe’s symptom”, “setting sun syndrome”, “hypertensive-hydrocephalic syndrome”.
Associated symptoms are:
- non-overgrowth of fontanelles;
- drowsiness;
- noticeable squint;
- white stripe of the eyeball between the pupil and the upper eyelid;
- frequent and profuse regurgitation;
- the occurrence of seizures;
- involuntary shuddering of the whole body;
- the baby’s innate reflexes are too weak;
- decreased muscle tone;
- excessive enlargement of the skull ;
- nausea; vomit;
- dizziness;
- poor sleep;
- excessive tearfulness;
- developmental delay.
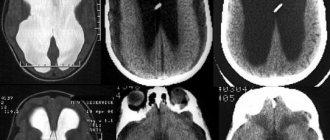
Reliable diagnostic methods for increased ICP are: ultrasound ( neurosonography ), CT and MRI of the brain.
TREATMENT OF HIGH ICP.
The choice of treatment methods depends on the severity of the disease.
Very severe forms ( hydrocephalus ) require surgical treatment with shunting to create an outflow of excess fluid. These are quite complex cases and osteopathic treatment can only be indicated after bypass surgery.
In less complex cases: traditionally, doctors prescribe diuretics, which remove fluid from everywhere, including the cerebrospinal fluid spaces. This is a nonspecific effect that is not aimed at the cause.
We set ourselves the task of normalizing the mechanisms of cerebrospinal fluid dynamics - the production and resorption of cerebrospinal fluid. This is work with the mobility of the bones of the base of the skull, which helps improve venous outflow, balance the tension of the dura mater, normalize the position and mobility of the cervical vertebrae, etc.
That is, we identify the root cause and act on it, restoring the normal physiology of the body.
Naturally, in the case of gross structural disorders, pharmacotherapy and, if necessary, surgical treatment are indicated. But if it is possible to restore normal mechanisms, this must be done.
It is important to understand that the solution to the problem does not need to be delayed or postponed, because the development of the syndrome can be prevented or reduced. It is necessary to consult a doctor - an osteopath already in the initial stages of the disease and almost always avoid serious consequences.
Diagnosis of intracranial pressure
Before prescribing treatment for your child, we perform a comprehensive neurological examination. It includes:
- Collecting anamnesis (conversation with the mother, studying the child’s medical record, history of pregnancy and childbirth and the results of previous studies);
- special neurological tests;
- active and muscle tests;
- reflex diagnostics;
- local palpation examination of the spine and musculoskeletal system.
In addition to the main examination, if necessary, the doctor may prescribe:
- NSG (neurosonography, ultrasound of the brain);
- MRI;
- Ultrasound;
- X-ray;
- Lab tests;
- EEG;
What does ICP mean?
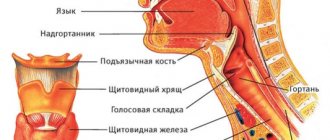
To understand how dangerous this is, you need to first study the anatomy of the baby’s head and figure out what processes occur in it.
The brain is located inside several membranes - arachnoid, soft and hard, surrounded on top by the bones of the skull. Inside the organ itself there are ventricles - cavities. There is cerebrospinal fluid present inside the ventricles and between the membranes.
Liquor is a clear, colorless liquid, very similar in appearance to water, containing a small amount of cells, protein and salts. In an infant, the amount of cerebrospinal fluid is about 50 ml. Liquor is constantly produced and absorbed; up to 500 ml of cerebrospinal fluid is produced per day by the choroid plexuses of the brain. This internal circulation of biological fluid ensures adequate nutrition of brain cells and also serves as protection from the effects of adverse factors.
Any disturbance in the system of liquor production, liquor circulation and absorption of liquor leads to its excessive accumulation in the cavities of the brain, which is called hydrocephalus, or dropsy of the brain.
The constant movement of cerebrospinal fluid inside the head occurs under the influence of intracranial pressure, so its level is not a constant value and can vary depending on various circumstances.
Treatment of intracranial pressure
To treat our little patients, we use only painless, gentle treatment methods that do not cause discomfort to the baby.
We use methods:
- Transcranial micropolarization (TCMP) is the effect of a low-power direct electric current (less than 1 mA) on brain tissue in order to activate individual brain centers (speech, motor, psychomotor, etc.);
- Manual therapy;
- Osteopathy - treatment by the hands of a doctor, a gentle effect on the musculoskeletal system, nervous and vascular systems, internal organs;
- Acupuncture - exposure to biologically active points with microneedles;
- Pharmacopuncture - the introduction of medicinal drugs of natural origin to the source of the problem;
- Isometric kinesiotherapy - individual gymnastic techniques/exercises, according to indications, with elements of joint massage;
- Isometric kinesiotherapy using the Exart installation;
- Ozone therapy - treatment with active oxygen;
- Physiotherapy;
- Physiotherapy with enzyme preparations;
- Medical massage;
- Therapeutic droppers;
- Hirudotherapy - treatment with leeches;
- Botulinum therapy - treatment with botulinum toxin;
- Tsubotherapy is a gentle effect on the reflex points of the body.
Remember that with increased intracranial pressure in children, treatment should be comprehensive, individual and under the supervision of a doctor.
Intracranial hypertension in children
January 30, 2017
Unfortunately, today intracranial hypertension in children (in other words, increased intracranial pressure) is not uncommon. Many parents have probably heard this term. Often, but not necessarily, intracranial pressure and cerebral palsy become companions.
Features and causes of occurrence Intracranial hypertension occurs due to an increase in the volume of cerebrospinal fluid (fluid of the ventricles of the brain), tissue fluid or blood. This phenomenon is also possible in cases of the appearance of a tumor and foreign tissue in the brain, and the pressure is not observed in any specific part of the brain, but covers it entirely.
Increased intracranial pressure can be caused by:
-congenital defects or anomalies, genetic predisposition; - hydrocephalus (water on the brain); - unfavorable course of pregnancy suffered during this period ———infectious diseases and/or difficult childbirth leading to birth injuries; -prematurity, intrauterine hypoxia or prolonged oxygen starvation during childbirth; - neuroinfections, inflammation of the membranes of the brain - meningitis, encephalitis.
The child cannot talk about his well-being, so the main task of parents is to carefully monitor the baby.
The symptoms are different:
profuse vomiting (several times a day), regurgitation in a fountain; superficial, restless sleep with frequent hysterical or monotonous crying for no reason; disproportionately large head size, rapid increase in skull size, inappropriate for age; swelling of the fontanelle and divergence of the sutures, failure to hear pulsations; irritability, lethargy, loss of appetite; muscle hypertonicity. convulsions, loss of consciousness, increased anxiety.
Intracranial hypertension itself is not a disease, but a symptom, so the goal of medical diagnosis is to identify the causes that led to the negative condition. Treatment begins immediately after the diagnosis is made.
Depending on the complexity of the symptoms, several methods and ways to eliminate them are used:
-the surgical route is used in the most severe cases, for example, with hydrocephalus - the essence of the surgical intervention is to install a shunt through which excess fluid is removed. It can be either temporary or lifelong and ensures rapid recovery for the patient. -drug treatment is practiced in cases of moderate severity. In this case, diuretics or combinations thereof are used, applied according to certain schemes. The results are monitored by neurosonography, so a significant improvement can occur within a week; - in mild forms of the disease, non-drug forms of treatment are prescribed, which may include the following procedures: a special drinking and eating regimen (diet); therapeutic swimming in the pool; a cycle of massage sessions and a complex of therapeutic exercises; physiotherapy and acupuncture; taking diuretic preparations and decoctions (at an older age and in the absence of an allergy to their components).
Thus, special attention should be paid to small children who can silently endure poor health for a long time, and if symptoms are detected, it is better not to delay a visit to a specialist. Any disease at an early stage is much easier to treat, and it is quite possible to prevent the consequences.
Back
Diseases caused by increased intracranial pressure
Our pediatric neurology department will help you not only make a correct diagnosis, but also undergo a course of treatment if your child has:
- Hyperactivity (attention deficit hyperactivity disorder, ADHD);
- Cerebral palsy (cerebral palsy);
- Autism;
- Delayed psychomotor development;
- Delayed speech development;
- Speech defects;
- Stuttering;
- Nervous tics;
- Enuresis;
- Sleep disturbances (sleeps poorly, sleeps little, wakes up frequently, does not fall asleep for a long time);
- Hypertonicity;
- Pyramid syndrome (pyramidal insufficiency syndrome);
- Hypertensive syndrome;
- Hydrocephalus (hydrocephalic syndrome, dropsy of the brain);
- Perinatal encephalopathy (perinatal damage to the central nervous system, PEP, PPCNS);
- Minimal brain dysfunction (MCD).
Causes of intracranial pressure:
- Birth or traumatic brain injury;
- Prematurity, pathologies during pregnancy or childbirth;
- Untimely fusion of the skull bones in a child;
- Benign brain tumors, which lead to increased blood pressure and changes in brain structures;
- Malignant brain tumors;
- Meningitis;
- Encephalitis;
- Toxic cerebral edema;
- Hydrocephalus;
- Genetic abnormalities and defects of the cerebrospinal fluid tract;
- Traumatic brain injury;
- Intracerebral hemorrhage.
In early childhood, signs of intracranial hypertension are:
- bulging of a large fontanel;
- Graefe's symptom (lag of the upper eyelid when the eyeball moves downwards);
- frequent regurgitation, mainly in a “fountain”;
- divergence of the sutures of the skull (in rare cases);
- an increase in head circumference that exceeds physiological norms by 2 or more times (in rare cases).
Additional signs may be: convergent strabismus, horizontal nystagmus.
Clinical diagnostic methods are:
- examination of the fundus by an ophthalmologist;
- neurosonography;
- echoencephalography (EEG);
- magnetic resonance imaging of the brain;
- transcranial Dopplerography of cerebral vessels;
- rheoencephalography (REG).
Treatment depends on the underlying cause that caused the increase in intracranial pressure, and can be either medicinal or surgical.