The article was checked by a cardiologist, member of the European Society of Cardiology, the Eurasian Association of Cardiologists, the Russian Society of Holter Monitoring O.A. Lozbineva. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
Edema is the medical term for the abnormal accumulation of fluid in certain tissues of the body. Parts of the body swell from injury or inflammation. Medicines, pregnancy and infections can also cause swelling. Fluid accumulation occurs when it is released from small blood vessels into nearby tissues.
Fluid accumulation may occur under the skin, usually in the lower extremities or lungs. The localization area can give the practitioner the first clues as to the main cause of the development of the pathological process in the body.
sign up for a consultation
Types of edema
Depends on origin:
- Lymphatic - those types of edema that are caused by causes and changes associated with the lymphatic system are considered as such. Among them are primary (there are congenital malformations of the lymphatic system, usually affecting the limbs), or secondary (there are acquired damage). The latter may be the result of operations to remove tumors in the lymphatic system, or in cases of burns, strokes or infections that cause vessel destruction.
- Dynamic - the lymphatic system does not show any changes, but excess fluid is felt. These include swelling of the veins caused by blood clots or problems with the blood vessels caused by strokes, inflammation, and medications. In women, the cause is varicose veins and exposure to hormones during pregnancy and the postpartum period.
The main factors are changes in the biochemical composition of tissue fluid and blood plasma. Disturbances also occur against the background of hormonal changes and increased capillary permeability.
The mechanism of pathology formation
Chronic cardiovascular failure develops slowly due to the body's compensatory mechanisms.
At the compensatory stage of the myocardium, the heart muscle begins to hypertrophy. The vessels expand, causing their walls to become more fragile and permeable over time. Hormones are produced that change the composition of the blood, which becomes more liquid, its volume increases due to increased work of the bone marrow and an increase in the amount of water due to retention.
Compensatory possibilities dry up, and the decompensatory stage begins, which is characterized by a weakening of the functions of the entire cardiovascular system.
As the muscle mass of the myocardium grows, its small vessels lag behind in development, as a result, the heart muscle lacks oxygen and nutrients. Pathological changes occur: the proliferation of connective and sclerotic tissue. The heart becomes unable to pump the increasing volume of blood. Extensive oxygen starvation begins, which covers all organs.
Along with this, the walls of blood vessels become more fragile and permeable. Lymph leaks from the vessels. Swelling begins. These phenomena are especially dangerous in the lungs. They quickly fill with liquid and stretch. A person is tormented by a severe cough, and the discharge of sputum does not provide relief.
Reasons for development
The veins in the legs have valves that act as "check valves" to prevent blood from flowing into the legs due to gravity. The heartbeat pushes blood through the arteries down to the legs. The blood must return to the heart to be recirculated through the veins. Blood pressure through the system and contracting leg muscles push blood up the veins, while valves prevent backflow down against gravity.
Valve insufficiency allows blood to pool in the legs and feet, eventually leading to swelling. When blood stagnates or pools in an area, fluid leaks into the surrounding tissue.
Valve insufficiency can occur for the following reasons:
- with age;
- from standing for long periods of time;
- from sitting for many hours;
- from varicose veins.
Regardless of the cause, as the valves in the legs become dysfunctional, blood pools and causes swelling, which puts pressure on the veins, causing them to widen and widen. This prevents the valves from working effectively, leading to even more swelling.
Main reasons for development:
- kidney diseases: glomerulonephritis, nephrotic syndrome, renal failure;
- heart diseases: heart failure;
- vein lesions (varicose veins, inflammation, thrombosis);
- liver diseases: cirrhosis of the liver, blockage of the hepatic veins;
- diseases of the endocrine system: hypothyroidism, diabetes;
- severe cancer;
- nutritional dystrophy;
- pregnancy;
- allergic reactions: insect bites, contact with an allergen.
Depending on the type, swelling can lead to retinal detachment, stroke, seizures, and even death. It is unacceptable to ignore the problem. To determine the cause, sign up for a consultation with specialists at the Yauza Hospital.
Acute form
Along with chronic, there is an acute form of heart failure. The reasons for its occurrence are:
- myocardial infarction;
- major stroke;
- structural defects of the heart, congenital and acquired;
- hypertension.
A distinctive feature of acute cardiovascular failure is the suddenness of the attack and the absence of the listed stages of development. The person's condition quickly deteriorates and death is possible within a few minutes. The occurrence of pathology is indicated by a sharp deterioration in condition, suffocation, severe cough with foam or red sputum, blue discoloration of the skin, and cold sweat.
In such cases, first aid is to call an ambulance. Then the victim should be taken out into the open air, the collar and other tight clothing should be unbuttoned. The best pose is considered to be sitting, with legs down. A nitroglycerin tablet should be given under the tongue. Repeat the dose every 10 minutes until the ambulance arrives.
Important! In acute heart failure, you should not take a supine position.
Edema as symptoms of diseases
In addition to vein problems, swelling can be caused by many other problems. In this case, clinical manifestations are usually observed on both legs.
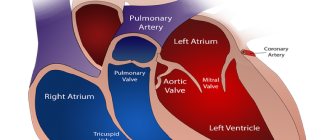
Heart pathologies
When the heart begins to fail as a pump, fluid pools in areas such as the legs and lungs and causes swelling. In addition, less blood flows to the kidneys, causing fluid retention.
Lung diseases
The cause is acute pulmonary failure, which is associated with the release of transudate from the capillaries. This is fraught with infiltration of the alveoli and a sharp disruption of gas exchange in the lungs.
It manifests itself as shortness of breath at rest, suffocation, a feeling of tightness in the chest, cough with the release of foamy bloody sputum. Accompanied by the development of acidosis and hypoxia.
Kidney diseases
Excess fluid and sodium in the circulation can cause fluid to accumulate. Swelling associated with kidney disease usually occurs in the legs and around the eyes.
Damage to the tiny filtering blood vessels in the kidneys can lead to nephrotic syndrome. In nephrotic syndrome, decreased levels of protein (albumin) in the blood can lead to fluid accumulation.
Severe liver pathologies
With cirrhosis, as a rule, fluid accumulates in the abdominal cavity. Accompanied by liver failure, dilation of hemorrhoidal veins and bleeding from the esophagus.
Quincke's edema
An acute disease that is characterized by the appearance of limited angioedema of the skin and subcutaneous tissue, body systems and various organs. The reasons are autoimmune and infectious diseases, false and true allergies. It occurs acutely and goes away within 2-3 days.
Arthritis
During the inflammatory process in the joint area, a large amount of synovial fluid is released. It accumulates in the cavity of the articular structure. When inflammation spreads to adjacent soft tissues, extensive (spread) edema develops.
We treat all types of edema
Specialists at the Yauza Clinical Hospital diagnose and treat edema of various origins. We follow international protocols and use modern equipment.
For cardiovascular diseases
“Cardiac” edema develops slowly – over several weeks or months. They are characterized by symmetry and increase in size in the evening. They first appear on the lower extremities or lower abdomen, in severe cases they spread throughout the body and are accompanied by the accumulation of fluid in the abdominal cavity (ascites) and enlarged liver. In this case, the skin most often feels cold to the touch and the swelling is dense. When pressed, a hole remains.
Patients complain of shortness of breath, which worsens when lying down, and low exercise tolerance. They have wheezing in the lungs, tachycardia, pallor of the lips, and cyanosis of the nasolabial triangle. As circulatory failure is compensated, swelling decreases or disappears.
Swelling due to venous insufficiency also becomes more pronounced in the evening, causing the sensation of shoes suddenly becoming tight (due to swelling of the feet), and the legs become visually thicker, often not symmetrically. Swelling in the legs is accompanied by a feeling of heaviness, fatigue, and pain in the legs. Spider veins and an enhanced pattern of veins are noticeable on the skin. In severe cases, swelling persists constantly, cramps in the calves are possible, trophic changes develop - thinning of the skin, persistent redness, peeling, itching, and poorly healing ulcers. Timely professional medical care helps prevent or reduce the risk of such progression of the disease.
For kidney diseases
“Renal” edema can develop very quickly - in less than a day. Swelling appears mainly on the face. Swelling under the eyes is noticeable in the morning. They can also be localized on the limbs and abdominal wall. When changing postures, bodies quickly shift. Fluid accumulation often occurs - ascites or hydrothorax. Edema skin is soft or dense, pale, dry.
Swelling due to kidney disease may be accompanied by a decrease in the amount of urine excreted, a change in its color, and possibly the appearance of blood (red blood cells) and protein in a urine test. Pain appears in the lumbar region. Nonspecific manifestations include headache and weakness. Shortness of breath and liver enlargement, characteristic of circulatory failure, are not observed. Renal edema can be a consequence of an infectious disease (tonsillitis, viral infection, etc.) and requires observation and treatment by a specialist (nephrologist, rheumatologist, therapist).
Allergic
Allergic edema develops quickly (in a few minutes) and is regional in nature. They arise as a result of contact with an allergen or an insect bite. They develop most often on the face (eyes, eyelids, mucous membranes, lips), arms (fingers, hands), elbows and knees.
The development of allergic edema is accompanied by itching and rash. In severe cases, due to bronchospasm, attacks of difficulty breathing are possible, usually in the exhalation phase. Swelling of the larynx can lead to suffocation and pose a threat to the patient's life. Therefore, patients prone to such a reaction should be prepared for a dangerous situation.
It is necessary to discuss in advance with the doctor what medications will help the patient safely wait for the ambulance to arrive (delivery to the hospital) in case of an acute allergy attack and always have them available.
Prolonged swelling causes stretching of the skin, makes blood vessels less elastic, and impairs blood circulation. Swelling negatively affects the joints and causes difficulty moving. Ulcers may develop at the site of swelling, which are subsequently difficult to treat. Don't take things to the extreme. Make an appointment with a doctor and get rid of the problem.
Diagnostic stages
Consultation and examination by a therapist. After a detailed conversation and medical examination, the patient can be referred for consultation to other specialists depending on the etiology of the disease: cardiologist, allergist, endocrinologist, nephrologist, urologist, etc.
Laboratory research. First of all, the following are carried out:
- general (with leukocyte formula) and biochemical blood tests;
- general urine analysis.
- Instrumental studies:
- ECG;
- echocardiography;
- Ultrasound of blood vessels of the lower extremities;
- X-ray of the chest organs.
Next, the doctor prescribes a set of studies on an individual basis in each individual case.
To effectively eliminate swelling, you need to know exactly what disease is causing it. Edema is not an independent disease, but a symptom. Diagnostics using modern equipment will allow us to determine the cause of the pathology. The information obtained allows the doctor to choose the most effective treatment. Don't put off taking care of your health until later. Schedule a consultation with your doctor today to stay energized for years to come.
sign up for a consultation
Treatment of swelling
Treatment of edema is carried out in accordance with the cause of its development. Here are some general recommendations:
- Limit fluid intake to 1.5 liters per day, and sometimes less.
- Reduce salt intake to 1–1.5 g per day.
- Diuretics should be taken only under the supervision of a doctor who monitors the patient’s condition and monitors the level of electrolytes in the blood. Diuretics can lead to a decrease in potassium levels in the body, so it is recommended to eat dried apricots, raisins, rice, baked potatoes and other foods rich in this trace element.
- For cardiovascular diseases, a cardiologist, after diagnosing “cardiac” edema, selects therapy to maintain a stable state of the vascular system. A patient with heart failure should visit a cardiologist regularly throughout his life. In case of venous insufficiency, conservative or surgical treatment is carried out by a vascular surgeon-phlebologist.
- If the swelling is caused by kidney disease, in addition to relieving the swelling, the doctor (therapist or nephrologist) prescribes therapy for the underlying disease, which may include antibiotics, anti-inflammatory hormonal drugs, etc.
- In case of allergic edema, which is accompanied by difficulty breathing, urgent medical attention is required. Before help is provided, you should take an antihistamine, if the condition is severe - prednisolone or dexamethasone. In case of an attack of suffocation of an allergic nature, take 1-2 breaths from an inhaler recommended by your doctor (allergist).
Publications in the media
Chronic systolic heart failure is a clinical syndrome that complicates the course of a number of diseases and is characterized by the presence of shortness of breath during exercise (and then at rest), fatigue, peripheral edema and objective signs of impaired cardiac function at rest (for example, auscultatory signs, echocardiographic data) . Statistical data. Chronic systolic heart failure occurs in 0.4–2% of the population. Its prevalence increases with age: in people over 75 years of age it develops in 10% of cases.
Etiology • Heart failure with low cardiac output •• Myocardial damage: ••• IHD (post-infarction cardiosclerosis, chronic myocardial ischemia) ••• Cardiomyopathies ••• Myocarditis ••• Toxic effects (for example, alcohol, doxorubicin) ••• Infiltrative diseases (sarcoidosis, amyloidosis) ••• Endocrine diseases ••• Nutritional disorders (vitamin B1 deficiency) •• Myocardial overload ••• Arterial hypertension ••• Rheumatic heart defects ••• Congenital heart defects (for example, aortic stenosis) •• Arrhythmias ••• Supraventricular and ventricular tachycardias ••• Atrial fibrillation • Heart failure with high cardiac output •• Anemia •• Sepsis •• Arteriovenous fistula.
Risk factors • Refusal of the patient from pharmacotherapy • Prescription of drugs with a negative inotropic effect, and their uncontrolled use • Thyrotoxicosis, pregnancy and other conditions associated with increased metabolic needs • Excess body weight • Presence of chronic pathology of the heart and blood vessels (arterial hypertension, coronary artery disease, defects hearts, etc.).
Pathogenesis • The pumping function of the heart is impaired, which leads to a decrease in cardiac output • As a result of a decrease in cardiac output, hypoperfusion of many organs and tissues occurs •• A decrease in cardiac perfusion leads to activation of the sympathetic nervous system and an increase in heart rate •• A decrease in renal perfusion causes stimulation of the renin-angiotensin systems. The production of renin increases, while excessive production of angiotensin II occurs, leading to vasoconstriction, water retention (edema, thirst, increased blood volume) and a subsequent increase in preload on the heart •• A decrease in the perfusion of peripheral muscles causes the accumulation of under-oxidized metabolic products in them, as well as hypoxia leads to severe fatigue.
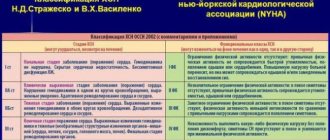
CLASSIFICATIONS Classification of the XII All-Union Congress of Therapists in 1935 ( N.D. Strazhesko, V.Kh. Vasilenko). • Stage I (initial) - latent heart failure, manifested only during physical activity (shortness of breath, tachycardia, fatigue). • Stage II (severe) - prolonged circulatory failure, hemodynamic disturbances (stagnation in the systemic and pulmonary circulation), dysfunction of organs and metabolism are also expressed at rest •• Period A - the beginning of a long stage, characterized by mild hemodynamic disturbances, dysfunction hearts or only parts of them •• Period B - the end of a long stage, characterized by profound hemodynamic disturbances, the entire cardiovascular system is involved in the process. • Stage III (final, dystrophic) - severe hemodynamic disorders, persistent changes in metabolism and functions of all organs, irreversible changes in the structure of tissues and organs.
New York Heart Association classification (1964) • Class I - ordinary physical activity does not cause significant fatigue, shortness of breath or palpitations • Class II - mild limitation of physical activity: satisfactory health at rest, but ordinary physical activity causes fatigue, palpitations, shortness of breath or pain • Class III - severe limitation of physical activity: satisfactory health at rest, but less than usual load leads to the appearance of symptoms • Class IV - inability to perform any physical activity without deteriorating well-being: symptoms of heart failure are present even at rest and intensify with any physical activity .
The classification of the Society of Heart Failure Specialists (OSSN, 2002) was adopted at the All-Russian Congress of Cardiologists in October 2002. The convenience of this classification is that it not only reflects the state of the process, but also its dynamics. The diagnosis must reflect both the stage of chronic heart failure and its functional class. It is necessary to take into account that the correspondence between the stage and the functional class is not entirely clear - the functional class is set in the presence of slightly less pronounced manifestations than is necessary to assign the corresponding stage of heart failure.
• Stages of chronic heart failure (may worsen despite treatment) •• Stage I - the initial stage of heart disease (damage). Hemodynamics are not impaired. Latent heart failure Asymptomatic left ventricular dysfunction •• Stage IIA - clinically pronounced stage of heart disease (damage). Hemodynamic disturbances in one of the blood circulation circles, expressed moderately. Adaptive remodeling of the heart and blood vessels •• Stage IIB - severe stage of heart disease (damage). Pronounced changes in hemodynamics in both circles of blood circulation. Maladaptive remodeling of the heart and blood vessels •• Stage III - the final stage of cardiac damage. Pronounced changes in hemodynamics and severe (irreversible) structural changes in target organs (heart, lungs, blood vessels, brain, kidneys). The final stage of organ remodeling.
• Functional classes of chronic heart failure (can change during treatment in either direction) •• FC I - there are no restrictions on physical activity: habitual physical activity is not accompanied by rapid fatigue, shortness of breath or palpitations. The patient can tolerate increased workload, but it may be accompanied by shortness of breath and/or delayed recovery •• FC II - slight limitation of physical activity: there are no symptoms at rest, habitual physical activity is accompanied by fatigue, shortness of breath or palpitations •• FC III - noticeable limitation of physical activity: at rest there are no symptoms, physical activity of lesser intensity compared to usual exercise is accompanied by the appearance of symptoms •• FC IV - inability to perform any physical activity without discomfort; Symptoms of heart failure are present at rest and worsen with minimal physical activity.
Clinical manifestations • Complaints - shortness of breath, attacks of suffocation, weakness, fatigue • • Shortness of breath in the initial stage of heart failure occurs during physical activity, and in case of severe heart failure - at rest. It appears as a result of increased pressure in the pulmonary capillaries and veins. This reduces the extensibility of the lungs and increases the work of the respiratory muscles. •• Severe heart failure is characterized by orthopnea - a forced sitting position taken by the patient to facilitate breathing with severe shortness of breath. The deterioration of health in the supine position is due to the deposition of fluid in the pulmonary capillaries, leading to an increase in hydrostatic pressure. In addition, in the lying position, the diaphragm rises, which makes breathing somewhat difficult. • Chronic heart failure is characterized by paroxysmal nocturnal shortness of breath (cardiac asthma), caused by the occurrence of interstitial pulmonary edema. At night, during sleep, an attack of severe shortness of breath develops, accompanied by coughing and the appearance of wheezing in the lungs. As heart failure progresses, alveolar pulmonary edema may occur •• Rapid fatigue in patients with heart failure appears due to insufficient oxygen supply to skeletal muscles •• Patients with chronic heart failure may experience nausea, loss of appetite, abdominal pain, abdominal enlargement (ascites) due to blood stagnation in the liver and portal vein system •• From the side of the heart, pathological III and IV heart sounds can be heard. Moist rales are detected in the lungs. Hydrothorax is characteristic, often right-sided, resulting from an increase in pleural capillary pressure and extravasation of fluid into the pleural cavity.
• Clinical manifestations of heart failure significantly depend on its stage •• Stage I - signs (fatigue, shortness of breath and palpitations) appear during normal physical activity, there are no manifestations of heart failure at rest •• Stage IIA - there are unexpressed hemodynamic disturbances. Clinical manifestations depend on which parts of the heart are predominantly affected (right or left) ••• Left ventricular failure is characterized by stagnation in the pulmonary circulation, manifested by typical inspiratory shortness of breath with moderate physical exertion, attacks of paroxysmal nocturnal shortness of breath, and rapid fatigue. Swelling and enlargement of the liver are uncharacteristic. ••• Right ventricular failure is characterized by the formation of congestion in the systemic circulation. Patients are concerned about pain and heaviness in the right hypochondrium, decreased diuresis. The liver is characterized by enlargement (the surface is smooth, the edge is rounded, palpation is painful). A distinctive feature of stage IIA heart failure is considered to be complete compensation of the condition during treatment, i.e. reversibility of manifestations of heart failure as a result of adequate treatment •• Stage IIB - there are profound hemodynamic disturbances, the entire circulatory system is involved in the process. Shortness of breath occurs with the slightest physical exertion. Patients are concerned about a feeling of heaviness in the right hypochondrium, general weakness, and sleep disturbances. Orthopnea, edema, ascites are characteristic (a consequence of increased pressure in the hepatic veins and peritoneal veins - transudation occurs, and fluid accumulates in the abdominal cavity), hydrothorax, hydropericardium •• Stage III - the final dystrophic stage with profound irreversible metabolic disorders. As a rule, the condition of patients at this stage is severe. Shortness of breath is pronounced even at rest. Characterized by massive edema, accumulation of fluid in the cavities (ascites, hydrothorax, hydropericardium, edema of the genital organs). At this stage, cachexia occurs.
Instrumental data • ECG : you can identify signs of blockade of the left or right branch of the His bundle, ventricular or atrial hypertrophy, pathological Q waves (as a sign of a previous MI), arrhythmias. A normal ECG casts doubt on the diagnosis of chronic heart failure. • EchoCG allows you to clarify the etiology of chronic heart failure and assess the functions of the heart, the degree of their impairment (in particular, determine the ejection fraction of the left ventricle). Typical manifestations of heart failure are expansion of the cavity of the left ventricle (as it progresses, expansion of other chambers of the heart), an increase in the end-systolic and end-diastolic dimensions of the left ventricle, and a decrease in its ejection fraction. • X-ray examination •• It is possible to detect venous hypertension in the form of redistribution of blood flow in favor of the upper parts of the lungs and an increase in the diameter of blood vessels •• With congestion in the lungs, signs of interstitial edema are detected (Kerley lines in the costophrenic sinuses) or signs of pulmonary edema •• Hydrothorax is detected ( most often right-sided) •• Cardiomegaly is diagnosed when the transverse size of the heart increases by more than 15.5 cm in men and more than 14.5 cm in women (or when the cardiothoracic index is more than 50%). • Catheterization of the cardiac cavities reveals an increase in pulmonary capillary wedge pressure of more than 18 mm Hg. Diagnostic criteria - Framingham criteria for the diagnosis of chronic heart failure, divided into major and minor • Major criteria: paroxysmal nocturnal dyspnea (cardiac asthma) or orthopnea, distention of the jugular veins, wheezing in the lungs, cardiomegaly, pulmonary edema, pathological III heart sound, increased central venous pressure ( more than 160 mm water column), blood flow time more than 25 s, positive “hepatojugular reflux” • Minor criteria: swelling in the legs, night cough, shortness of breath on exertion, liver enlargement, hydrothorax, tachycardia more than 120 per minute, decrease in vital capacity by 1 /3 of the maximum • To confirm the diagnosis of chronic heart failure, either 1 major or 2 minor criteria are required. The symptoms detected must be related to heart disease.
Differential diagnosis • Nephrotic syndrome - a history of edema, proteinuria, renal pathology • Liver cirrhosis • Occlusive lesions of the veins with subsequent development of peripheral edema. Treatment • It is necessary to first evaluate the possibility of influencing the cause of the deficiency. In some cases, effective etiological intervention (for example, surgical correction of heart disease, myocardial revascularization in ischemic heart disease) can significantly reduce the severity of manifestations of chronic heart failure • In the treatment of chronic heart failure, non-drug and drug therapy methods are distinguished. It should be noted that both types of treatment should complement each other.
Non-drug treatment • Limiting the consumption of table salt to 5–6 g/day, liquid (up to 1–1.5 l/day) • Optimizing physical activity •• Moderate physical activity is possible and even necessary (walking for at least 20–30 minutes 3 –5 r/week) •• Complete physical rest should be observed if the condition worsens (at rest the heart rate decreases and the work of the heart decreases).
Drug therapy . The ultimate goal of treatment of chronic heart failure is to improve the quality of life and increase its duration.
• Diuretics. When prescribing them, it is necessary to take into account that the occurrence of edema in heart failure is associated with several reasons (constriction of the renal vessels, increased secretion of aldosterone, increased venous pressure. Treatment with diuretics alone is considered insufficient. In chronic heart failure, loop (furosemide) or thiazide (for example, hydrochlorothiazide) diuretics. If the diuretic response is insufficient, loop diuretics and thiazides are combined •• Thiazide diuretics. Hydrochlorothiazide is usually used in a dose of 25 to 100 mg/day. It should be remembered that if the renal GFR is less than 30 ml/min, it is not advisable to use thiazides •• Loop diuretics begin to act faster, their diuretic effect is more pronounced, but less durable than that of thiazide diuretics. Furosemide is used at a dose of 20–200 mg/day IV, depending on the manifestations of edema and diuresis. It can be prescribed orally at a dose of 40– 100 mg/day.
• ACE inhibitors cause hemodynamic unloading of the myocardium due to vasodilation, increased diuresis, and decreased filling pressure of the left and right ventricles. Indications for prescribing ACE inhibitors are clinical signs of heart failure, a decrease in left ventricular ejection fraction of less than 40%. When prescribing ACE inhibitors, certain conditions must be observed according to the recommendations of the European Society of Cardiology (2001) •• It is necessary to stop taking diuretics 24 hours before taking ACE inhibitors •• Blood pressure should be monitored before and after taking ACE inhibitors •• Treatment begins with small doses with gradual their increase •• It is necessary to monitor renal function (diuresis, relative density of urine) and the concentration of blood electrolytes (potassium, sodium ions) while increasing the dose every 3–5 days, then every 3 and 6 months •• Avoid co-administration of potassium-sparing diuretics (their can be prescribed only for hypokalemia) •• Concomitant use of NSAIDs should be avoided.
• The first positive data have been obtained on the beneficial effect of angiotensin II receptor blockers (in particular, losartan) on the course of chronic heart failure as an alternative to ACE inhibitors in cases of intolerance or contraindications to their use.
• Cardiac glycosides have a positive inotropic (increase and shorten systole), negative chronotropic (decreasing heart rate), negative dromotropic (slowing AV conduction) effect. The optimal maintenance dose of digoxin is considered to be 0.25–0.375 mg/day (in elderly patients 0.125–0.25 mg/day); The therapeutic concentration of digoxin in blood serum is 0.5–1.5 mg/l. Indications for the use of cardiac glycosides are tachysystolic atrial fibrillation and sinus tachycardia.
• b-blockers •• The mechanism of beneficial action of β-blockers in chronic heart failure is due to the following factors ••• Direct protection of the myocardium from the adverse effects of catecholamines ••• Protection against catecholamine-induced hypokalemia ••• Improvement of blood flow in the coronary arteries due to a decrease in heart rate and improvement diastolic relaxation of the myocardium ••• Reducing the effect of vasoconstrictor systems (for example, due to decreased renin secretion) ••• Potentiation of the vasodilating kallikrein-kinin system ••• Increasing the contribution of the left atrium to the filling of the left ventricle due to improved relaxation of the latter •• Currently from b -adrenergic blockers for the treatment of chronic heart failure, carvedilol is recommended for use - a b1- and a1-blocker with vasodilating properties. The initial dose of carvedilol is 3.125 mg 2 times / day, followed by an increase in the dose to 6.25 mg, 12.5 mg or 25 mg 2 times / day in the absence of side effects in the form of arterial hypotension, bradycardia, decreased left ventricular ejection fraction (according to EchoCG) and other negative manifestations of the action of b-blockers. Metoprolol is also recommended, starting with a dose of 12.5 mg 2 times / day, bisoprolol 1.25 mg 1 time / day under the control of ventricular ejection fractions with a gradual increase in dose after 1-2 weeks.
• Spironolactone. It has been established that the administration of the aldosterone antagonist spironolactone at a dose of 25 mg 1–2 times a day (in the absence of contraindications) helps to increase the life expectancy of patients with heart failure. • Peripheral vasodilators are prescribed for chronic heart failure if there are contraindications or if ACE inhibitors are poorly tolerated. Of the peripheral vasodilators, hydralazine is used at a dose of up to 300 mg/day, isosorbide dinitrate at a dose of up to 160 mg/day.
• Other cardiotonic drugs . β-Adrenergic agonists (dobutamine), phosphodiesterase inhibitors are usually prescribed for 1–2 weeks in the final stage of heart failure or in case of a sharp deterioration in the patient’s condition.
• Anticoagulants. Patients with chronic heart failure are at high risk of thromboembolic complications. Both pulmonary embolism due to venous thrombosis and thromboembolism of vessels in the systemic circulation caused by intracardiac thrombi or atrial fibrillation are possible. The administration of indirect anticoagulants to patients with chronic heart failure is recommended in the presence of atrial fibrillation and a history of thrombosis.
• Antiarrhythmic drugs. If there are indications for the prescription of antiarrhythmic drugs (atrial fibrillation, ventricular tachycardia), it is recommended to use amiodarone at a dose of 100–200 mg/day. This drug has minimal negative inotropic effects, whereas most other drugs in this class reduce left ventricular ejection fraction. In addition, antiarrhythmic drugs themselves can provoke arrhythmias (proarrhythmic effect). Surgery
• The choice of the optimal method of surgical treatment depends on the cause leading to heart failure. Thus, in case of ischemic heart disease, in many cases, myocardial revascularization is feasible; in case of idiopathic subaortic hypertrophic stenosis, septal myectomy; in case of valvular defects, prosthetics or reconstructive interventions on the valves; in case of bradyarrhythmias, pacemaker implantation, etc.
• In case of heart failure refractory to adequate therapy, the main surgical treatment is heart transplantation. • Methods of mechanical circulatory support (implantation of assisters, artificial ventricles and biomechanical pumps), previously proposed as temporary options before transplantation, have now acquired the status of independent interventions, the results of which are comparable to the results of transplantation. • To prevent the progression of cardiac dilatation, devices are implanted in the form of a mesh that prevents excessive expansion of the heart. • In case of cor pulmonale that is tolerant to treatment, transplantation of the heart-lung complex seems to be a more appropriate intervention.
Forecast. Overall, the 3-year survival rate of patients with chronic systolic heart failure is 50%. The mortality rate from chronic systolic heart failure is 19% per year.
• Factors, the presence of which correlates with a poor prognosis in patients with heart failure •• Decrease in left ventricular ejection fraction of less than 25% •• Inability to climb one floor and move at a normal pace for more than 3 minutes •• Decrease in the content of sodium ions in blood plasma less than 133 mEq /l •• Decrease in the concentration of potassium ions in the blood plasma less than 3 meq/l •• Increase in the content of norepinephrine in the blood •• Frequent ventricular extrasystole during daily ECG monitoring.
• The risk of sudden cardiac death in patients with heart failure is 5 times higher than in the general population. Most patients with chronic heart failure die suddenly, mainly from ventricular fibrillation. Prophylactic administration of antiarrhythmic drugs does not prevent this complication.
ICD-10 • I50 Heart failure
Why us
Advantages of visiting our medical center:
- Doctors. We welcome specialists of the highest qualification category, holders of academic degrees, with extensive experience in leading Russian clinics.
- Individual approach. The doctor will develop an individual treatment plan for each patient in accordance with the cause of development and clinical picture of the disease.
- Complexity. Effective treatment of edema and the diseases that cause them is possible thanks to the close cooperation of our clinic’s specialists - therapist, cardiologist, allergist, endocrinologist, urologist, etc.
- Expert equipment. All studies are carried out using modern equipment and are highly accurate.
- Comfort. All consultations, studies and treatment are carried out within our hospital, which allows our patients to save money.
You can see prices for services in the price list or check by calling the phone number listed on the website.
Age and gender factor
Statistical studies prove the connection between the spread of the disease and the gender and age of the patient.
In the age group up to 65 years, women suffer from congestive heart failure to a lesser extent; above this age, the rates become equal. Death as a result of acute heart failure is recorded in men after 45 years.
In old age, symptoms of congestive heart failure are more common, this is explained by chronic diseases, poor lifestyle, and reduced immunity.