The liver is the “laboratory” of the human body.
Complex reactions of splitting and neutralizing compounds coming from inside and outside take place in this gland. Constant toxic or infectious exposure leads to a malfunction of the organ and the gradual destruction of its structure. Healthy tissue is gradually displaced and the gland ceases to function normally. Liver cirrhosis is a chronic disease in which hepatocytes die and the affected areas of parenchyma are replaced by connective tissue. The surface becomes scarred and wrinkled. The changes are irreversible, especially in the last phase.
Treatment of liver cirrhosis in the early stages can stop the damage and prolong a person’s life for decades. At the same time, the liver remains active, which allows you to live a full life. Delaying contact with a doctor is fraught with serious irreversible consequences. How does pathology develop? Let's take a closer look.
Content:
- How does alcoholic cirrhosis of the liver develop?
- Classification
- Symptoms of the disease
- Diagnostic features
- How to treat alcoholic cirrhosis of the liver
- How long do people live with cirrhosis of the liver?
The human liver is the main organ that protects the body from the effects of poisons. It takes the brunt of alcohol and neutralizes toxins. In this difficult and sometimes unequal struggle, it itself is gradually being destroyed. As a result, inflammation develops - hepatitis, which, with continued alcoholization and the destructive influence of alcohol, turns into alcoholic cirrhosis of the liver. This complication is life-threatening and, in the absence of sobriety and adequate treatment, leads to disastrous consequences. Therefore, the sooner the patient begins to get rid of this disease, the greater his chances of regaining health. Healing pathology is included in the tasks of the main course of anti-alcohol treatment. Hepatologists deal with advanced stages.
Causes of cirrhosis
According to statistics, about 50% of liver cirrhosis is associated with alcohol abuse and the development of alcoholic liver disease (ALD). 1Moreover, 25% of them had a history of viral hepatitis.1
Other causes of cirrhosis include2:
- metabolic diseases associated with excessive accumulation of iron, copper and other elements;
- Autoimmune lesions;
- Primary and secondary biliary cirrhosis;
- Diseases of the vascular system (Budd-Chiari disease);
- Long-term use of medications that have a toxic effect on the liver;
- non-alcoholic fatty liver disease (NAFLD), which is associated with the accumulation of large amounts of free fatty acids in hepatocytes (liver cells), is characterized by a chronic course and potential progression from stage to stage: steatosis - steatohepatitis - fibrosis - cirrhosis (same as alcoholic disease liver, but the likelihood of developing cirrhosis in AFLLD is 10 times higher).5
Regardless of the cause, cirrhosis develops in the same way: the lobular structure of the liver is disrupted with the formation of nodes in place of destroyed hepatocytes—the so-called false lobules.
- Small nodular - the size of fibrous nodes is no more than 3 mm;
- Large nodular - nodes 3-5 mm;
- Mixed.
How does alcoholic cirrhosis of the liver develop?
This painful process leads to the death of cells - hepatocytes. In their place, fibrous connective tissue appears, which forms the essence of cirrhotic changes. In the classification of all existing cirrhosis, alcoholic diseases occupy from 30 to 50%. Ethanol entering the blood is neutralized by hepatocytes. Free radicals released during detoxification destroy the cell membranes of the organ. Vessels also suffer from destruction. Their subsequent spasm and hypoxia lead to worsening destruction. The dead zones are replaced by fibrous formations. The main functions of the liver are gradually and progressively lost. In advanced stages they are irreversible. Only transplantation can help the patient. As a result of observing people who drink, it was revealed that the cirrhotic process develops in 35% of alcoholics. The disease occurs more often in men, and is more severe in women.
Why does the disease develop?
In the human body, the liver cleanses the blood of toxins and metabolic products, promotes the synthesis of nutrients and compounds necessary for life. These functions are performed by hepatocytes - special cells that make up the liver. If hepatocytes die, their place is taken by connective tissue, forming small (up to 3 mm in diameter) or large (over 3 mm) nodules. In this case, the organ either increases in size or decreases and becomes denser. Among the most significant causes of liver cirrhosis are:
- regular consumption of alcoholic beverages;
- previous viral hepatitis;
- autoimmune reactions of the body;
- congenital metabolic pathologies - hemochromatosis, hepatocerebral dystrophy, etc.);
- frequent contact with toxic chemicals due to work or place of residence;
- long-term use of hepatotoxic drugs;
- blockage of the biliary tract;
- dysfunction of the heart and/or blood vessels, leading to stagnation of blood in the liver.
In approximately half of patients, the disease develops under the influence of several factors simultaneously. The most common is a combination of viral hepatitis and alcohol intoxication. In about a third of patients, it is not possible to determine what exactly was the trigger for the development of the pathology. Such cases are called cryptogenic.
Classification
The disease is divided according to changes in the organ and severity. The following types of cirrhosis are distinguished:
- Small-knot.
- Large-knot.
- Mixed.
Stages of alcoholic cirrhosis of the liver:
- Compensated – without pronounced symptoms.
- Subcompensated – with initial manifestations, but with preservation of functions.
- Decompensated – accompanied by partial and then complete failure of functioning.
Compensatory stage
The onset of the disease is characterized by a slight intensity of manifestations. The patient periodically feels heaviness or discomfort on the right side in the hypochondrium - usually these sensations occur after eating or physical activity. Flatulence develops, performance decreases, periodic nausea and a bitter taste in the mouth are possible. The liver and spleen increase slightly in size. When you consult a doctor, it is quite easy to stop the development of the disease, preserving liver function.
Symptoms of the disease
As such, there are no symptoms at the early stage of compensation. On this basis, identifying the cirrhotic process is quite difficult. Therefore, the disease is not detected for the first few years. Initial suspicions arise against the background of hepatitis with increased organ size. When receiving compensation, the patient complains about:
- Decreased appetite and nausea.
- Emaciation.
- Weakness.
- Belching, heartburn, flatulence.
- Unpleasant sensations in the right hypochondrium.
When examining the patient, an increase in the size of the liver borders is determined. At the stage of subcompensation, the following is revealed:
- Severe asthenic syndrome: constant weakness and increased fatigue, apathy, depression.
- Great emaciation with aversion to food.
- Low blood pressure.
- Tachycardia.
- Redness of the skin of the face, hands and feet.
- Visible enlargement and palpation of the parotid glands.
- Specific obesity: thin limbs and fat deposits in the abdomen and thighs.
- Gynecomastia in men.
- Testicular atrophy, infertility, impotence.
- Changing fingers in the form of drumsticks.
- Yellowish skin with spider veins.
- Contractures of the muscles of the palms with gradual loss of their functions.
Decompensation is characterized by:
- Signs of portal hypertension with ascites - accumulation of fluid in the abdominal cavity.
- Rectal hemorrhoidal and esophageal (esophageal) bleeding.
- Jaundice with liver failure, enlarged spleen.
- Vomiting, complete lack of appetite, constant diarrhea.
- Coma.
- Hepatic encephalopathy with personality changes and disturbances of consciousness.
Palpation of the abdomen reveals a sharply compacted liver. High numbers of transferases indicate an advanced process. Cirrhosis is often complicated by dysfunction of the lungs, heart, and pancreas. Polyneuropathy appears on the part of the nervous system.
Diagnostic features
When identifying cirrhotic changes, the existing symptoms are taken into account. Additionally, clinical and biochemical blood tests are taken from patients.
They define:
- Anemia.
- Less commonly, leukocytosis.
- Decreased platelets.
- Increase in gamma globulins.
- Increase in AST (more) and ALT.
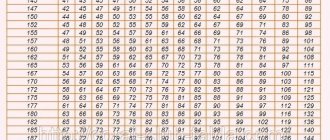
Ultrasound data plays an important role. They reveal a decrease in the size of the organ and foci of fibrosis. Computed tomography provides an even more accurate picture. With its help, not only the structure is assessed, but also pathological changes in nearby anatomical formations. Informative methods include elastography, and the most accurate is liver biopsy. All obtained data are examined using a special Child-Pugh scale, which allows you to accurately determine the phase of the disease: compensated, subcompensated, decompensated.
How to treat alcoholic cirrhosis of the liver
Therapy implies that the drinker must completely stop drinking alcohol. Only in this case is it possible to achieve a positive result. The second important condition for healing is the selection of a special diet. The food should be dominated by products containing a complete complex of proteins and vitamins. Fried, smoked, salted and preserved foods are excluded. These goals are best met by the fifth liver table. Drug therapy includes:
- Long-term use of hepatoprotectors.
- Ursodeoxycholic acid.
- Multivitamins. After the injection course, they continue to be given in tablets.
- Hormone therapy.
- Ademetionine is the best way to restore and stimulate hepatocytes, protecting them from destruction. It can improve the flow of bile, has detoxifying properties and protects the brain from the effects of poisons. It has an antidepressant effect.
- Protease inhibitors. With their help, inflammatory phenomena are reduced and fibrosis processes are prevented.
Treatment of complications includes eliminating the cause of portal hypertension (increased pressure in the hepatic vein system) by restricting blood flow in the veins of the esophagus. For this purpose they prescribe:
- Pituitary hormones.
- Nitrates.
- Beta blockers.
- Diuretics.
Lactulose is prescribed for intestinal detoxification and improvement of digestive processes. When ascites appears, large doses of diuretics and albumin are administered. Excess fluid from the abdominal cavity under the influence of drugs is actively excreted by the kidneys. When hepatic encephalopathy develops, the following is carried out:
- Active detoxification.
- Antibacterial therapy.
- Prescribing a special diet to minimize protein.
In case of complete liver failure, it is recommended to treat the patient in a surgical hospital for the purpose of organ transplantation.
Treatment of cirrhosis
Treatment of cirrhosis involves:
- Treatment of the underlying disease that led to the development of cirrhosis;
- Specific therapy for complications, including medications: for example, the prescription of diuretics for ascites, the prescription of antibiotics for spontaneous bacterial peritonitis, etc.
- Surgical treatment of ascites and bleeding from dilated veins of the esophagus and stomach1
Important components are diet, exclusion of harmful effects on the liver, such as alcohol, hepatotoxic drugs, treatment of concomitant chronic diseases.4 If the measures taken are ineffective, organ transplantation is indicated1.
How long do people live with alcoholic cirrhosis of the liver?
Prognostic expectations depend on the stage of the disease, complete abstinence from alcohol, the age of the patients, compliance with dietary recommendations and existing complications. The more advanced the form of the disease, the worse the survival rate. The answer to the question of clients of drug clinics: does alcohol cause cirrhosis of the liver is always an unequivocal yes.
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!