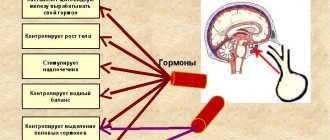
First, it’s worth understanding what hormones are?
They are produced by certain cells of the body, which are located in special organs. These organs are called endocrine glands. In order for them to function correctly and secrete a normal amount of hormones, their work is controlled by a whole cascade of endocrine regulation organs, namely: the hypothalamic-pituitary system, peripheral glands and the pineal gland.
The hypothalamus is the highest control center for hormonal levels. A signal goes from the hypothalamus to the pituitary gland whether it is necessary or not to release hormones.
The pituitary gland secretes a secretion that can either block or stimulate the production of hormones.
The peripheral glands include the thyroid and parathyroid glands, pancreas, ovaries in women and testes in men.
The pineal gland synthesizes melatonin. It works both day and night completely independently.
when should you get your hormones checked?
Hormonal screening for women
The choice of hormonal screening, that is, determining which hormones to give a woman, depends on the patient’s complaints, her age and the nature of the menstrual cycle.
From the second to the fifth day of the cycle, the level of pituitary hormones is assessed, which controls the functioning of the ovaries:
- LH (luteinizing hormone);
- FSH (follicle stimulating hormone);
- prolactin;
- AMH (anti-Mullerian hormone);
- inhibin B;
- estradiol;
- progesterone
To measure ovarian hormone levels, the test is performed on the seventh to ninth day of the menstrual cycle. The analysis determines the level of estradiol, testosterone and proteins that bind these hormones: globulin and albumin.
On days 19-22, the concentration of estradiol and progesterone is checked. These hormones should be given to women.
- Estradiol is a beauty hormone; rounded body shapes, timbre of voice, delicate skin, libido depend on it; it plays an important role in a girl’s puberty.
- Progesterone. The task of this hormone is to regulate the menstrual cycle and maintain pregnancy.
If the cycle is disrupted, the procedure for taking tests is selected by the doctor individually. This service can be ordered during your stay at the Mashuk Aqua-Therm sanatorium-resort complex - we conduct research on any day of the menstrual cycle. Our gynecologists treat such problems. The sanatorium has developed treatment programs that can be combined with recreation at a medical facility.
How to get examined?
All examinations are divided into planned and urgent. A routine examination is also carried out in the complete absence of symptoms, when screening is simply necessary. For example, due to iodine deficiency in many regions, all residents should have their thyroid-stimulating hormone tested periodically. If there are deviations from normal values, you should consult an endocrinologist. He will prescribe a list of further examinations to clarify the diagnosis.
If the patient has complaints, this is an indication for urgent examination. But not in every case, hormonal imbalance has external manifestations. Therefore, you should carefully monitor your health if the following symptoms appear:
- swelling,
- pigmentation,
- brittle nails,
- constant heat or cold,
- dry skin,
- hypo- or hypertension,
- obesity or malnutrition,
- myalgia,
- joint pain,
- constant fatigue
- short or tall,
- excessive sleepiness or insomnia,
- decreased performance.
The reason for consulting an endocrinologist is menstrual irregularities. Also, special attention should be paid to the control of sex hormones during menopause.
When do you need to donate blood for hormones?
Planning a pregnancy is an important and responsible stage that will require a full medical examination from future parents. Some couples will definitely need to undergo hormone tests.
Direct indications for their implementation are the following factors:
- The age of the spouses is over 35 years.
- Irregular menstruation in a woman.
- Failure to conceive within a year of regular sexual activity without contraception.
- History of miscarriage or miscarriage.
- Suspicion of the presence of benign and malignant formations.
- Obesity in one of the partners.
- Decreased libido.
What tests need to be taken?
There is a gender difference in the list of required hormones for testing. For example, in women these are: TSH, follicle-stimulating hormone, luteinizing hormone, prolactin, cortisol, testosterone, DHEA-S. If you have menstrual irregularities, you should definitely check your progesterone levels. If a woman has problems conceiving a child, she should definitely do a test for the level of anti-Mullerian hormone. Thanks to it, you can understand how many eggs are left in a woman’s body.
In case of pathology of the reproductive system in men, it is necessary to determine the amount of follicle-stimulating and luteinizing hormone, as well as prolactin and testosterone.
All other examinations are quite individual and are selected for each person separately by an endocrinologist. Hormonal tests should be carried out once a year for screening purposes, and more often in the presence of pathology.
what hormone tests should I take?
If you suspect diabetes, you need to check your glucose level. If the results are questionable, it is worth conducting a glucose tolerance test. A person must drink 75 grams of glucose, and then the sugar level must be measured again.
A comprehensive study of steroid hormones (mineralocorticoids, glucocorticoids and sex hormones), used in the diagnosis of “virilizing syndromes” (polycystic ovary syndrome, tumors of the gonads and adrenal glands, Cushing’s disease, congenital hyperplasia of the adrenal cortex), as well as in assessing the function of the hypothalamic-pituitary- adrenal system.
Synonyms Russian
Steroid hormones, mineralocorticoids, glucocorticoids and sex hormones.
English synonyms
Steroid hormones, Serum, Mineralocorticoids, glucocorticoids and sex hormones.
Research method
High performance liquid chromatography-mass spectrometry (HPLC-MS).
Units
ng/ml (nanograms per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid taking estrogens and androgens 48 hours before the test.
- Avoid physical and emotional stress for 24 hours before the test.
- Do not smoke 3 hours before the test.
General information about the study
The synthesis of steroid hormones is a multi-step process during which cholesterol (cholesterol), under the action of several enzymes, is converted into active compounds that perform various functions. Depending on their physiological effects, steroid hormones are divided into mineralocorticoids, glucocorticoids and sex hormones. Mineralocorticoids and glucocorticoids are formed only in the adrenal cortex, while sex hormones are produced both in the adrenal cortex and in the gonads and adipose tissue. The body reaches a certain concentration and ratio of steroid hormones, which is necessary for the normal development of the reproductive system and sexual characteristics, maintaining water-electrolyte balance and vascular tone, as well as adaptation to environmental factors. Violation of this ratio leads to the development of a wide range of diseases, among which the most important are the so-called virilizing syndromes (polycystic ovary syndrome, Cushing's disease, adenoma and carcinoma of the adrenal cortex (Cushing's syndrome), as well as congenital hyperplasia of the adrenal cortex). It is important to note that differential diagnosis of these diseases cannot be carried out on the basis of clinical signs alone; it is based on a comprehensive determination of the level of steroid hormones and their precursors (12 compounds in total). This analysis allows for simultaneous assessment of all three groups of steroid hormones. Thus, corticosterone and deoxycorticosterone are precursors of aldosterone, and therefore measuring their concentration allows us to assess the characteristics of the synthesis of mineralocorticoids in the body. Determination of the level of 17-OH-progesterone (17-OPG), 21-deoxycortisol, cortisol and cortisone allows us to characterize the stages of glucocorticoid synthesis. Progesterone, androstenedione, dehydroepiandrosterone (DHEA) and testosterone are sex hormones.
A comprehensive analysis of steroid hormones is a mandatory component of the differential diagnosis of congenital adrenal hyperplasia - adrenogenital syndrome - a group of autosomal recessive enzymopathies accompanied by impaired synthesis of steroid hormones. Depending on the severity of the disease, adrenogenital syndrome can manifest itself in childhood, adolescence or adulthood. Its most common form (95% of cases) is caused by 21-hydroxylase deficiency, which impairs the synthesis of cortisol and aldosterone. A characteristic laboratory sign of 21-hydroxylase deficiency is a significant increase in the level of 17-OPG, DHEA, androstenedione and testosterone with a significant decrease in corticosterone, deoxycorticosterone and cortisol. It should be noted that only with the help of a comprehensive study of steroid hormones is it possible to differentiate 21-hydroxylase deficiency from another, more rare variant of adrenogenital syndrome - 11-beta-hydroxylase deficiency, since both enzymopathies have a similar clinical picture. Unlike 21-hydroxylase deficiency, 11-beta-hydroxylase deficiency is characterized by an excess of deoxycorticosterone. With the help of a comprehensive study of sex hormones, other forms of adrenogenital syndrome (17-alpha-hydroxylase, 3-beta-hydroxysteroid dehydrogenase deficiency) can be diagnosed.
In addition, a comprehensive study of steroid hormones can be used to assess the function of the hypothalamic-pituitary-adrenal axis when examining a patient with signs of adrenal insufficiency.
When interpreting the study results, some features of steroid metabolism should be taken into account. Most of the steroid hormones are in the blood in a bound state (bound to steroid-binding globulin, sulfated), that is, inactive. The proportion of active hormone depends on the physiological state of the body, the use of certain medications, and concomitant pathologies. Normally, only a third of the total amount of steroid hormones is present in a free state and is responsible for the effects manifested in target organs. The study allows you to determine the total amount of steroid hormones in the blood serum (the active and bound fractions of the hormone are not assessed separately). In addition, the effect of steroid hormones can be modified by their interaction with other hormonally active compounds at the level of binding to specific receptors, so the test result does not always correlate with the severity of the clinical manifestations of virilization syndrome. In other words, the study allows us to assess the concentration of steroid hormones, but not their bioactivity in the body.
What is the research used for?
- To diagnose diseases manifested by virilization syndrome;
- for differential diagnosis of clinical forms of adrenogenital syndrome;
- to assess the function of the hypothalamic-pituitary-adrenal system in a patient with signs of adrenal insufficiency.
When is the study scheduled?
- When examining a patient with symptoms of hyperandrogenism (hair growth above the upper lip, on the chin, the “white line” of the abdomen, severe acne, changes in voice timbre, clitoromegaly, increased muscle mass);
- when examining an infant with signs of impaired gender differentiation (external genitalia with characteristics of both female and male gender);
- when examining a patient with signs of adrenal insufficiency (weakness, fatigue, nausea, vomiting, loss of muscle mass and weight, appetite disturbances, hypotension, disturbances of consciousness).
What do the results mean?
Reference values
- Cortisone
| Age | Reference values |
| 1-7 days | 26-156 ng/ml |
| 7-14 days | 3-45 ng/ml |
| 2 weeks — 3 months | 9-54 ng/ml |
| 3 months - 1 year | 7-46 ng/ml |
| 1 year - 17 years | 6-30 ng/ml |
| Adults (morning) | 12-35 ng/ml |
| Adults (evening) | 6-28 ng/ml |
- Cortisol
| Age | Reference values |
| 1 month — 1 year (morning) | 46-230 ng/ml |
| 1 year - 6 years (morning) | 60-250 ng/ml |
| 6 – 18 years (morning) | 46-150 ng/ml |
| Adults (morning) | 46-206 ng/ml |
| Adults (evening) | 18-136 ng/ml |
- Corticosterone
| Age | Reference values |
| 1 – 17 years (morning) | 1.35-18.6 ng/ml |
| 1 – 17 years (evening) | 0.7-6.2 ng/ml |
| Over 17 years old (morning) | 1.3-8.2 ng/ml |
| Over 17 years old (evening) | 0.6-2.2 ng/ml |
- Deoxycorticosterone
| Age | Reference values |
| 1 month - 1 year | 0.07-0.49 ng/ml |
| 1-7 years | 0-0.37 ng/ml |
| 7-14 years | 0-0.34 ng/ml |
| More than 14 years | 0-0.19 ng/ml |
- 21-deoxycortisol
| Floor | Age | Reference values |
| Female | 7-10 years | 0-0.94 ng/ml |
| 10-13 years | 0-0.74 ng/ml | |
| 13-16 years old | 0-0.64 ng/ml | |
| 16-18 years old | 0-0.47 ng/ml | |
| Over 18 years old | 0-0.33 ng/ml | |
| Male | 7-10 years | 0-0.59 ng/ml |
| 10-13 years | 0-0.89 ng/ml | |
| 13-16 years old | 0-0.71 ng/ml | |
| 16-18 years old | 0-0.88 ng/ml | |
| Over 18 years old | 0-0.68 ng/ml |
- Progesterone, ng/ml
| Male | 1-17 years | 0.0-0.15 |
| Over 17 years | 0.0-0.11 | |
| Female | 1-11 years | 0.0-0.26 |
| 11-12 years old | 0.0-2.55 | |
| 12-13 years old | 0.0-8.56 | |
| 13-14 years old | 0.0-6.93 | |
| 14-15 years old | 0.0-12.04 | |
| 15-16 years old | 0.0-10.76 | |
| 16-17 years old | 0.0-12.94 | |
| More than 17 years, by cycle phases | Menstrual (1-6th day) | 0.0-0.17 |
| Folliculin (proliferative) (3-14th day) | 0.0-1.35 | |
| Ovulatory (day 13-15) | 0.0-15.63 | |
| Luteal (15th day - beginning of menstruation) | 0.0-25.55 | |
| Postmenopause | 0.0-0.1 | |
| 1-12th week Bertie | 6.25-45.46 | |
| 12-24th week. Bertie | 15.4-52.1 | |
| 24 or more weeks Bertie | 24.99-99.92 |
- 17-OH-progesterone
| Floor | Age | Reference values | |
| Female | 4 days – 1 month | 0.07-1.06 ng/ml | |
| 1 month – 1 year | 0.13-1.6 ng/ml | ||
| 1-7 years | 0.04-1.15 ng/ml | ||
| 7-10 years | 0-0.71 ng/ml | ||
| 10-13 years | 0-1.29 ng/ml | ||
| 13-16 years old | 0.09-2.08 ng/ml | ||
| 16-18 years old | 0-1.78 ng/ml | ||
| Over 18 years old | 0-2.07 ng/ml | ||
| Cycle phase | Folliculin (proliferative) | 0.15-0.7 ng/ml | |
| Luteal (day 15 – before the start of menstruation) | 0.35-2.9 ng/ml | ||
| Menstrual (1-6 days) | 0.15-0.7 ng/ml | ||
| Male | 4 days – 2 months | 0-2 ng/ml | |
| 2-12 months | 0.03-0.9 ng/ml | ||
| 1-7 years | 0.04-1.15 ng/ml | ||
| 7-10 years | 0-0.63 ng/ml | ||
| 10-13 years | 0-0.79 ng/ml | ||
| 13-16 years old | 0.09-1.4 ng/ml | ||
| 16-18 years old | 0.24-1.92 ng/ml | ||
| Over 18 years old | 0.15-0.7 ng/ml | ||
- Testosterone, ng/ml
| Female | Up to 30 days | 0.2-0.64 |
| 1-6 months | 0.0-0.2 | |
| 6 months - 2 years | 0.0-0.09 | |
| 2-4 years | 0.0-0.2 | |
| 4-6 years | 0.0-0.3 | |
| 6-8 years | 0.0-0.07 | |
| 8-10 years | 0.01-0.11 | |
| 10-12 years | 0.03-0.32 | |
| 12-14 years old | 0.06-0.5 | |
| 14-16 years old | 0.06-0.52 | |
| 16-18 years old | 0.09-0.58 | |
| 18-60 years | 0.09-0.55 | |
| Over 60 years | 0.05-0.32 | |
| Male | Up to 1 month | 0.75-4 |
| 1-6 months | 0.14-3.63 | |
| 6 months - 2 years | 0-0.37 | |
| 2-4 years | 0-0.15 | |
| 4-6 years | 0-0.19 | |
| 6-8 years | 0-0.13 | |
| 8-10 years | 0.02-0.08 | |
| 10-12 years | 0.02-1.65 | |
| 12-14 years old | 0.03-6.19 | |
| 14-16 years old | 0.31-7.33 | |
| 16-18 years old | 1.58-8.26 | |
| 18-40 years old | 3-10.80 | |
| 40-60 years | 3-8.9 | |
| Over 60 years | 3-7.2 |
- Dehydroepiandrosterone, ng/ml
| Female | Up to 2 days | 0-11 | |
| 2-7 days | 0-8.7 | ||
| 7 days - 1 month | 0-5.8 | ||
| 1-6 months | 0-2.9 | ||
| 6 months — 2 years | 0-1.99 | ||
| 2-4 years | 0-0.85 | ||
| 4-5 years | 0-1.03 | ||
| 6-8 years | 0-1.79 | ||
| 8-10 years | 0.14-2.35 | ||
| 10-12 years | 0.43-3.78 | ||
| 12-14 years old | 0.89-6.21 | ||
| 14-16 years old | 1.22-7.01 | ||
| 16-18 years old | 1.42-9.00 | ||
| 18-40 years old | 1.33-7.78 | ||
| More than 40 years | 0.63-4.70 | ||
| More than 40 years | Postmenopause | 0.6-5.73 | |
| By cycle phases | 18-40 years old | Menstrual (1-6th day) | 1.33-7.78 |
| Folliculin (proliferative) (3-14th day) | 1.33-7.78 | ||
| Ovulatory (day 13-15) | 1.33-7.78 | ||
| Luteal (15th day - beginning of menstruation) | 1.33-7.78 | ||
| Pregnancy | 1.33-7.78 | ||
| Premenopause | 1.33-7.78 | ||
| More than 40 years | Menstrual (1-6th day) | 0.63-4.70 | |
| Folliculin (proliferative) (3-14th day) | 0.63-4.70 | ||
| Ovulatory (day 13-15) | 0.63-4.70 | ||
| Luteal (15th day - beginning of menstruation) | 0.63-4.70 | ||
| Pregnancy | 0.63-4.70 | ||
| Premenopause | 0.63-4.70 | ||
| Male | Up to 2 days | 0-11 | |
| 2-7 days | 0-8.7 | ||
| 7 days - 1 month. | 0-5.8 | ||
| 1-6 months | 0-2.9 | ||
| 6 days - 2 years | 0-2.5 | ||
| 2-4 years | 0-0.63 | ||
| 4-6 years | 0-0.95 | ||
| 6-8 years | 0.06-1.93 | ||
| 8-10 years | 0.10-2.08 | ||
| 10-12 years | 0.32-3.08 | ||
| 12-14 years old | 0.57-4.10 | ||
| 14-16 years old | 0.93-6.04 | ||
| 16-18 years old | 1.17-6.52 | ||
| 18-40 years old | 1.33-7.78 | ||
| More than 40 years | 0.63-4.70 |
- Androstenedione
| Female | Up to 8 days | 0.2-2.9 |
| 8 days — 1 month | 0.18-0.8 | |
| 1-6 months | 0.06-0.68 | |
| 6 months - 2 years | 0-0.15 | |
| 2-4 years | 0-0.16 | |
| 4-6 years | 0.02-0.21 | |
| 6-8 years | 0.02-0.28 | |
| 8-10 years | 0.04-0.42 | |
| 10-12 years | 0.09-1.23 | |
| 12-14 years old | 0.24-1.73 | |
| 16-18 years old | 0.35-2.12 | |
| 18-40 years old | 0.26-2.14 | |
| More than 40 years | 0.13-0.82 | |
| Male | Up to 8 days | 0.2-2.9 |
| 8 days — 1 month | 0.18-0.8 | |
| 1-6 months | 0.06-0.68 | |
| 6 months - 2 years | 0.03-0.15 | |
| 2-4 years | 0-0.11 | |
| 4-6 years | 0.02-0.17 | |
| 6-8 years | 0.01-0.29 | |
| 8-10 years | 0.03-0.30 | |
| 10-12 years | 0.7-0.39 | |
| 12-14 years old | 0.1-0.64 | |
| 14-16 years old | 0.18-0.94 | |
| 16-18 years old | 0.3-1.13 | |
| 18-40 years old | 0.33-1.34 | |
| More than 40 years | 0.23-0.89 |
- 11-deoxycortisol
| Floor | Age | Reference values, ng /ml |
| Female | 1-6 months | 0,1 — 2 |
| 6 months - 1 year | 0,1 — 2,76 | |
| 1-4 years | 0,07 — 2,47 | |
| 4-7 years | 0,08 — 2,91 | |
| 7-10 years | 0 — 0,94 | |
| 10-13 years | 0 — 1,23 | |
| 13-16 years old | 0 — 1,07 | |
| 16-18 years old | 0 — 0,47 | |
| Over 18 years old | 0 — 0,55 | |
| Male | 1-6 months | 0,1 — 2 |
| 6 months - 1 year | 0,1 — 2,76 | |
| 1-4 years | 0,07 — 2,02 | |
| 4-7 years | 0,08 — 2,35 | |
| 7-10 years | 0 — 1,2 | |
| 10-13 years | 0 — 0,92 | |
| 13-16 years old | 0 — 0,95 | |
| 16-18 years old | 0 — 1,06 | |
| Over 18 years old | 0 — 0,59 |
- 17-OH-pregnenolone
| Floor | Age | Reference values, ng /ml |
| Female | 1-6 months | 2,29 — 31,04 |
| 6 months – 1 year 1 month. | 0 — 9,17 | |
| 1 year 1 month - 2 years | 0 — 5,92 | |
| 2-5 years | 0 — 2,8 | |
| 5-7 years | 0 — 3,5 | |
| 7-10 years | 0 — 2,12 | |
| 10-13 years | 0 — 3,98 | |
| 13-16 years old | 0 — 4,07 | |
| 16-18 years old | 0 — 4,23 | |
| Over 18 years old | 0 — 2,26 | |
| Male | 1-6 months | 2,29 — 31,04 |
| 6 months – 1 year 1 month. | 0 — 9,17 | |
| 1 year 1 month - 2 years | 0 — 5,92 | |
| 2-5 years | 0 — 2,49 | |
| 5-7 years | 0 — 3,19 | |
| 7-10 years | 0 — 1,87 | |
| 10-13 years | 0 — 3,98 | |
| 13-16 years old | 0,35 — 4,65 | |
| 16-18 years old | 0,32 — 4,78 | |
| Over 18 years old | 0 — 4,42 |
Characteristic laboratory parameters for the most common “virilizing syndromes”
- Polycystic ovary syndrome: increased concentrations of testosterone, dehydroepiandrosterone and androstenedione with normal values of glucocorticoids and mineralocorticoids.
- Cushing's syndrome: increased concentrations of cortisol and cortisone with normal values of mineralocorticoids and sex hormones.
- Congenital adrenal hyperplasia (21-hydroxylase deficiency): increased levels of 17-OH-progesterone, dehydroepiandrosterone, androstenedione and testosterone with a significant decrease in corticosterone, deoxycorticosterone and cortisol.
- Congenital adrenal hyperplasia (11-hydroxylase deficiency): increased levels of 17-OH-progesterone, dehydroepiandrosterone, androstenedione, testosterone and deoxycorticosterone with a significant decrease in corticosterone and cortisol.
Typical laboratory parameters for primary adrenal insufficiency:
- Decreased levels of corticosterone, deoxycorticosterone, 17-OH-progesterone, 21-deoxycortisol, cortisol and cortisone with normal concentrations of sex hormones.
What can influence the result?
- The result of the analysis may be influenced by the performance of diagnostic studies using radiocontrast agents within 7 days before the examination.
- The concentration of steroid hormones depends on the time of day - it reaches a maximum in the morning and decreases in the evening.
What to do after the examination?
If the problem is identified, you need to contact a specialist. If we are talking about gynecological pathology, you need to consult a gynecologist-endocrinologist. If problems arise in a man, then you need to consult an andrologist. Together with a specialist, the person will undergo additional research and begin appropriate therapy. Hormone therapy is a lengthy process and takes from three to six months. After therapy it is necessary to carry out monitoring.
If there are deviations from the norm in the tests, you should urgently consult an endocrinologist.
What is a hormonal study?
Hormones are different in chemical structure, but equally highly active biological substances secreted by the endocrine glands (thyroid, parathyroid, thymus, adrenal glands, pituitary gland, hypothalamus and others) directly into the circulatory system.
A hormonal blood test can be prescribed by a general practitioner and specialized doctors: endocrinologist, gastroenterologist, gynecologist, neurologist, urologist and others, depending on the suspicion of dysfunction of certain organs.
Indications for checking hormones in men
In men, it is recommended to check the concentration of hormones in the blood for various disorders:
- examination for infertility;
- suspected testicular tumor;
- kidney disease with impaired adrenal function;
- to clarify the nature of obesity;
- in adolescence with widespread acne on the face and chest skin;
- growing too quickly or falling behind age standards;
- the appearance of swelling of the mammary glands.
Men suffer no less than women from the lack of heirs
A study of thyroid function in boys and adult men is carried out to diagnose thyrotoxicosis, and in the case of reduced function, the possibility of influencing the mental development of the child is identified.