Tendonitis is a process of inflammation that occurs where a muscle connects to a bone. This disease belongs to fatigue diseases of the musculoskeletal system of the body, since its development occurs against the background of deteriorating tissue condition. Standard medications that relieve pain and inflammation are ineffective for this problem. They help relieve discomfort and eliminate symptoms, but cannot cure the disease.
Knee tendonitis is an inflammatory process that occurs in the tendon above the knee. It connects the thigh muscle to the tibia. Hip tendonitis is an inflammation of the tissues and ligaments that surround the joint. There is also tendinitis of the tendons that are located in the area of the ischial tuberosity. This process is considered the most dangerous to human health, so its treatment must be started immediately after the diagnosis has been made. If this is not done, the tendonitis will develop into a pinched sciatic nerve.
Elbow joints may also suffer from a similar condition, but it may have different names depending on the specific location of the problem. It is popularly called “baseball elbow.”
Many people confuse tendinosis with stretched or torn tendons. But they have a significant difference. When tendons are mechanically injured, some fibers are torn and soon begin to grow together and heal. The affected area brings discomfort and acute pain to the person, so he is forced to reduce the load on it. With tendonitis, tissue rupture occurs constantly, and their healing is always at different stages. The load on the affected area is not reduced. It is for this reason that treatment may be delayed, and the disease becomes chronic.
Stages of tendinitis
Modern medicine distinguishes several stages of this disease. These include:
- Acute phase. The damaged area of the body causes severe pain. If a person feels discomfort in a calm state, then with physical activity it develops into unbearable acute pain;
- Subacute phase. The pain persists and is accompanied by swelling. Movements become difficult and limited;
- Chronic phase. Tissue degeneration occurs. Pain becomes a constant “guest”, as does stiffness.
Diagnostics
To establish a diagnosis of ankle tenosynovitis, you should initially conduct a visual examination of the area of inflammation. During palpation, the doctor will clearly see swelling, stiffness in the joint, and acute pain in the patient.
In order to distinguish this disease from arthritis, a person should undergo an x-ray. To accurately track the nature of tendon inflammation, MRI is used.
A correctly established diagnosis allows you to successfully select treatment. Otherwise, a person will only waste precious time. At the same time, it is worth differentiating tenosynovitis from other common joint lesions that may have similar symptoms.
In laboratory tests of such patients, the level of leukocytes and ESR are always elevated, which indicates an acute spreading inflammatory process.
Modern classification of the disease
Tendonitis can be different. There is a certain classification, which is based on the characteristics of inflammation and methods of its treatment. Today, doctors distinguish between serous, purulent, and fibrous inflammatory processes.
Tendinosis is also divided according to the place of its occurrence. There are such tendinitis:
- Temporal.
It causes difficulty chewing food. When the jaw opens, a clicking sound may occur. Often the process is accompanied by discomfort or pain;
- Tendonitis of the shoulder joint.
The disease affects the capsule, which serves as the connection of the tendon with the supraspinatus and biceps muscles. Only an experienced specialist can help solve this problem. With tendinosis of the shoulder joint, the patient cannot fully raise his arm up or move it behind his head;
- Biceps tendonitis
leads to impairment and stiffness of hand movements;
- The disease that affected elbow joint
, does not allow full flexion and extension of the limb in this place. Accompanied by severe pain during physical activity and movement;
- Wrists.
It makes itself felt after physical activity. The patient feels stiffness in his hands, and is also unable to bend and straighten his fingers;
- Hip joint.
It is difficult for a person with this disease to move, let alone run or perform other more intense physical activities. After some time, the joint becomes permanently dysfunctional;
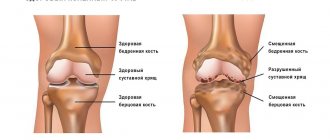
- Knee joint.
With this disease, the tendon in this area is affected. Damage can lead to partial or complete degeneration. The reason is the constant wearing of uncomfortable high-heeled shoes, as well as physical training to the limit. If adequate treatment is not provided, the patient may remain crippled for life;
- Achilles tendon
. Most often, professional athletes and heavy physical labor workers suffer from this problem. The disease is characterized by the presence of painful sensations even at rest. The pain intensifies when walking up stairs, and there is a feeling of stiffness in the joint;
- Feet.
In this case, the pain extends not only to the lesion, but also “radiates” to the lower leg. If you do not undergo treatment, then over time nodules appear in the foot, which make it difficult to move the leg;
Whatever type of tendonitis bothers you, it is important to consult a doctor in time so that he can conduct an examination and prescribe the necessary medications. Self-medication is not only ineffective, but also unsafe for health.
Which joints are most often affected?
A tendon connects bones or bones and muscles. It is covered on top with connective tissue, and on the inside with a synovial membrane that secretes lubricant for better gliding and movement of the limbs. The inflammatory process leads to disruption of this process. Sliding slows down and pain occurs.
Most often, inflammation affects the tendons of the forearm, hand, wrist, ankle and foot. Tenosynovitis can be acute or chronic. If, when the first signs of the disease appear, a person does not carry out effective treatment, does not fight inflammation and pain, and after the clinical manifestations subside, he continues to load the tendon, then the disease begins to recur frequently. Dystrophy of the tendon sheaths occurs, and motor activity drops sharply.
Up to contents
Causes of joint tendonitis
Many people are interested in the question, where does this disease come from? Most often it occurs in two categories of people. The first is professional athletes who train often, for a long time and for wear and tear. This excessive stress on the body leads to damage to tendons and joints. The second is the age category of people who have “passed” forty. In this case, the cause of tendonitis is age-related disorders in the body.
Damage due to excessive physical activity can be caused by a variety of factors:
- If you start doing exercises without the necessary warm-up and warm-up, and also if you systematically violate the technique of performing them;
- Problems in the hip joint appear when running technique is violated. The foot does not land on the ground correctly, the joint suffers from an impact on a hard surface, since the foot is at the wrong angle;
- Exercises that involve sudden jumps, bends, and turns can also provoke the appearance of a similar problem;
- Using incorrect and uncomfortable shoes when we are talking about outdoor activities and not in the gym;
- Problems with the elbow joint are caused by sudden movements of the hands, accompanied by a violation of the technique of performing exercises. As well as constantly performing the same movement with frequent intervals;
- If you apply too much weight during exercise, tendinitis of the shoulder joint may occur.
The anatomical features of the human skeleton can also cause this disease. For example, problems in the hip joint may be caused by unequal leg lengths. Custom-made shoes with soles of different heights can help the situation. Problems in the knee joints often cause bowed legs or dislocated joints.
The older a person gets, the less elastin fibers he contains in his body. They are responsible for the mobility and elasticity of tendons. At the same time, the number of collagen fibers increases. They are responsible for the strength of fabrics. Therefore, this leads to the development of tendinosis.
In rare cases it may be caused by:
- infectious diseases that are sexually transmitted;
- metabolic disorders;
- mechanical injuries in the place where the tendons are located;
- autoimmune diseases.
What triggers the development of tenosynovitis?
Experts include the following provoking factors:
- microtrauma of tendons;
- heavy physical work associated with joint overload;
- bruises from an accidental fall on a sharply bent or straightened limb;
- spread of infection to the tendons and their sheaths with osteomyelitis, infectious arthritis, phlegmon;
- toxic reactive inflammation of tendons with rheumatic joint damage;
- entry of pathogens into joint structures through the bloodstream during tuberculosis, gonorrhea or other infectious diseases.
Up to contents
Symptoms of tendinitis
This disease comes with several different symptoms. But the most obvious of them is pain. At the initial stage, discomfort may be noticeable only after physical exertion or hard work. Over time, they visit a person with enviable regularity. The sensation can be described as a dull pain, which is concentrated at the site of tissue inflammation. At the same time, it appears only during the movement. When the joint is at rest, the discomfort disappears. If you press on the area of the body where the disease has begun to develop, the pain becomes stronger.
If the inflammation is in an advanced state, then a symptom of tendonitis is redness of the skin around the affected tendon, as well as a local increase in temperature. The joint loses mobility, in some cases a characteristic crunch appears when the body moves.
Elastic nodules in the tissue that can be palpated are also a symptom of tendinitis. They occur after prolonged treatment. There may be one or several nodules. They are an accumulation of fibrous tissue that appears in place of inflammation.
A symptom of shoulder tendonitis may be the appearance of calcifications. These are denser nodules that represent an accumulation of salt deposits. Very often, tendinosis ends in tissue rupture, which leads to longer treatment and rehabilitation.
Survey
Inspection
Evaluation of a patient with signs and symptoms of de Quervain's tenosynovitis should begin with a thorough history followed by a physical examination.
History taking
- Overuse injury or acute injury.
- Have symptoms appeared before?
- Repetitive hand movements during work or daily activities.
- The pain is localized above the base of the thumb and in the dorsolateral region of the wrist near the styloid process of the radius.
- One hand dominance.
- Pregnancy or postpartum period.
Physical examination
Vital Signs
- Height.
- Weight.
- HELL.
- Pulse.
- NPV.
- Temperature (if required).
In a sitting position
- Resting hand/thumb position.
- Inflammation around the base of the finger on the dorsal side and/or near the styloid process of the radius.
Neurological examination
If you have symptoms such as numbness and tingling, as well as pain, it is necessary to conduct a neurological examination and check whether the symptoms are associated with pathology in the cervical spine. It is important to determine whether the central nervous system is involved in the process, whether the sensitivity of the skin at the base of the thumb and index finger is reduced (this area is innervated by the superficial branches of the radial nerve). Pay attention to a symptom such as hand weakness and determine whether it is due to pain or a neurological problem.
Dermatomes (C4-T1)
- Myotomes (C4-T1).
- Reflexes (C5, C6, C7).
- Pathological Hoffman reflex.
Palpation
During palpation, the most significant will be the detection of such a deviation as painful sensitivity over the base of the thumb and/or the 1st compartment of the wrist extensors above the styloid process of the radius. It is also possible to palpate the thickening of the synovial vagina. It is very important to rule out arthritis or a fracture of the scaphoid by palpating the first carpometacarpal joint to determine whether there is tenderness or deformity there.
- Dorsoradial region.
- Styloid process of the radius.
- “Anatomical snuffbox” - scaphoid, trapezius, extensor digitorum longus, extensor pollicis brevis, abductor pollicis longus and first carpometacarpal joint.
- Soft tissue surrounding the affected area.
Range of motion
Range of motion can also be used as a screening tool to rule out involvement of the cervical spine, proximal joints, and anatomical structures. Note any deviations in range of motion and be aware that when testing the thumb, there may be a clicking sound and a feeling of “sticking” in the thumb. All this is associated with reduced tendon mobility.
- Range of motion in the cervical spine.
- Flexion, extension, adduction and abduction of the shoulder (right and left).
- Flexion and extension in the elbow joint (right and left).
- Pronation and supination of the forearm (right and left).
- Wrist: Flexion, extension, ulnar and radial deviation.
- Fingers two to five:
- Abduction and adduction in the metacarpophalangeal joints.
- Flexion and extension (in the metacarpal, metacarpophalangeal and interphalangeal joints).
- Abduction and adduction (in the metacarpal-carpal, metacarpophalangeal joints).
- Opposition.
Muscle tests with resistance
In the presence of pain, strength naturally decreases. Note the maximum force possible in the absence of pain. This data will be useful in tracking the patient's progress during treatment.
- Grip strength.
- Pinch strength (finger squeezing force).
Muscle length
Watch for signs of hyper/hypomobility. Treatment will be prescribed based on dysfunction. Keep in mind that areas of hypomobility are often areas of referred pain.
- Congenital flexibility (clawed hand symptom).
- Extensors and flexors of the wrist.
Joint mobility
- Distal radioulnar joint.
- Wrist joint.
- Midcarpal joint.
- Thumb.
- Metacarpal, metacarpophalangeal and interphalangeal joints.
- Brush.
- Intercarpal joints.
Specific tests
Finkelstein test
- To confirm - Finkelstein test.
- To exclude: test for osteoarthritis of the first metacarpal joint (Grind Test);
- palpation to identify a scaphoid fracture;
- Upper Limb Tension Test, or ULTT B - to determine neuritis of the superficial sensory branch of the radial nerve;
- assessing the clinical likelihood of cervical radiculopathy;
- intercarpal instability.
Neurological tests
- Upper Limb Tension Test, or ULTT B.
- Test to detect damage to the radial nerve.
- Test to detect damage to the superficial sensory branch of the radial nerve.
- Tinel's sign.
Be careful with the position of your thumb while performing tests.
Circulation
- Pallor/Capillary refill.
- It is important to use the capsule-ligamentous apparatus in the acute phase of traumatic injury.
- Stress test of the collateral ligaments of the fingers (varus/valgus).
Tendonitis in pregnant women and its features
This disease is a frequent “guest” of women who are expecting a child. If there are suspicions, then it is preferable not to do an x-ray or computed tomography during the examination. Any medications that a pregnant woman will take must be prescribed by the attending physician and also agreed with the gynecologist. In this case, self-medication will be dangerous not only for the patient, but also for her unborn child.
When the first symptoms of tendinitis appear, doctors advise limiting yourself to physical therapy, rest, and applying cold compresses to the affected area. If you need to relieve inflammation and reduce pain, ointments based on painkillers are prescribed.
If the problem enters an acute phase, the doctor may resort to immobilization of the joint. Antibiotics may be prescribed, but only if a bacterial infection is found and other treatments have been ineffective. In the most extreme cases, surgery is performed on the joint.
Clinical picture
Clinical picture of de Quervain's tenosynovitis
The main complaint of patients is pain in the wrist on the side of the radius, which radiates to the forearm when trying to grab something with the thumb or straighten it. The pain is described as “constantly aching, burning, twitching.” Often the pain is aggravated when performing grasping, squeezing or twisting movements. Examination may reveal swelling in the area of the anatomical snuffbox, tenderness in the area of the styloid process of the radius, decreased range of motion in the first metacarpal joint, palpable thickening of the first dorsal compartment, and tendon crepitus. Other symptoms include weakness and paresthesia of the hand. These symptoms appear with a positive Finkelstein diagnostic test.
Features of the development of tendinitis in children
This disease does not occur as often in children as in adults. The most “popular” place where tendinosis occurs is the knee joint. At the first symptoms of tendonitis in a child, you need to contact a pediatric traumatologist. He will conduct an examination and make an accurate diagnosis. After this, the little patient will be prescribed the necessary medications. Most often, the list includes muscle relaxants and non-steroidal anti-inflammatory drugs, both for oral administration and in the form of ointments.
For a certain period of time, you will have to limit your mobility and remove all physical activity. If the pain is very severe, the joint is immobilized. Treatment includes a variety of physical therapy, including electrophoresis. As soon as the acute phase of the disease has passed, a course of massages is carried out and physical therapy is added.
Kinds
Tenosynovitis of the fingers can be infectious and aseptic. The latter occurs as a result of damage to the inner lining of the tendon sheath and is not associated with the introduction of bacteria or viruses. Infectious diseases are classified depending on the species of microorganisms. The cause of the development of nonspecific tendovaginitis is the introduction of Staphylococcus aureus and epidermal Staphylococcus, Streptococcus, and Escherichia coli. Specific pathology is provoked by pathogens of gonorrhea, brucellosis, tuberculosis, and syphilis. In orthopedics, it is also customary to subdivide tenosynovitis as follows:
- professional aseptic. Its development is preceded by overload and microtrauma of the tendon sheath with monotonous frequent movements. The resulting inflammatory process can lead to destructive and degenerative changes in connective tissue structures;
- reactive aseptic. Occurs as a result of the immune system's response to the introduction of foreign proteins. Most often diagnosed in patients with local circulatory disorders, rheumatic pathologies
Tendinitis of the fingers can manifest itself acutely, with pronounced clinical manifestations. A chronic disease is characterized by alternating remissions with relapses that occur after hypothermia or excessive physical exertion.
Complications after tendinitis
Like any other disease, tendon tendinitis can have complications. It is not difficult to avoid them if you start the right treatment on time. However, it may happen:
- tissue ruptures;
- chronic course of the disease, which is accompanied by constant pain;
- processes of bone tissue proliferation, which lead to inflammation of various types.
Timely examination by a doctor and compliance with all his instructions will minimize the likelihood of complications.
Methods for diagnosing and treating the disease
Early diagnosis of the disease is extremely important for timely initiation of treatment for tenosynovitis. Determining an acute aseptic and infectious nonspecific process is not difficult, since the clinical picture in these forms of the disease is significantly pronounced and specific.
Due to the fact that the symptoms of specific tendovaginitis are vague and have a subacute course, its diagnosis requires:
- a comprehensive analysis of the patient’s medical history and anamnesis of the development of the disease;
- collecting purulent masses from the lesion to determine the pathogen;
- in some cases (if the development of sepsis is suspected), a venous blood test for sterility is necessary.
Treatment of tendinitis
It is important that treatment for this disease is prescribed by a doctor. The first step is to remove excess stress on the joint whose tendons are inflamed. It is not necessary to completely immobilize an arm or leg. You can simply “take care” of your limbs and not put unnecessary strain on them physically. In order to reduce mobility, elastic bandages, bandages, and bandages are useful. Exercise therapy may be prescribed, which should be carried out by an experienced rehabilitation therapist. Properly selected exercises will not only relieve muscle tension, but also strengthen them.
To relieve the pain that always accompanies tendonitis, doctors prescribe non-steroidal anti-inflammatory drugs. They are available in the form of ointments and creams, as well as tablets for oral administration.
In some cases, treatment with glucocorticoid injections will be effective, but it should be remembered that such injections can provoke tendon rupture. Physiotherapy, which is used in combination with drug treatment, will also be useful. If a large amount of calcifications and salt deposits were found in the inflamed area, then shock wave therapy will help break them up.
If the sciatic nerve is pinched due to inflammation of the hip joint, the doctor may prescribe surgery to eliminate the underlying problem. In this case, drug treatment will be ineffective, since it can only eliminate the symptoms, but not cure the disease.
One of the most popular drugs today that helps heal inflamed joints and tendons is Artracam. It has a positive effect on the metabolism in cartilage tissues and also stimulates biosynthesis.
The main active ingredient of Artracam is glucosamine sulfate. It has a pronounced analgesic and anti-inflammatory effect, and also increases the amount of hyaluronic acid in the synovial fluid. Degenerative processes in the joints are slowed down, and joint function is restored. The pain becomes less pronounced even in the acute period.
Aseptic (crepitating) form of the disease
The development of this form of the disease is caused by a lack of synovial fluid, which causes increased friction between the layers of the tendon sheath. An accumulation of serous or hemorrhagic exudate occurs in the capsule cavity. With proper and timely treatment, the exudate is converted into fibrinous, which indicates the beginning of regeneration.
However, clinicians have proven that in most cases, first-time aseptic tenosynovitis, treated incorrectly or insufficiently, develops into a chronic form. This can be explained by the formation of a large number of adhesions inside the capsule and the replacement of cells that form the synovial fluid with connective tissue.
Differential diagnosis
- Intercarpal instability. The wrist is a complex anatomical area consisting of a large number of small bones and ligaments. Degenerative processes or direct trauma can lead to instability between the articulating bones, which in turn leads to pathological changes in the biomechanics of the hand and the appearance of pain. Scapholunate dissociation, scaphotrapeziotrapezial joint degeneration, and lunate-triquetral dissociation can all be associated with radial wrist pain.
- Fracture of the scaphoid bone.
- Most often, a scaphoid fracture occurs as a result of a fall on an outstretched arm with an extended wrist. In this case, pain occurs on the side of the radius, there is also swelling in the area of the anatomical snuffbox, limited range of motion, pain when performing a movement, especially at the end of the amplitude. If the patient has been injured and subsequently experiences pain in the wrist from the side of the radius, then it is first necessary to exclude a fracture of the scaphoid bone.
- Damage to the superficial branches of the radial nerve (Wartenberg syndrome). The superficial branches of the radial nerve innervate the dorsal surface of the first and second fingers and the first interdigital space. Nerve fibers can become compressed between the extensor carpi radialis brevis and brachioradialis tendons due to scar tissue formation after injury or from wearing tight jewelry. As a result of compression, ischemia develops and, as a result, numbness and tingling in the area of innervation.
- Radiculopathy of the cervical spine at the C6 level. Compression of the spinal nerve roots can cause sensory disturbances, muscle weakness, and weakened reflexes. The key dermatomes of the C6 segment are the radius of the second metacarpal and the index finger, which is approximately the same area where pain occurs in de Quervain's syndrome. It is precisely because of the similarity of symptoms that it is important to exclude cervical radiculopathy and carefully check the C6 segment.
- Osteoarthritis of the first metacarpal joint. Osteoarthritis of the first metacarpal joint usually occurs in people over 50 years of age and usually manifests itself as stiffness of the joint in the morning, decreased range of motion, and tenderness in the area. With this disease, the squeeze test will be positive.
- Crossover syndrome. With this syndrome, pain will occur closer to the back of the forearm, mainly in the middle and about 5 cm below the wrist.