What is echinococcosis?
In order to start talking about the symptoms of the disease, and even more so about the prevention and prevention of infection by parasites, it is necessary to clearly understand what we are dealing with.
And so, echinococcosis is a disease caused by parasites from the group of tapeworms. The disease affects parasitic cysts formed in the tissues of internal organs, most often in the liver and lungs.
How does the ecchinococcal parasite enter the body?
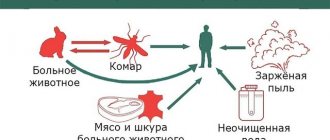
Echinococcosis is a zoonotic disease , as it is transmitted from animal to human, but what path does the parasite take before it enters the human body?
Intermediate carriers of the parasite are herbivores and omnivores that have consumed food and water contaminated with eggs. Next, in the animal’s body, the parasite goes through its larval stage, which takes place in the internal organs.
The definitive host is a carnivore. The parasite lives in the intestines, and the final carrier becomes infected by eating the organs of intermediate animals infected with cysts.
A person acts as a random intermediate carrier . The whole point is that people can become infected with echinococcosis in the same way as intermediate carriers - animals, but cannot transmit the infection to the final carrier.
Symptoms of echinococcosis.
When infected, the human body develops from one to several hydatids. They are most often localized in the liver or lungs; in rare cases, the infection affects other organs and tissues.
A person can be infected with echinococcosis, but not suspect it for many years. All this can continue until clinical signs appear. Moreover, more than half of infected patients receive treatment after a large amount of time has passed from the onset of infection.
The main symptoms of the disease may be pain in the abdomen and its area, nausea and vomiting; these signs are characteristic of liver echinococcosis. In cases of infection of the lung tissue, chest pain, shortness of breath when inhaling, or a chronic cough are noticed.
Why are we considering echinococcosis of the lungs and liver?
The thing is that localization in the liver and lungs accounts for the largest percentage of cases of infection. Below we will look at echinococcosis of the liver and lungs separately and in more detail.
The role of parasites in the structure of morbidity among the population of the Russian Federation has been steadily increasing in recent years. Increasingly, echinococcosis is found in non-endemic foci, where doctors are unfamiliar or have little knowledge of the basic principles of its diagnosis and treatment, which often leads to late detection of the disease and to unfortunate errors in treatment. These facts force us to pay closer attention to the problem of echinococcal invasion. Indeed, in addition to the fact that, as a rule, young able-bodied people, as well as children, suffer, more than 2/3 of patients require surgical treatment. Unfortunately, the frequency of disease relapses remains high, which causes understandable dissatisfaction among surgeons with the results of treatment of this category of patients [2, 4, 8]. In this work, we aimed to discuss the main features of the development of echinococcus and, accordingly, the course of the disease, as well as important points in the surgical and conservative treatment of invasion.
Biology of the parasite
The causative agent of echinococcosis is the tapeworm Echinococcus granulosus
, which parasitizes carnivores. Echinococcosis is a severe parasitic disease and in its development always goes through the stage of cyst formation. Echinococcosis in humans and animals is the same, and an intermediate host is required for the parasite to fully develop.
The intermediate hosts of the parasite are humans and farm animals. Definitive hosts, such as dogs, become infected by eating the entrails of animals with hydatid cysts. The embryonic elements contained in the cyst (protoscolexes and acephalocysts) attach to the wall of the animal’s small intestine and grow into adults. Mature segments containing 400-800 oncospheres are detached from the abdomen of the protoscolex; infected dog feces contaminate the grass and soil; eggs enter the intestines of sheep, pigs, camels or humans, or onto the fur of dogs. A person can become infected by petting a dog or eating contaminated vegetables. It is important to understand that the role of meat products is minimal, since both humans and farm animals are intermediate hosts, and heat treatment of meat almost always leads to the death of the parasite. The possibility of infection through meat plays a role only among persons engaged in slaughtering livestock, cutting meat and skins [2, 4, 8].
The opinion, widespread even among some medical workers, about the possibility of a healthy person becoming infected from a patient is completely wrong. When working with people infected with echinococcosis and those around them, it is worth paying special attention to this kind of explanatory conversations, since such patients are often isolated for some reason. However, when faced with a case of infection of one of the family members with echinococcosis, it always makes sense to examine the rest. This is not due to the fact that they infect each other, but because members of the same family together could eat food that already contained echinococcus eggs.
After the Echinococcus egg (oncosphere) enters the body of the intermediate host, the following occurs. Oncospheres are covered with a membrane that dissolves under the action of gastric juice. The released parasites penetrate the intestinal mucosa and enter the liver through the portal vein system, where they develop into a mature cyst. Most parasites are retained in the hepatic sinusoids, which is why 70% of echinococcal cysts form in the liver. Individual eggs pass through the liver and, bypassing the heart, are retained in the pulmonary capillary bed, which leads to the formation of pulmonary cysts (15-20%). Echinococcal heart disease is also possible, but is observed quite rarely - in less than 0.5% of patients. This is attributed to the high rate of blood flow through the organ. When the parasite enters the systemic circulation, cysts (10-15%) are formed in the spleen, brain and bone marrow, etc. Observations of isolated echinococcosis of the subcutaneous tissue of the legs, ligament of the uterus, eyes, thyroid and pancreas are described as casuistic [1, 3 , 7]. Thus, if echinococcosis is suspected, it is first of all advisable to examine the first target organ, the liver, and then the lungs.
From the echinococcus embryo, a maternal cyst develops over several months, which is a bubble filled with liquid. The wall of an hydatid cyst consists of two membranes: the outer cuticular and the inner germinal (germ). The cuticular and germinal membranes are macroscopically represented by a single capsule, so most often they appear under the single concept of “chitinous membrane”. Externally, the hydatid cyst is surrounded by a dense connective tissue fibrous capsule formed from the tissues of the organ as a result of the protective reaction of the intermediate host against the metabolic products of the parasite [3].
Diagnosis of echinococcosis
In the early period, echinococcosis is practically asymptomatic. In this regard, patients often seek medical help when the parasitic cyst reaches a significant size, squeezing neighboring organs, or due to the cyst breaking into the pleural cavity or bronchi, etc.
Of decisive importance in the diagnosis of early stages, as well as as a confirmatory method in the presence of radiological signs of echinococcosis, are immunological studies - the detection of specific antibodies to echinococcus in the blood using an enzyme-linked immunosorbent assay (ELISA) reaction. A high content of specific antibodies is observed in 95% of patients with an active process: when live parasite cysts are localized in the liver, abdominal cavity and retroperitoneal space, as well as with multiple and combined damage to internal organs. It makes sense to perform not a qualitative, but a quantitative analysis for echinococcosis due to the high frequency of false-positive results in a qualitative analysis.
Eosinophilia occurs in 18-83% of cases; Some authors note a characteristic increase in the number of leukocytes and total blood plasma protein in patients with echinococcosis. The number of blood lymphocytes is usually reduced; the level of all classes of blood immunoglobulins is often elevated. Let us make a reservation that all these changes in blood composition are characteristic of active forms and even multiple organ damage by the parasite. With 1-2 even mature cysts, the peripheral blood picture, as a rule, does not undergo significant changes.
The leading method of radiological diagnosis of echinococcosis of the liver and other organs is ultrasound examination. The method is publicly available and allows you to diagnose echinococcosis at a stage when parasitic cysts are still small in size, starting from 1.5-2 cm.
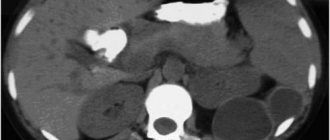
On the sonogram, the hydatid cyst itself is a hypoechoic (anechoic) formation with a double contour. This is the chitinous membrane, which looks like the hyperechoic inner layer of the cyst. Inside it, multiple mobile hyperechoic inclusions like sediment are often identified. These are the germinal elements of Echinococcus, the so-called “hydatid sand”. The fibrous capsule looks like a hyperechoic rim and is separated from the chitinous membrane by a hypoechoic layer - the “lymphatic cleft” (Fig. 1).
Rice. 1. Sonogram of an hydatid cyst of the liver. An anechoic formation with basal enhancement, a hypoechoic rim and a clear two-circuit structure of the wall is determined.
A ribbon hyperechoic structure in the lumen of the cyst (detached chitinous membrane), as well as additional cystic inclusions (daughter cysts), are pathognomonic only for hydatid cysts (Fig. 2).
Rice. 2. Sonogram of an hydatid cyst with a detached chitinous membrane (ribbon hyperechoic structure, indicated by arrows). The diagnosis of echinococcosis is valid even with a combination of two or three of these signs [3].
When the cyst size is up to 30-40 mm, these signs are weakly expressed, which makes differential diagnosis extremely difficult, therefore, for small cysts, in addition to blood ELISA for echinococcosis, it is advisable to perform magnetic resonance imaging (MRI). As a rule, MRI allows one to identify signs characteristic of a parasitic cyst [9].
Treatment
The drug albendazole has been developed for chemotherapy of echinococcal invasion. However, as the only treatment method, albendazole is effective only in the early stages of the disease, until a dense fibrous capsule with a lymphatic gap has formed around the parasitic cyst itself [4]. These structures reliably protect echinococcus from systemic influences. In this regard, the most common treatment method for most patients with echinococcosis is surgery [3, 7].
Three types of interventions have been developed for the surgical treatment of echinococcosis: traditional open, laparoscopic and minimally invasive percutaneous. According to world statistics, minimally invasive interventions are currently used in almost a third of patients with echinococcosis [5, 7, 8]. At the same time, surgeons are more prone to sparing interventions in endemic countries, where the number of patients is significantly larger. In those countries where the disease occurs sporadically, an overly radical approach with a predominance of total pericystectomy or liver resection still dominates.
An attractive, at first glance, technique of laparoscopic removal of echinococcal cysts does not always justify itself. The fact is that various technical devices that prevent hydatid fluid from entering the abdominal cavity, as the cavity subsides, no longer reliably eliminate the risk of contamination. This is associated with a high rate of relapses after surgery. In recent years, the indications for laparoscopic surgery for liver echinococcosis have been revised, and the technical accessibility of the cyst is no longer considered one of the main indications for it. Laparoscopic interventions are advisable if it is technically possible to remove the cyst without opening it, i.e., if it is possible to perform the so-called ideal echinococcectomy. This situation occurs when the cyst is located marginally or extraorganically, which is extremely rare [7, 10].
Percutaneous echinococcectomy is currently the standard of surgical treatment for patients with liver echinococcosis with type I-II cysts according to the Gharbi classification [6]. The technique combines the advantages of low-traumatic access and the possibility of parasite eradication [1, 5, 9]. As experience is gained, contraindications to percutaneous interventions are also reviewed. Our experience shows that traditional contraindications to percutaneous echinococcectomy, such as the location of the cyst superficially, subcapsularly, extrahepatically, close to the main vessels and ducts in the liver tissue or outside it, as well as the presence of a small number of daughter cysts inside the mother one, are very relative. Such features somewhat complicate the operation, but when performed professionally, they do not affect the result [3, 5].
The main and, in fact, the only contraindication to percutaneous echinococcectomy is the release of germinal elements beyond the fibrous capsule - the so-called exogenous budding. With this type of cyst, there is no way to treat the budded fragment with germicide, and this almost always leads to relapse of the disease.
Method of percutaneous echinococcectomy from the liver
In foreign practice, the technique of percutaneous echinococcectomy appears under the abbreviation PAIR - puncture, aspiration, injection, and respiration (puncture, aspiration, injection and respiration). As you might guess, this is a list of the main stages of the operation [5].
Percutaneous intervention for echinococcosis requires very careful adherence to the surgical procedure. The main requirements are the use of a catheter needle for initial entry into the cyst and transhepatic access for carrying out the instrument. During the initial puncture of a living hydatid cyst, the use of the Seldinger technique, i.e., insertion of a catheter along a guide after removing the puncture needle, is absolutely unacceptable. Since the hydatid fluid is under high pressure in the cyst, its outflow with contamination of the cavity during the process of replacing the needle with a catheter is inevitable. For the same reason, transhepatic access to the cyst is necessary, no matter how tempting and safe the puncture trajectory outside the organ may seem. Liver tissue serves as an additional barrier between the cyst and the free abdominal cavity.
So, after puncture of the cyst with a catheter needle under ultrasound control, antiparasitic treatment is performed with an effective germicide. The hydatid fluid is completely removed and sent for parasitological examination to further verify the diagnosis. The remaining cavity in the appropriate volume is filled with germicide along the catheter. One of the most effective intraoperative germicides with a proven antiparasitic effect on Echinococcus granulosus in vitro
and
in vivo
is an 87% aqueous solution of glycerol with an exposure of at least 7 minutes. It is the stage of removing hydatid fluid and antiparasitic treatment that is the most critical in the entire operation and requires scrupulous adherence to the technique. There is a high risk of fluid effusion into the surrounding space with the development in the long term of contamination and relapse or a severe allergic reaction in the patient during surgery, up to and including anaphylaxis. In this regard, it is advisable to prevent anaphylactic reactions by early intraoperative administration of a dose of corticosteroid. Germicide exposure longer than 7 minutes is not justified. Experimental studies on mice have confirmed that exposure to an 87% aqueous solution of glycerol for 6-7 minutes is sufficient for the complete death of protoscolexes.
After complete removal of the germicide, the stage of echinococcectomy proper begins, i.e., removal of all elements of the parasite with a chitinous shell. After treatment with glycerin, i.e., destruction of living protoscolexes, it is already possible to replace the catheter needle with drainage of sufficient diameter (at least 16 Fr) through a guidewire. This allows, with certain experience, to completely remove all elements of the parasite and the chitinous membrane on the first day after surgery. Is it possible to leave the membrane in a cyst that has already been treated with germicide? It is possible, but impractical, because a residual cavity is almost always preserved, the risk of suppuration of which is reliably almost 2 times higher when the membrane is left. After removing the maximum possible volume of the chitinous membrane, the drainage from the cyst can be removed and the echinococcectomy can be considered complete.
After percutaneous echinococcectomy, the surgeon is faced with the question of the residual cavity after surgery. There is no clear solution to this problem yet. We have empirically established that in children the residual cavity almost always closes on its own within the first year after surgery. In adults, reduction in cavity volume occurs less frequently. At the same time, attempts at repeated interventions for the purpose of additional sclerosis of the cavity only aggravate the situation.
Experience shows that a residual cavity requires watchful waiting and dynamic monitoring. The longer the observation period, the smaller the number of patients with residual cavity. At the same time, the more often repeated interventions are performed, the more rigid and resistant to influence the cyst walls become. In principle, it is obvious that the existence of a small residual cavity, about 4-5 cm, does not have a significant effect on either the function of the liver or the body as a whole. There is no developed international algorithm for residual cavities yet. Based on our own experience, we came to the conclusion that for clinically significant residual cavities, microwave ablation is more effective than repeated percutaneous drainage and sclerotherapy.
It is worth touching on traditional open methods of treating liver echinococcosis. With the accumulation of experience, clear indications for performing laparotomy for echinococcosis have emerged. Today, the need for major traumatic surgery is often caused by contamination of the abdominal cavity in case of non-compliance with the rules of anti- and aparasiticity during previous laparoscopic or percutaneous intervention [7, 9].
The general desire to minimize the traumatic nature of the operation also affected traditional surgical treatment for liver echinococcosis. It has been proven that a simple echinococcectomy, consisting of opening and antiparasitic treatment of the cyst, followed by removal of the membranes and, if necessary, capitonnage of the residual cavity, gives equally satisfactory long-term results in relation to relapse of the disease, as do total pericystectomy or liver resection, i.e. complete removal of the cyst even together with the fibrous capsule [7].
Despite the improvement of intervention techniques, adherence to the principles of anti- and aparasitic surgical intervention, the introduction of various chemical and physical methods of influencing the parasite, the use of advanced instruments, the frequency of relapses of the disease remains high and reaches 5-33% [8, 10], so the enormous impact The results of treatment are influenced by subsequent chemotherapy or anthelmintic therapy. It is also necessary to influence small-sized screenings of echinococcus, which are inaccessible to modern diagnostic methods. Several multicenter studies, in which our clinic participated, have proven that a course of specific antiparasitic drugs is strictly necessary to prevent relapse of the disease even after a perfectly performed operation [7-9].
The most effective and generally accepted drugs affecting hydatid echinococcus are albendazole and its analogues [4, 9]. It is unfortunate that surgeons are not very willing to recommend postoperative drug treatment to patients. The prevailing point of view about the extreme toxicity of the drug is not true. Moreover, chemotherapy is also justified as an independent method of treatment for cysts up to 3 cm in size or less, especially for pulmonary echinococcosis. We emphasize, however, that for large cysts, mandatory surgical treatment of one kind or another is indicated, since the use of albendazole alone in this case is ineffective.
Thus, scientific achievements in recent years have radically changed approaches to diagnosis and choice of treatment methods for patients with echinococcosis. New aspects of the morphology of the parasite have shown that the result of the use of modern highly informative instrumental research methods is not just a statement of the fact of the presence of a cyst, but also an indication in the research protocol of its characteristics, size, nature of the contents, shape, description of the shape of daughter cysts, mention of the presence of exo- and endogenous budding cysts, the degree of their penetration into the fibrous capsule. Ultrasound and MRI are considered the most effective in this regard. Detection of cystic formations almost always requires serological tests for echinococcosis. Patients with echinococcosis, regardless of the size and location of the cysts, are not subject to dynamic observation and should be sent to a surgical hospital with experience in treating such patients. An integrated approach is mandatory, including the use of postoperative anthelmintic therapy. All patients with hydatid cysts larger than 3 cm are subject to surgical treatment. The choice of intervention technique is determined depending on the technical capabilities of the hospital and the characteristics of the cyst itself.
The authors declare no conflict of interest.
Liver echinococcosis.
This type of infection accounts for from fifty to seventy percent of all cases of echinococcosis. The parasite larvae travel through the bloodstream from the intestinal walls to the liver, where most of them settle on small capillaries. Over time, the cysts slowly but progress, thereby breaking into the internal environment of the liver.
The earliest symptoms of liver echinococcosis include:
- Heaviness and pain in the epigastric region
- Heaviness and pain in the right hypochondrium
This is due to the development of a cyst in the right lobe of the liver.
Relevance of the problems of echinococcosis and alveococcosis
The relevance of the problems of echinococcosis and alveococcosis is associated with their wide prevalence, the variety of negative effects on the human body and the pronounced polymorphism of clinical manifestations. According to the Federal Service for Surveillance on Consumer Rights Protection and Human Welfare, the incidence of echinococcosis in the Russian Federation in 2008 increased by 5.4% compared to the previous year. A total of 551 cases of hydatid and alveolar echinococcosis (0.39 per 100 thousand population) were registered in 63 constituent entities of the Russian Federation versus 527 cases (0.37 per 100 thousand population) in 2007 in 56 constituent entities of the Russian Federation. Among children under 14 years of age, 71 cases of echinococcosis were registered (0.34 per 100 thousand), in 2007 - 49 cases (0.23 per 100 thousand children). The share of urban residents in the last two years has been 48% of the total number of diseases.
On the territory of the Russian Federation, deaths from echinococcosis are systematically recorded. During the period from 1996 to 2008, 109 deaths were registered, the largest number of which occurred in the Krasnoyarsk Territory (21.1%) and the Orenburg Region (19.2%). According to form No. 5 vet. “Information on the veterinary and sanitary examination of raw materials and products of animal origin for 2008” identified 72,371 samples of meat with echinococcal blisters in the markets in 46 constituent entities of the Russian Federation. The percentage of contamination of cattle meat was 2.31%, sheep - 3.5%, pigs - 1.17%.
An analysis of hospitalization of patients with echinococcosis and alveococcosis at the Regional Oncology Dispensary named after. A.I. Krizhanovsky" from 2004 to 2008.
During this period, 47 primary patients with this pathology were treated. Of these, the majority are women (54%).
The largest number of cases were registered in the cities of Krasnoyarsk, Lesosibirsk, Yeniseisk, Sharypovo, Uzhur and other cities of the Krasnoyarsk Territory. The incidence of echinococcosis exceeds that of alveococcosis (60% and 40%, respectively).
Surgical treatment was performed in 52% of patients with a favorable outcome (remission) and inoperable cases in 46%, one death. Patients are observed by an infectious disease specialist at the KKB or at their place of residence for the purpose of anti-relapse therapy with Albendazole.
Up
Pulmonary echinococcosis.
The development of pulmonary echinococcosis is less common than infection in the liver and accounts for twenty to thirty percent of all cases of infection. Once the infection enters the lung tissue, the disease begins to progress.
As it grows, it can cause:
- Chest pain
- Cough (from a dry cough to a wet cough with the presence of blood)
- Manifestation of shortness of breath
- In cases of the development of a particularly large cyst, deformations of the chest are noticed
1.General information
Echinococcus is one of the most dangerous parasites, the larva of which can be transmitted to humans from infected animals (mainly canines), with water, unwashed berries, etc. At a certain stage of development, echinococci form spherical cysts with a diameter of 1-5 to 20 cm (or more) in vital organs: liver, lungs, kidneys, brain, etc. Most often, echinococcosis is registered in livestock-raising regions, where the most favorable conditions for the spread of the helminth exist, but in the era of total migrations and travel, you can become infected, essentially, anywhere.
The lungs are affected in approximately 15% of all cases of echinococcal invasion, and this is the second most common site of occurrence (after the liver) of the main focus. The severity of pulmonary echinococcosis is due to the objective difficulties of diagnosis, the abundance of complications and the obvious danger of the very localization of cysts in the respiratory system.
A must read! Help with hospitalization and treatment!
Treatment of echinococcosis at the EUGINE clinic.
Our clinic specializes in the treatment of echinococcosis of the lungs, liver and other organs or tissues. Thanks to the technique developed by Evgeniy Lee, director and innovator of our clinic. A specially developed drug treatment method allows you to get rid of echinococcosis and formed cysts once and for all without surgical or chemotherapy intervention.
Also, our specialists are always happy to help you and diagnose your body, which will allow you to clearly look at the problem and immediately begin effective treatment. You can make an appointment with us in two ways. The first is to call us at the number listed on the website. The second is to leave a request by filling out the form on the right. Our operators are always ready to help and advise you on any questions you may have.
Take care of your body and prevent possible parasitic diseases in time, and the EUGINE clinic will become your indispensable assistant in this!
4.Treatment
Despite reports of successful courses of chemotherapy for fairly small cysts, conservative therapy for pulmonary echinococcosis is generally ineffective. Currently, only surgical treatment is possible. Several different techniques have been developed and are successfully used (echinococcectomy, pericystectomy, in rare cases and strictly according to indications - lung resection). As a preferred choice, if the clinical situation allows, the so-called. ideal enucleation of the cyst, i.e. removal of the echinococcal capsule without destroying its shell. Surgery is usually performed with intensive drug support.
Methods for preventing echinococcosis are quite obvious: identifying and eliminating possible foci of infection, strict control of the sanitary condition of livestock farms, systematic destruction of stray animals, especially dogs. Recommendations for regular deworming (as well as reducing the number) of service dogs have been developed and published for implementation. The main measures of individual prevention are the avoidance of drinking unboiled water and unwashed berries, and mandatory hand hygiene after any contact with dogs and any other animals (this especially applies to children).