28.06.2017
Diseases of the chest and abdominal cavity | Liver and pancreas
The starting point for the departure of bile is the place of its formation - liver cells. The final point is the duodenum, where bile carries out its main work. Between them are transport routes of varying lengths and calibers, passing both inside and outside the liver. They are called bile ducts or vessels. In ancient Greek, “χολή” means bile and “ἀγγεῖον” means vessel. Hence the accepted name for their inflammation - cholangitis.
Causes and types
Cholangitis occurs due to obstruction of the bile ducts and associated infection. The patency of the ducts can be difficult due to the formation of stones, scarring, removal of the gallbladder, cysts, various parasites, etc.
Infection usually occurs in two ways:
- ascending route (from the intestine);
- descending path (through blood and lymph).
- There are acute and chronic cholangitis.
In this case, acute cholangitis occurs:
- catarrhal (with the occurrence of swelling of the mucous membrane of the bile ducts);
- purulent (pus forms and spreads to neighboring organs);
- diphtheritic (necrosis occurs during inflammation);
- necrotic (occurs due to the entry of enzymes into the pancreas, destroying the mucous membrane);
- The chronic form can be latent, recurrent, septic, abscessing, sclerosing.
4. Treatment of cholangitis
Treatment for cholangitis is surgical. First, the cause of bile stagnation is eliminated and its outflow is restored. The operation is usually performed laparoscopically.
After this, it is necessary to remove the intoxication. If cholangitis is caused by bacteria or parasites, then antibiotics or antiparasitic drugs are prescribed.
For primary sclerosing cholangitis, treatment consists of taking ursodeoxycholic acid drugs.
To ensure that cholangitis does not have to be treated at all, prevention is recommended. First of all, timely treatment of pancreatitis, cholecystitis and cholelithiasis is necessary.
Symptoms
Symptoms of acute cholangitis:
- fever;
- chills;
- increased sweating;
- intense pain in the hypochondrium on the right;
- nausea, vomiting;
- change in skin color and whites of the eyes (they become yellow);
- skin itching.
The chronic form rarely has pronounced symptoms, but the following manifestations are possible:
- periodic fever;
- itching;
- increased fatigue;
- enlargement of the phalanges of the fingers;
- redness of the palms.
2. Symptoms of the disease
Cholangitis is characterized by a sudden onset. The patient may quickly develop the following symptoms of cholangitis:
- A sharp increase in body temperature, accompanied by chills;
- Spasmodic pain in the right side of the abdomen;
- A sharp drop in blood pressure;
- Nausea and vomiting;
- Weakness.
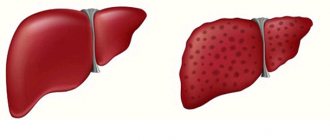
In addition, with cholangitis, liver failure develops, which is characterized by impaired consciousness, skin itching and jaundice.
Visit our Hepatology page
Treatment
Treatment of cholangitis is possible with both medications and surgery.
Treatment of acute cholangitis is carried out only in a hospital setting due to the risk of complications in the form of spread of infection to other organs.
For conservative treatment, the following is prescribed:
- antibacterial drugs;
- means to combat intoxication;
- drugs aimed at the outflow of bile;
If drug therapy does not produce results, then surgical intervention is indicated. In most cases, the endoscopic technique is used, because it is the least invasive. During the operation, the surgeon can drain the ducts, remove stones, and eliminate narrowing.
In case of extensive lesions, the patient needs strip surgery, during which the destroyed areas are removed.
3.Diagnosis of the disease
First of all, the doctor will examine you and record your symptoms. To accurately diagnose cholangitis, the following methods of examining internal organs can be used:
- Duodenal intubation with bile examination is also performed. This is done to determine the causative agent of cholangitis;
- Ultrasound of the abdominal cavity. Ultrasound helps assess the size of the liver and bile ducts;
- ERCP (endoscopic retrograde cholangiopancreatography). ERCP allows you to examine the bile ducts X-ray using contrast;
- MRI and CT can complement the results of ERCP.
The following tests are also performed to diagnose cholangitis:
- Complete blood count (CBC). With the help of OAC, inflammatory processes in the body are detected;
- Biochemical blood test (BAC). During the test, the indicators of ALT (alanine aminotransferase), AST (aspartate aminotransferase) and GGT (hamaglutamyl transpeptidase) are measured;
- General urine test for bile pigments;
- Stool analysis for parasites.
About our clinic Chistye Prudy metro station Medintercom page!
Causes of cholangitis
Bile stagnation is often the main predisposing factor. The trigger is infection (mainly bacterial). Stagnation becomes a consequence of blockage of the bile ducts with stones, compression by a tumor, cicatricial changes in the walls of blood vessels, dyskinesia, stenosis of the papilla of Vater, inflammatory processes in nearby organs, etc. Less commonly, helminths, autoimmune reactions, and entry into the ducts of pancreatic secretions act as a causative factor for inflammation of the bile ducts .
Cholangitis rarely acts as an independent pathology. More often it accompanies and/or is accompanied by disorders of other organs of the gastrointestinal tract.
Primary sclerosing cholangitis
Treatment of patients with PSC is carried out in three directions.
Reducing the effects of chronic cholestasis . For this purpose, it is recommended to limit the consumption of neutral fats (up to 40 g/day), calcium intake (up to 6 g/day), and fat-soluble vitamins A, D, E, K. For symptomatic vitamin deficiencies, parenteral administration of vitamins A, D2, K is necessary (monthly ). To relieve skin itching, the most painful symptom in some patients, ursodeoxycholic acid 10-15 mg/(kg day) 1, phenobarbital (0.1-0.3 g/day), rifampicin (0.15-0.45 g/day) are used. day), hylestyramine (4-16 g/day).
Treatment of specific complications. The development of bacterial cholangitis requires treatment with antibiotics, taking into account the most frequently detected microorganisms in bile (enterobacteria, enterococci, bacteroides, clostridia). The drugs of choice for parenteral administration are ampicillin or mezlocillin or clindamycin in combination with gentamicin, 3rd generation cephalosporins of the cefatoxime group, although the latter have no effect on enterococcus. To effectively treat anaerobic infection, metronidazole is added to these drugs. For patients with mild cholangitis, antibacterial drugs (ampicillin, ciprofloxacin, biseptol) are prescribed orally. Antibiotics are sometimes used long-term to prevent recurrence of suppurative cholangitis, but there are no studies confirming the effectiveness of this approach. Severe bile duct strictures are dilated using a balloon dilator inserted endoscopically or percutaneously; if ineffective, an endoprosthesis is installed. A brush biopsy from the sites of greatest narrowing is necessary to exclude cholangiocarcinoma, but cytological studies are insufficiently effective. The formation of cholesterol and pigment stones, localized mainly in the gallbladder, is observed in more than a quarter of patients. When blocking the bile ducts with a stone, the possibility of endoscopic removal of the stone from the extrahepatic ducts with ERCP with sphincterotopy, and from the intrahepatic ducts - with percutaneous transhepatic cholangiography, should be discussed. If it is impossible to remove the stone, surgical treatment is indicated. Cholangiocarcinoma develops in 10-15% of patients, more often in the terminal stage of PSC (similar to the development of colon cancer in UC), and is one of the main causes of death in patients. Chemotherapy and radiation therapy are ineffective; tumor resection is possible; an alternative to resection is a liver transplant.
Treatment aimed at slowing the progression of the disease is surgical. The effectiveness of reconstructive operations on the bile ducts with the creation of bile drainage (internal with the application of an enterostomy or external) is assessed ambiguously, however, given the frequent occurrence of purulent recurrent cholangitis and the development of complications during liver transplantation in the future, surgical interventions on the bile ducts should be avoided whenever possible. Proctocolectomy in patients with UC is ineffective and is not used as a method of treatment and prevention of PSC progression.
Drug treatment . Three drugs with different mechanisms of action have been evaluated in controlled trials: Dpenicillamine, cyclosporine, ursodeoxycholic acid. In addition, separate uncontrolled studies have assessed the effectiveness of colchicine and immunosuppressants (glucocorticosteroids). None of these drugs appears to have much effect on the progression of the disease, especially if treatment is started at the stage of cirrhosis. D-penicillamine is ineffective for PSC. The use of other drugs in the early stage of the disease may be accompanied by an improvement in the clinical and laboratory course. The administration of ursodeoxycholic acid (10-15 mg/(kg/day) leads to a decrease in skin itching, a decrease in laboratory parameters of cholestasis, cytolysis, but this effect disappears after stopping the drug. The use of glucocorticosteroids and their combination with colchicine has a positive effect in patients with severe immune reactions and a significant increase in aminotransferase activity, however, these data are not confirmed in other studies. The use of cyclosporine C did not give the expected results. In isolated reports regarding treatment with azathioprine and methotrexate, the effectiveness of azathioprine was not confirmed; with treatment with methotrexate, impressive results of improvement were obtained only biochemical parameters, but also the histological picture at the early stage of PSC, which requires further evaluation of the drug in controlled studies, given its hepatotoxicity.
An effective method of treating PSC is liver transplantation, which is undoubtedly indicated for patients with established liver cirrhosis and the development of hepatic cell failure, portal hypertension and at least one of the complications: bleeding from varices of the esophagus or stomach, resistant ascites, recurrent bacterial peritonitis, portosystemic encephalopathy, as well as recurrent purulent cholangitis. However, the progressive course of the disease in most patients, the possibility of developing cholangiocarcinoma, as well as good long-term results of transplantation suggest the possibility of liver transplantation even before the terminal stage of the disease. PSC, along with PBC and biliary atresia, is one of the main indications for liver transplantation. After liver transplantation, one- and two-year survival rates are 89 and 83%, respectively, and follow-up periods reach 10 years or more.
Forecast:
In 70% of patients, progression of PSC with the development of liver cirrhosis is observed, regardless of the presence or absence of symptoms of liver failure in chronic patients. Reverse development is extremely rare. The main prognostic
Factors include serum bilirubin level, patient age, histological stage of liver disease, and the presence of splenomegaly. The duration of the disease from the moment of diagnosis ranges from 10 months to 29 years, the average survival rate is about 12 years.
Thus, PSC is an increasingly recognized liver disease, which is one of the causes of chronic cholestasis with outcome in biliary cirrhosis and the possible development of cholangiocarcinoma. The importance of studying the disease is due to its significantly greater prevalence than previously estimated, the incidence of predominantly young people, and the lack of development of effective drug therapy. PSC should be suspected in a patient with ulcerative colitis or Crohn's disease with increased blood alkaline phosphatase activity. ERCP is the main diagnostic method. Liver biopsy findings are of additional importance. Liver transplantation is recognized as the only effective treatment method. Clarification of the etiology and pathogenesis of progressive bile duct sclerosis will make it possible to change the prognosis of the disease, which remains serious in most patients.