TODAY NO PEOPLE DIE FROM AIDS IF
are observed by a doctor, start treatment on time and do not make mistakes in treatment.
Until recently, AIDS was a deadly disease. It was called the "plague of the 20th century." AIDS equaled death. Since 2006 the situation has changed. Now people are not dying with HIV diagnosis. True, they live their whole lives taking medications (antiretroviral drugs) strictly according to the clock, going to the doctor without fail, getting tested, and monitoring their health status. Thanks to antiretroviral drugs, HIV infection has turned from a fatal disease into a chronic one. If HIV infection is detected in time and taken under control, then a person’s life is practically out of danger. If all rules for taking antiretroviral drugs are followed, a healthy child is born to an HIV-infected mother in 99% of cases.
The Sverdlovsk region has a high level of HIV infection. Every day, 25 new cases of HIV infection are detected, in 15 of them the infection occurred more than 10 years ago. The virus is actively transmitted through sexual contact. But the main route of transmission remains parenteral (during injection drug use).
In such conditions, life changes. What to do? How to avoid getting infected with HIV? The main thing is to avoid risky contacts.
Risky contact
is any sexual contact without a condom .
Even if you have a regular partner whose HIV status is unknown, a condom is necessary. After all, everyone could have risky contacts. How to avoid getting HIV from your partner?
What if you decide to start a family? Have children? In this case, there is a civilized way: get examined, get tested, including for HIV.
The virus does not manifest itself for many years. A person may not know that he has HIV and pass it on to his partners.
For years the disease is asymptomatic, during this period the person feels absolutely healthy.
Currently, there are drugs that inhibit the development of HIV in the body. Their use makes it possible to maintain the immune system at an indefinite level for a long time, but there is no cure yet for a complete cure, so HIV infection is a chronic and serious disease.
In the context of the rapid spread of HIV infection, it is important:
– know everything about HIV/AIDS
– know your HIV status – give up drugs – use a condom when having sexual intercourse with a partner whose HIV status is unknown.
Diagnosis and treatment of HIV are free and carried out at state expense.
What can be done to prevent HIV from developing into AIDS?
If a person is diagnosed with HIV infection, he needs to start antiretroviral therapy (ART) as soon as possible, which will suppress the replication of the virus. Those registered with the territorial Center for the Prevention and Control of AIDS are given the medicine free of charge. A doctor should select a treatment regimen and help you register. A person taking the medicine will never get AIDS and will be able to live a normal life, says the US Centers for Disease Control and Prevention (CDC) in a leaflet about HIV. However, the drug will not be able to completely cleanse the body of infection, so you will have to take it for the rest of your life.
– The goal of therapy is to achieve an undetectable viral load. This means that the virus is completely suppressed, but its inactive forms live in cells,” says Nikolai Lunchenkov, an infectious disease specialist at the H-Clinic University Clinic.
Am I required to disclose information about my diagnosis?
One reason to tell your sexual partners that you have HIV is to protect them from contracting the virus. If you use a condom or your viral load is below detectable levels and your partner is using PrEP, this precaution may seem unnecessary. It may also not be of much importance from a health or interpersonal perspective. However, there is also a legal reason why disclosing this information may be very important. In many states (***as well as in Russia) there are laws requiring information about one’s HIV status, and in some states this obligation applies regardless of whether the partner became HIV-positive as a result of contact or not. You need to be aware of the laws in your state to avoid breaking the law.
Can HIV be asymptomatic?
According to
WHO, approximately 21% of HIV-infected people do not know that they are infected and continue to infect others.
Based on the official statistics
on the number of infected people - 38 million people in 2021 - it turns out that about 7-8 million people around the world unknowingly carry the immunodeficiency virus.
The first symptoms appear within 2–4 weeks after infection and are similar to the flu or a cold: enlarged lymph nodes, sore throat, aching muscles, fever, and occasionally mouth ulcers appear. However, some people may have no symptoms at all. Then the immune system begins to actively produce antibodies and launch other protective mechanisms that slow down the rapid reproduction of the virus, and the condition described above passes. The person begins to feel better and lives a normal life for several years, not suspecting anything. This period can last 10 years or longer, but under the onslaught of the virus, the immune system sooner or later gives in and AIDS begins.
Weak immunity of the receiving partner during oral sex
Modern medicine has learned to treat many diseases.
But some of them require the use of a number of drugs that reduce immunity.
For example, hormones and cytostatics for systemic diseases (arthritis, systemic lupus erythematosus, etc.) or after organ transplantation.
In addition to many positive aspects, such drugs have one very negative one - a decrease in immune activity.
As a result, saliva cannot cope with even the smallest amount of HIV and infection occurs.
The progression of infection in such people is also noticeably faster.
The first signs of AIDS appear already one or two years after infection.
How to get tested for HIV?
– There are several types of testing, but the simplest is a rapid test. It detects the presence of antibodies to HIV infection in saliva in a few minutes,” explains Nikolai Lunchenkov. – There is a huge amount of antibodies in saliva, and to HIV (if it is in the body) too. Antibodies are proteins secreted by immune cells to neutralize pathogens and viruses.
One line means a negative result, that is, the absence of antibodies (and therefore HIV). However, you need to keep in mind that in the first month after infection, the result may be false negative due to the fact that antibodies have not yet developed. The presence of two strips does not guarantee that there are definitely antibodies to HIV, but this is a good reason to be rechecked at a specialized center by taking a blood test. There are two types of analysis: by detecting antibodies or through PCR (allows you to detect the RNA of the virus).
– It is worth remembering about the so-called “window period”, when the infection occurred recently and antibodies have not yet been developed (they appear approximately four weeks after infection). In this case, a test for determining antibodies is useless; it is better to use the PCR diagnostic method, says Nikolai Lunchenkov. – But it will take about a day. When a patient consults a doctor for post-exposure prophylaxis, he is immediately tested for HIV, but only to rule out that the person was not infected long before unprotected contact. This is important because the tactics for treating chronic HIV infection and preventing it are different.
Sores in the mouth
Sometimes host partners do not take into account such an obvious risk factor as open wound surfaces.
They are usually associated with recent oral and ENT interventions and irritant phenomena:
- dental procedures – tooth extraction, gum dissection
- periodontal disease - in the acute stage or even at the treatment stage
- piercing, which is now so popular among young people
- ENT surgeries , for example - removal of tonsils (tonsillectomy)
- cocaine use , smoking and vaping
There are also more rare variants, for example - a tumor, tuberculous rashes.
Even when there is no blood in the saliva, you should not consider yourself safe when providing oral sex to an HIV-positive man or woman.
Until the doctor says that all the damage has healed successfully.
Regardless of what caused them.
Is it true that a condom does not protect completely?
So far, the only thing more reliable than a condom in preventing STIs is the absence of any sexual contact. WHO calls
male condoms are approximately 80–85% effective. Gaps in effectiveness are mainly due to improper storage and use of products No. 2.
– It is worth understanding that 80% is average data from the entire planet. The statistics are mainly worsened by third world countries, where used condoms are washed, dried and reused, says Nikolai Lunchenkov.
From time to time you can hear that latex and other materials allow viruses to pass through, but an infectious disease specialist calls this a myth and urges not to believe in it. The Fact Sheet for Public Health Personnel from the US Centers for Disease Control and Prevention (CDC) states that latex condoms provide an impenetrable barrier to particles the size of STIs.
After all, most condoms are coated with a lubricant that can fill hypothetical micropores.
Previously, Roskachestvo examined the quality of condoms. See the results HERE
.
Can I have children?
Yes. Medicines can reduce the risk of mother-to-child transmission of HIV during pregnancy and childbirth to less than one percent. Before fertilization, the sperm of an HIV-positive donor must be cleared of the virus. The main difference will be that you will need a specialist in HIV, fertilization and childbirth. Recently, doctors have been recommending PrEP to prevent partner infection in couples who are trying to conceive. If you want to adopt a child or obtain guardianship, there are protective measures for HIV-positive parents so that your interests will not be infringed.
How to properly store and use condoms?
There are many nuances that the UK National Health Service (NHS) writes about.
Condoms should be stored in a place that is not too warm and not too cold. That is, keeping them in a car that sits in the cold at night is just as undesirable as carrying them in a trouser pocket. The optimal temperature is room temperature. Of course, products should be kept away from sharp objects that could puncture the packaging. Leaving the bag dangling loosely in a backpack or bag is a bad idea, because it can be damaged unnoticed by a collision with a bunch of keys and other things.
Before use, it is important to carefully open the package without using your teeth. When putting on a condom, press down on the accumulator to squeeze out the air from it. Gently roll the product to the base of the penis.
You should not use the same condom more than once - no matter how obvious it may sound. It was mentioned above that in some countries, repeated use is considered normal, which makes the spread of HIV in such areas particularly difficult to contain.
There is no need to put one on top of the other: contrary to expectations, the protection will be less reliable - condoms are more likely to break.
Oil-based lubricants should not be used with latex and polyisoprene condoms, as the products may break. The same can be said about any oil and Vaseline. If a woman uses vaginal suppositories (for example, for treatment), this also increases the risk of rupture. In this case, it is better to use polyurethane condoms, they are invulnerable to fat.
Barrier methods
HIV viruses do not pass through the pores of quality latex.
And now there are not only male, but also female condoms.
When the genitals or oral cavity do not even come into contact with each other, this is the best way to prevent HIV and other STIs.
When used correctly, oral sex becomes 100% safe.
Low-quality products and aggressive sex, when the latex of a condom can be damaged by the actions of a partner, can weaken the effectiveness of protection.
Now there are already developments in the use of special polymer sprays.
They create a film on the genitals impenetrable to microorganisms with complete preservation of sensory sensations.
What protects against HIV transmission besides condoms?
There is so-called pre-exposure and post-exposure prophylaxis for HIV. In the first case, the medicine should be taken regularly by those who have an increased risk of becoming infected: for example, those who have unprotected sex with an untested partner(s). In the second case, medications are needed for those who have already had unprotected sexual contact, especially if it was with a person at risk. Or if the blood of such a person gets into an open wound.
The active ingredients of the drugs block one of the enzymes of the virus that promotes its reproduction. WHO writes
that if you start taking the medicine as soon as possible after contact with the patient (ideally within the first 72 hours), the risk of contracting HIV is reduced by more than 80%.
– Medicines can be bought at some pharmacies in almost any city. The cost of the original drug varies in the range of 9–15 thousand rubles, but there are also budget analogues, says Nikolai Lunchenkov. - In any case, you will first have to discuss the pill regimen with your doctor, and it is important to contact him as early as possible. If you can’t quickly get to a specialist, try contacting representatives of various charitable foundations, and especially organizations fighting AIDS. Perhaps they will help you find the right doctor, and somewhere they will share medications for the first day.
Concomitant sexually transmitted infections
In modern conditions, HIV (especially at the stage of asymptomatic carriage) often coexists with other pathogenic microorganisms.
In sufficient quantities for infection, pathogens are contained in vaginal discharge and in droplets of prostatic secretion, which serves as a male analogue of lubricant.
Pathogenic microorganisms, such as Trichomonas, gonococci, Treponema pallidum, or herpes virus, greatly reduce the protective properties of saliva.
Plus - they violate the integrity of the mucous membrane of the oral cavity and ENT organs.
This weakening of viral defenses greatly facilitates the invasion of HIV into the capillaries.
And syphilis and herpes generally create open gates in the form of ulcers and chancre.
Where does the AIDS virus live?
The virus is found in small quantities in urine, feces, and tears. Once they enter the body of healthy people, infection is impossible. HIV is found in elevated concentrations in such biomaterials as:
- blood;
- sperm;
- vaginal secretion;
- human milk;
- spinal substance.
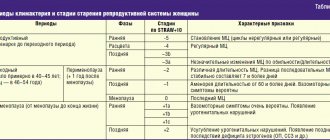
If the above biofluids penetrate the bloodstream, AIDS occurs. Table. Concentration of immunodeficiency virus in biological fluids
| Biological fluid | In dangerous concentration | In a non-hazardous concentration |
| Lymph | + | |
| Blood | + | |
| Saliva | + | |
| Tears | + | |
| Breast milk | + | |
| Genital tract discharge | + | |
| Sputum | + | |
| Urine | + | |
| Sperm | + | |
| Sweat | + | |
| Cerebrospinal fluid | + |





![Table 2. Hemodynamic definition of PH (adapted from [2] with modifications)](https://ms-pi.ru/wp-content/uploads/tablica-2-gemodinamicheskoe-opredelenie-lg-adaptirovano-iz-2-s-izmeneniyami-330x140.jpg)


