Oophoritis is an inflammation in the ovaries that leads to damage to the genitourinary system of a girl/woman. Has a danger to the reproductive system.
An inflammatory process in the ovary can cause inflammation in the fallopian tubes. The disease appears both in one ovary (then unilateral oophoritis is diagnosed) and in two at once, which is called bilateral oophoritis. If inflammation develops in both the ovaries and the uterine appendages, they speak of adnexitis or salpingoophoritis.
- Causes and pathogens
- Symptoms of oophoritis
- Acute oophoritis
- Subacute oophoritis
- Chronic oophoritis
- Exacerbation of chronic oophoritis
- Left-sided oophoritis
- Right-sided oophoritis
- Bilateral oophoritis
- Salpingitis and oophoritis
- Oophoritis during pregnancy
- Diagnostics
- Treatment
- Prevention of oophoritis
Causes and pathogens
The disease can be caused by the following pathologies:
- chlamydia
- gonorrhea
- t richomoniasis
- tuberculosis
- staphylococci (rare)
- streptococci
- Candida
- coli
The development of the disease is influenced by the following factors:
- menstrual cycle
- hypothermia
- surgical manipulation of the genitals
- abortions
- installation of an intrauterine device
In most cases, ovarian inflammation is a secondary process. This means that the infection first develops in the fallopian tubes, uterus or cervical canal, and then moves upward. In rare cases, pathogens of oophoritis penetrate the gonads through lymph and blood.
If the disease is not treated, the infection spreads to the fallopian tubes, causing them to thicken. Pathological changes in the ovaries negatively affect periadnexitis, and the accumulated inflammatory exudate causes the accumulation of pus and forms pyovar. The infection may subsequently extend beyond the ovary and be accompanied by pelpioperitonitis. Oophoritis can also be caused by appendicitis, from which the infection spreads to the ovaries.
Oophoritis develops actively if the following factors are present:
- endocrine system diseases
- infections in the body that develop chronically
- stressful situations and overwork
- diseases of the genitourinary system
- lack of a regular sexual partner
- unprotected sexual intercourse
- smoking
- promiscuity
Consequences and complications
Among the complications of this disease it is worth highlighting:
- Hormonal imbalance. The most common luteal phase deficiency is progesterone and shortening of the luteal phase.
- Transition to chronic oophoritis, the complication of which is progesterone deficiency and chronic anovulation, which is accompanied by anovulatory uterine bleeding and the risk of ovarian malignancies.
- Miscarriage.
- Chronic pelvic pain.
- Purulent-inflammatory formations (tubo-ovarian tumor, ovarian abscesses, pyosalpings). Inflammatory tubo-ovarian "tumor" presents as enlarged and painful appendages that resemble a tumor. The spread of infection goes from bottom to top: endometritis (after abortion, intrauterine interventions, from intrauterine devices) - purulent salpingitis - oophoritis. Ovarian abscesses (pyovarium) are formed from cystic formations; often microabscesses merge with each other, forming a single abscess.
- Pelvioperitonitis (inflammation of the pelvic peritoneum) when the infection enters the peritoneal cavity through the tubes. According to the nature of the inflammation, the process can be serous-fibrous and purulent. The latter is very difficult and is characterized by the appearance of pus in the pouch of Douglas (the depression of the peritoneum between the rectum and the uterus) with the formation of abscesses.
- Ectopic pregnancy.
- Tubal infertility.
Symptoms of oophoritis
Manifestations may vary depending on the stage of the pathological process. The stage can be identified by palpation and ultrasound, which makes it possible to determine swelling, tissue changes and soreness of the ovaries. The pathology can have an acute, subacute and chronic course, depending on which the symptoms differ.
Acute oophoritis is manifested by a number of such signs:
- disruption of the gastrointestinal tract
- general weakness
- high temperature, chills
- painful urination
- headaches and muscle pain
- uterine bleeding
- purulent vaginal discharge
- sharp pain during intercourse
- intense pain in the lower abdomen
In the acute form of the disease, the ovaries are very enlarged due to the inflammatory process and swelling, and pain appears on palpation. The patient must be hospitalized and treated in a hospital.
The chronic form of oophoritis is characterized by the following symptoms:
- pain in the lower abdomen during intercourse
- menstrual irregularities
- dull and aching pain in the groin area and vagina, which becomes stronger during menstruation and with the development of pathologies of various natures
- systematic “awakening” of the disease after remission due to cooling of the body, fatigue and infection in the body
- unproductive attempts to conceive a child
- leucorrhoea (constant scanty discharge)
Chronic oophoritis occurs if the acute form of the disease is not treated. The pathology is most often diagnosed when trying to understand the reason for the inability to conceive or when visiting a doctor with menstrual irregularities. The ovaries, as revealed by palpation (palpation by the doctor), are dense in consistency and located behind the uterus.
The chronic form of the disease leads to the following consequences:
- decreased performance
- problems falling asleep
- fast fatiguability
- irritability
- mood changes
Classification
By process localization:
- Unilateral (right-sided or left-sided) oophoritis.
- Bilateral.
Depending on the pathogen:
- Non-specific.
- Specific.
With the flow:
- Spicy.
- Subacute.
- Chronic.
In 25% of cases, the acute process, despite timely treatment, becomes chronic, and chronic salpingitis and chronic oophoritis occupy the main place in the structure of diseases. If we consider the causes of female infertility, then chronic salpingitis and oophoritis occupy first place, and in the case of miscarriage - second.
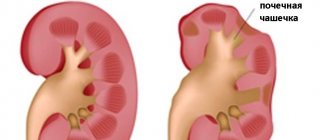
Chronic inflammation of the ovaries is accompanied by impaired development of follicles (folliculogenesis and ovulation are impaired) and their atresia occurs (reverse development of follicles). Fibrous tissue develops in the ovaries and scars form; sclerotic changes also occur in the vessels. The process can be one-way or two-way. What is it - bilateral oophoritis? This means that the ovaries on both sides (right and left) are involved in the chronic inflammatory process, so there is a high risk of infertility.
Chronic salpingoophoritis occurs over a long period of time and with exacerbations. Chronic inflammation of the appendages is accompanied by dysfunction of the nervous, urinary, endocrine and immune systems. In addition, chronic oophoritis is also accompanied by the inclusion of autoimmune mechanisms, as a result of which antibodies to ovarian tissues are produced and ovarian failure quickly develops. As a result, the woman’s risk of infertility increases even more, and the prospects and results of in vitro fertilization worsen. Treatment of a chronically ongoing disease is long-term and includes several stages (inpatient, outpatient and sanatorium-resort treatment).
Acute oophoritis
Typical symptoms for this form of the disease include pain when going to the toilet, constant pain in the lower abdomen, spotting and purulent vaginal discharge, and impaired ovarian function. The temperature may rise. Patients often suffer without sleep, become irritable and lethargic. During sexual intercourse, unpleasant sensations and pain occur, therefore girls with acute oophoritis do not experience any desire for intimacy. The appendages are enlarged and pain is present.
Pathological changes occur in the structure of the fallopian tube. It fuses with the ovary, forming a single inflamed area. When the ovarian tissue melts, purulent discharge from the fallopian tube is observed. The body is exposed to intoxication. If acute oophoritis is unilateral, then the disease can quickly spread to a healthy ovary. In this case, we can talk about a bilateral lesion, which is quite difficult to treat. Inflammation leads to the futility of trying to conceive a child.
Treatment comes only in a hospital. The sick girl/woman is prescribed antibiotic painkillers. During the recovery process, physiotherapeutic and balneological procedures are prescribed to prevent the disease. Complex therapy should also include vitamins. Vaginal suppositories are also prescribed, which helps prevent relapses.
Pathogenesis
Typically, oophoritis (usually salpingoophoritis) develops as an ascending infection from the vagina or uterus due to infection during sexual intercourse or complicated abortions and childbirth. In response to the introduction of the pathogen, an inflammatory reaction of the body occurs.
When the ovaries are involved in the process, their epithelium and adjacent peritoneum are first infected ( periophoritis ). Then inflammation covers the cortical layer of the ovary (actually oophoritis). In the ovary, microcirculation is disrupted, tissue damage occurs, and swelling occurs due to inflammatory effusion. Multiple follicular cysts of varying diameters form inside the enlarged ovary, as in polycystic ovary syndrome. Unlike polycystic disease, in this case there is no thickening of the stroma.
Proliferation is the final phase of inflammation and the number of connective tissue cells in the lesion increases and the number of T and B lymphocytes increases. Connective tissue cells can differentiate into fibroblasts, which produce rough fibrous tissue that replaces normal ovarian tissue. As a result of this, it loses its function.
Sometimes ulcers form in the cavity of the follicle or small cysts, which, merging, form an ovarian abscess , which is considered as a complication of oophoritis. Infectious factors are a prerequisite for the development of autoimmune oophoritis with its characteristic decrease in hormonal function.
The chronic inflammatory process is the breeding ground for the human papillomavirus, cancer and precancerous processes, since local immunity decreases.
Chronic oophoritis
The chronic form of oophoritis is a long-term inflammatory process in the ovaries, which occurs if the human body is weakened. For a long time you may not suspect a pathology, because there will be no obvious symptoms. The consequences are very dangerous: fallopian tube adhesions and infertility.
Typical symptoms of chronic oophoritis:
- aching dull pain in the lower abdomen and groin, intensifying before the onset of menstrual periods, with acute respiratory viral infections and hypothermia
- irregular cycle
- decreased sex drive
- regular heavy leucorrhoea (discharge)
- inability to get pregnant
- feeling tired, irritability, insomnia
- sharp pain during intercourse
Oophoritis can be left-sided, right-sided or bilateral. With bilateral symptoms, the symptoms are blurred and treatment is complicated. Treatment of the chronic form of the disease is aimed at eliminating the inflammatory process and painful sensations, restoring the protective properties of the immune system and the lost functions of the female reproductive system. The doctor must not only cure the disease itself, but also nervous and hormonal disorders that affect women's health.
Exacerbations of oophoritis are treated with immunomodulators. A combination of medication and traditional treatment helps. Folk remedies suggest using herbal medicinal decoctions, making baths, douching and tampons from them. It is also important to eliminate such a symptom as pain, because it affects the state of the cardiovascular and nervous system, provokes nervousness, chronic fatigue and irritability. Antibacterial treatment is indicated in the subacute and acute stages of oophoritis, as well as during exacerbation of the inflammatory process.
Exacerbation of chronic oophoritis
This is a fairly common phenomenon that occurs due to weakened immunity and prolonged inflammation. Treatment is the same as for acute oophoritis. Most often, the disease worsens before scheduled menstruation. Typical complaints are abdominal pain, purulent vaginal discharge, general malaise, etc. Treatment can be inpatient or outpatient. If a tumor process or a focus of suppuration was detected during oophoritis, then this is an indication for surgery. Physiotherapy and balneotherapy methods are preventive.
HOW TO TREAT SALPINGITIS
Self-medication for this disease is unacceptable. Too often, inadequate therapy leads to the transition of the acute and subacute to the chronic form and the occurrence of irreversible processes and complications in the fallopian tubes and inevitable surgical intervention. Unilateral salpingitis is treatable and produces positive results. Bilateral is more difficult to treat, but rarely causes complications if it is noticed in a timely manner.
The actual treatment of inflammation of the fallopian tubes depends on the cause and stage of the disease.
In the case of an acute process, salpingitis is treated in a hospital: rest, ice on the lower abdomen (in the first days), painkillers, anti-inflammatory drugs, antibiotics, etc. In the subacute stage, physiotherapeutic treatment is carefully started (quartz locally or on another area of the body, etc.).
DRUGS FOR TREATING SALPINGITIS
- Antibacterial, broad spectrum;
- Antimicrobial, specific targeting;
- Antifungal;
- Probiotics and eubiotics;
- Nonsteroidal anti-inflammatory drugs;
- Vitamins and minerals;
- Antioxidants and antiplatelet agents;
- Immunomodulators and immunocorrectors.
During the period of rehabilitation and recovery after acute inflammation and in the chronic stage, all types of physiotherapy, mud therapy, hirudotherapy, balneotherapy and other methods are indicated (see below). In case of relapses of the disease, the prescription of antibiotics is not indicated, since exacerbation, as a rule, is not caused by reinfection or activation of autoinfection. If conservative treatment of salpingitis is unsuccessful, and the uterine appendages are significantly enlarged (sactosalpinx), surgical intervention is indicated.
INDICATIONS FOR OPERATION
- Lack of results from medication and physiotherapeutic treatment;
- Inflammatory tumor in the adnexal region;
- Presence of purulent tubo-ovarian formation;
- Tubal form of infertility;
- Formation of pyosalpinx;
- Tuboovarian abscess (purulent inflammation of the fallopian tube and ovary).
- Adhesions causing obstruction of the fallopian tubes (if conservative treatment methods described below are ineffective).
HOW TO PREVENT DISEASE
Prevention of salpingitis includes the fight against abortion, prevention of postpartum and post-abortion complications, careful consideration of contraindications for various intrauterine interventions, timely elimination of foci of infection, effective treatment of inflammatory diseases of the pelvic organs (endometritis, adnexitis, oophoritis, cervicitis). Observance of the rules of intimate hygiene, both personal and during sexual intercourse, is of great importance in its prevention.
ADDITIONAL METHODS FOR SUBACUTE AND CHRONIC SALPINGITIS
| PHYSIOTHERAPY | MUD TREATMENT | GYNECOLOGICAL MASSAGE | AUTOPLASMOTHERAPY | AUTO HEMOTHERAPY | HYRUDOTHERAPY |
Physiotherapy in combination with injections, Laennec drips, gynecological massage, and mud therapy plays an important role in the treatment of inflammatory processes in the fallopian tubes and ovaries. These procedures for the patient are selected individually, taking into account the characteristics of the course and form of salpingitis, age, and contraindications.
DO YOU WANT TO CURE ACUTE OR CHRONIC SALPINGITIS? THE BEST DOCTORS AND EFFECTIVE METHODS ARE HERE!
At the initial consultation, the clinic’s gynecologist determines the range of issues that need to be addressed, carries out the necessary studies (tests, examination, ultrasound) according to indications, and draws up an individual plan. In addition to the generally accepted methods (pharmacological, medicinal, etc.) for treating inflammation of the fallopian tubes, additional effective methods of conservative treatment in gynecology, proven by time and many years of practice, are used according to indications.
Today the reception is held by:
| Bezyuk Laura Valentinovna Obstetrician-gynecologist, gynecologist endocrinologist, specialist in gynecology of children and adolescents. Ultrasound. STI. Reproductive medicine and rehabilitation. Salpingitis. Physiotherapy | Vakhrusheva Diana Andreevna Obstetrician-gynecologist, endocrinologist, ultrasound diagnostics. Inflammation of the tubes, ovaries, infections. Contraception. Physiotherapy. Anti-aging intimate medicine and aesthetic gynecology |
MAKE AN APPOINTMENT WITH A GYNECOLOGIST ONLINE
Left-sided oophoritis
If you are diagnosed with left-sided oophoritis, this means that the pathological process affected only the left ovary. The reason lies in gynecological interventions, infectious diseases of the genital organs, stress, weak immunity and cooling (for example, you sat in the cold for a long time).
With left-sided oophoritis, pain is felt only on the left. Typically, there is an increase in temperature that does not go away when taking antipyretics. Between menstruation, bleeding may occur, which makes the woman very tired. Abdominal pain radiates to the sacrum and lower back. There is constant pain when urinating. Purulent and serous discharge from the genital tract is frequent.
Diagnosis requires a gynecological examination, laboratory methods and bacteriological examination. If the ovary is enlarged and there is pain during palpation, ultrasound of the pelvic organs, hystersalpingoscopy and laparoscopy with visual examination of the fallopian tubes, ovaries and uterus are prescribed.
List of sources
- Abramchenko V.V., Bashmakova M.A., Korkhov V.V. Antibiotics in obstetrics and gynecology. – St. Petersburg: Spetslit, 2000.– 220 p.
- Rational pharmacotherapy in obstetrics and gynecology // Guide for practitioners, edited by V.I. Kulakova, V.N. Serova, M., “Litterra”, 2005, pp. 724–727.
- Serov V.N., Tikhomirov A.L. Modern principles of treatment of inflammatory diseases of the female genital organs. Toolkit. M., 2002.
- Prilepskaya V.N. Features of infectious processes of the lower genital tract. Possibilities of therapy with drugs for local use // Gynecology. 2000; 2 (2): pp. 57–59.
- Abramchenko V.V., Kostyuchek D.F., Perfileva G.N. Purulent-septic infection in obstetric and gynecological practice. St. Petersburg, 1994. 137 p.
Right-sided oophoritis
The pathology is characterized by an inflammatory process in the right ovary. Often, right-sided inflammation is confused with appendicitis, due to very similar symptoms: sharp girdling pain in the lower abdomen, radiating to the lower back. The causative agents are microorganisms and infection. Without timely medical care, inflammation can spread to a healthy ovary.
The cause of inflammation of the right ovary can be gynecological manipulations and operations, intrauterine device, abortion. The disease does not develop if you have a strong immune system. Lack of personal hygiene, adherence to strict diets, frequent changes of sexual partners and alcohol consumption are factors that provoke the disease.
Symptoms of right-sided oophoritis:
- pain in the lower abdomen on the right side
- temperature rise
- weakness and severe fatigue
- vaginal bleeding
- pathological vaginal discharge
- pain during intercourse
- the onset of menstruation at the wrong time (broken cycle)
During treatment, it is important to maintain sexual rest and fully follow the recommendations of the attending physician.
Bilateral oophoritis is diagnosed if the right and left ovaries are inflamed at the same time. The reasons are the same as for unilateral oophoritis. The main manifestations are intense pain in the groin, lower abdomen and lower back. Pathological discharge, vaginal discharge and other symptoms that are characteristic of the unilateral form of the disease are also characteristic of bilateral ovarian pathology.
Bilateral oophoritis develops from a unilateral ovarian lesion. This happens when pathogenic microorganisms pass from the fallopian tubes through the abdominal lining. And salpingoophoritis develops if simultaneous infection of the ovaries and uterine cavity occurs.
The main cause of 2-sided oophoritis: genital infections or microorganisms of normal microflora that began to multiply under the influence of certain factors. In this case, the provoking factor for exacerbation of the disease is unprotected sexual intercourse, hypothermia, a decrease in the protective properties of the immune system, infectious processes in the body, emotional and nervous shocks.
Diagnostics reveals swelling of the ovaries and the appearance of an abscess, which can be felt as a small lump. It is necessary to perform laparoscopy to determine the stage of the disease and the location of the inflammation. If necessary, the doctor may prescribe a puncture and administration of medications.
The goal of treatment is to eliminate intoxication of the body and weaken the inflammatory process. Broad-spectrum antibiotics are used to treat the acute stage. Treatment also includes anesthetics, immunostimulants and vitamin complexes to fight infection. In chronic cases, the patient should be prescribed anti-inflammatory medications and physical therapy.
Prevention of inflammation is a mandatory step. It is necessary to exclude unprotected sexual intercourse, abortion and cooling of the genitourinary system. At the first manifestations of ARVI, it is necessary to urgently treat the disease, preventing its development and chronicity.
Causes of salpingitis
The microbial factor plays a leading role in the development of salpingitis. Salpingitis is caused by staphylococci, Escherichia coli, streptococci, Proteus, gonococci, Trichomonas, chlamydia, fungi and Mycobacterium tuberculosis. In the latter case, tuberculous salpingitis develops. In most cases, salpingitis is caused by associations of microorganisms (staphylococci and Escherichia coli).
Along with the microbial factor, provoking factors are of great importance. These include childbirth, abortion, intrauterine contraception, hysteroscopy, hysterosalpingography, which weaken the barrier mechanisms of the cervix. Behavioral factors are also important: early onset of sexual activity, sexual relations during menstruation, a large number of sexual partners and a high frequency of sexual contacts.
Salpingitis and oophoritis
As already noted, these two pathologies have similar symptoms. Often, inflammation of the ovaries causes damage to the fallopian tubes, that is, salpingitis. The pathogens are various microorganisms that can be combined, so antibiotics may not help in treatment (one drug acts on a specific pathogen, but it turns out that there are several pathogens). Inflammation leads to changes due to which the fallopian tube fuses with the ovary. Pus accumulates in the fallopian tube, which is why the ovarian tissue is destroyed.
Both pathologies under consideration are manifested by severe pain in the lower abdomen, in the left or right side. How severe the pain will be depends on the stage of the disease. Pain is characterized as:
- aching
- acute
- cutting
- pulsating
- aggravated by physical activity
Oophoritis and salpingitis are diagnosed using a method such as ultrasound; laboratory tests, laparoscopy, etc. are important. Treatment depends on the pathogen identified. In the acute stage, the woman is sent to a hospital for treatment. At the beginning of the disease, the patient should remain completely at rest; cold compresses and ice should be placed on her stomach. After this, treatment is carried out with antibiotics and medications that relieve pain. If treatment with medications is ineffective, they resort to surgery.
Signs of purulent salpingitis
Purulent salpingitis is a complication of exudative salpingitis. With purulent salpingitis, the woman’s condition sharply worsens: fever, chills occur, and intoxication increases (dry coated tongue, decreased blood pressure, tachycardia). Palpation of the abdomen is sharply painful, the muscles of the anterior abdominal wall are tense. Vaginal examination reveals a sharply painful, significantly enlarged fallopian tube. Purulent salpingitis is accompanied by symptoms of pelvioperitonitis - local limited peritonitis, which occurs due to infection of the pelvic peritoneum. When purulent contents break into the abdominal cavity, purulent salpingitis leads to diffuse peritonitis.
When purulent salpingitis is diagnosed, conservative treatment is not effective. In this case, only surgical treatment is indicated - removal of the focus of purulent destruction. But even in cases of unilateral tubectomy (removal of the fallopian tube) for purulent salpingitis, a woman after completion of rehabilitation can be referred for IVF.
Oophoritis during pregnancy
The disease is dangerous because it has serious consequences that affect a woman’s ability to become pregnant. Violations of the functions of the appendages, obstruction of the tubes, and adhesions occur. The regularity of menstruation and sexual function are disrupted. Pathologies appear in other organs, such as colitis, pyelonephritis and cystitis. Chronic inflammation of the ovaries can lead to miscarriages, ectopic pregnancies, etc.
For the reasons mentioned above, it is important to detect and treat oophoritis in a timely manner. When planning a pregnancy, it is necessary to undergo a complete examination. With the development of bilateral oophoritis, pregnancy will not occur at all. If there is an infection in the pelvis, the fetus can become infected, then its development is disrupted.
When the function of the appendages is impaired, the body's production of estrogen and progesterone is also impaired. This explains miscarriages if a woman still manages to get pregnant. Then hormone replacement therapy is carried out.
General information
Inflammatory processes of the uterine appendages, which include the fallopian tubes and ovaries, occupy first place among gynecological diseases. In second place is menstrual irregularity, and in third place are endometriosis and infertility.
The problem of inflammatory diseases of the female sphere is relevant in gynecology, in view of the fact that they do not tend to decrease, as the frequency of sexually transmitted infections increases. The importance of the problem lies in the fact that inflammatory diseases of the appendages lead to infertility in 18% of cases.
The infection may be limited to the tubes (inflammation of which is called salpingitis ) and may involve the ovaries ( oophoritis ). What kind of disease is this - oophoritis? This is inflammation of the ovaries, resulting from an infectious lesion. The main spectrum of microorganisms that cause inflammation are chlamydia , mycoplasma , gonococci , ureaplasma and trichomonas . Recently, there has been a tendency towards association of pathogens and the occurrence of mixed infections, and this worsens the course of the disease and its prognosis.
The ovaries are the organ that produces eggs and sex hormones ( estrogens and progesterone ). The fallopian tubes serve to transport eggs into the uterus. Under the influence of complex hormonal mechanisms, a mature egg is fertilized in the tube and moves into the uterine cavity, where it is implanted and pregnancy develops.
Even a minor inflammatory process destroys the normal structure of the ovary and leads to functional disorders. With oophoritis, endocrine function is disrupted (hypo- or hyperestrogenemia), menstrual irregularities occur, and infertility may develop. Since most often the infection enters the ovaries via an ascending route (from the vagina and uterus, if the process cannot be localized), it cannot bypass the fallopian tubes. Therefore, in most cases, the inflammatory process affects the tubes and ovaries ( salpingoophoritis ).
Recently, the number of “erased” forms of the disease with minimal or no clinical manifestations has increased. It is these latent forms of salpingofooritis that are dangerous because, in the absence of treatment or due to inadequate treatment, they easily develop into a chronic recurrent course. Sometimes even treatment taken late increases the risk of complications. In this case, dense adhesions are formed, the anatomy of the pelvis and the function of the pelvic organs are disrupted, and chronic pelvic pain develops.
Diagnostics
Diagnosis of oophoritis is considered a complex process. Symptoms that are characteristic of this pathology may also occur in other diseases. Differential diagnosis is required for the following diseases:
- appendicitis
- ectopic pregnancy
- cyst, etc.
A gynecological examination and medical history are needed at the very beginning when a patient consults a doctor. An examination is carried out on the chair and palpation of the ovary/ovaries. Particular attention is paid to the presence or absence of vaginal discharge and the general condition of the body. The doctor collects anamnesis, including finding out complications after childbirth, if any.
They do laboratory diagnostics, that is, test blood and urine to determine the level of leukocytes. Swabs are taken from the urethra and vagina. The doctor also prescribes, as noted above, an ultrasound of the pelvic organs. Hysterosalpingoscopy may be necessary, which can detect pathological changes in the structure of the fallopian tubes, the cause of which is chronic inflammation of the ovaries.
Also, when diagnosing oophoritis, the body is checked for the presence of infectious pathogens using PCR, ELISA, and RIF methods. Additional studies may be prescribed if purulent or tuberculous inflammation is detected. An informative method for diagnosing the disease in question is laparoscopy. Examine the fallopian tubes, uterus, ovaries; this method is also important for discriminating diagnostics. The main indication for laparoscopy is chronic pain in the lower abdomen, long-term infertility, inflammation of the ovaries of unknown origin.
Treatment
When the diagnosis is accurately established, the stage of the disease is known, then treatment is determined. The acute form, as we have already noted, is treated in the hospital. The patient must remain in bed; cold compresses are applied to her lower abdomen. Desensitizing and painkillers, antibacterial and restorative drugs are prescribed.
Treatment of the chronic form of the disease is complex. An individual course of treatment is drawn up, which includes physical therapy and medication. Physical therapy may include:
- hirudotherapy
- electrophoresis
- gynecological massage
- magnetic therapy
- laser therapy
Often they resort to folk methods of treatment and herbal medicine, which are also used in the prevention of oophoritis. The therapy is long-term, but it must be completed. If the cause of the disease is a sexually transmitted infection, then the partner is also treated to avoid prostatitis and re-infection of the partner. During the treatment period, both are prescribed sexual rest.
Antibiotics for oophoritis are prescribed for relapses of chronic inflammation and intensification of pathological processes in the ovaries. At the same time, they resort to methods of restorative treatment. The choice of antibiotics depends on the body's sensitivity to the drug. To do this, bacteriological culture is carried out and the type of pathogen is determined.
The most commonly used antibiotics to treat oophoritis are:
- Sumamed
- Azithromycin
- Hexamethylenetetramine
- Amoxiclav
- Gentamicin
- Urotropin
- Unidox Solutab
- Doxycycline
- Klindafer
- Doxibene
- Metronidazole
- Dalatsin
- Trichopolum
- Ceftriaxone, etc.
The following medications are used to relieve abdominal pain:
- Aspirin
- Nospaz
- Asalgin
- Spasmalgon
- Tempalgin
Vaginal suppositories are also used for treatment:
- hexicon
- betadine
- suppositories with indomethacin
Prevention of oophoritis
Preventive measures include:
- the use of barrier contraception in cases where conceiving a child is not planned
- prevention of chronic inflammation of the uterine appendages: salpingitis, adnexitis, salpingoophoritis
- paying attention to diet
- treatment of all emerging diseases, including genital
- regular examinations with a gynecologist
- ban on taking baths with a water temperature of 38°C or more
- ban on hypothermia
- control of psycho-emotional balance