Sometimes dentists jokingly say that they can diagnose any patient before he sits in the chair. “The wonders of X-ray vision” or unrivaled professional experience? I hasten to disappoint: neither one nor the other. The point is the widespread prevalence of periodontal diseases. And the diagnosis of “gingivitis” can be given in absentia to the vast majority without making a mistake. So, what is periodontium and what does it consist of?
The periodontium of a tooth is the tissue that surrounds it. More precisely, a complex of tissues. They are interconnected by their common location, development and functions. The structure of the periodontium has four main components:
- gum;
- periodontal ligament;
- tooth root cement;
- alveolar bone (alveolar part of the lower jaw and alveolar process of the upper).
Well, first things first. In this article we will look at the structure of the gums.
The gum is part of the oral mucosa that covers the alveolar bone (1) and surrounds the necks of the teeth (2).
The main task of the gum is to protect the tissues underneath it from mechanical and microbial damage.
Attached gum
From simple to complex: let's start with the attached gum. It is dense, elastic, firmly connected to the periosteum by collagen fibers. Wider in the incisor area (up to 4.5 mm in the upper jaw) than in the chewing teeth. Above, the attached gum borders on the marginal gum, below – on the mucous membrane of the alveolar bone. The border with the marginal gingiva is a small depression called the gingival groove (white arrow). And the mucous membrane of the alveolar bone originates at the mucogingival junction (black arrow).
The importance of sufficient gum volume during implantation
- Aesthetics . During implantation, not only the success of installing the implant itself is taken into account, but also the appearance of the structure relative to the dentition. Installation of an artificial root should not interfere with the fixation of the crown, prosthesis, or interfere with neighboring teeth. In this case, the aesthetic gingival contour must be recreated.
- Functionality . Soft tissues provide nutrition to the bone structure of the jaw and support implant structures. Therefore, even before installing implants, the doctor analyzes the volume and condition of the gums and decides whether augmentation is required.
- Prevention of rejection . A healthy mucous membrane that forms around the implant protects the structure from plaque and bacterial penetration, and reduces the risk of peri-implantitis.
Gingival sulcus
The depth of the gingival sulcus can be determined using a probe (periodontal, preferably). Normally it can be up to 3 mm. But it is worth considering that the gingival groove is not the same on different surfaces of the tooth: the approximal grooves are deeper, and they are shallower on the lingual and buccal sides. With many periodontal diseases, this depth increases (the answer to the question “why?” will be a little lower).
The gingival sulcus is lined with sulcular epithelium (or gingival sulcus epithelium). It is thin, non-keratinizing and is a kind of semi-permeable membrane for gingival fluid, on the one hand, and for microbial toxins, on the other.
Methods
The surgical method is chosen by the doctor based on the gum parameters, width and thickness. Plastic surgery is performed using:
- using your own tissues from the intervention area;
- transplantation of a donor flap from the hard palate;
- application of collagen matrices or membranes.
Membranes are a progressive method of restoration. It differs from others in its high predictability, minimally invasiveness and short rehabilitation period.
Gingival fluid
Gingival fluid is transudate or exudate (more protein compared to transudate) from the connective tissue of the gum and its blood vessels. Normally there is very little of it - 0.5-2 ml; with inflammation this figure increases. The composition of this liquid is very diverse:
- Microorganisms;
- Leukocytes;
- Desquamated epithelium;
- Enzymes;
- Immunoglobulins;
- Other serum and connective tissue components.
It is logical that its composition determines the functions it performs: it cleanses the gingival sulcus, has antimicrobial properties and even improves the attachment of the epithelium to the tooth.
The gingival sulcus (2) is followed by the attachment epithelium (attachment, connective) (3).
Recovery period - healing time, recommendations
After surgery, follow your doctor's recommendations:
- use a protective mouth guard to prevent damage to the surgical site;
- do not eat food during the first 5-10 hours , you can drink water after a couple of hours;
- don't smoke for 3 days;
- stick to a diet - take warm lean foods;
- carry out thorough hygiene - cleaning 2-3 times a day , it is not recommended to touch the surgical site with a brush, antiseptic drugs are used;
- take prescribed antibacterial drugs;
- limit physical activity.
The rehabilitation period depends on the volume of intervention and the chosen surgical method. On average, gums heal in 10-14 days.
Junctional epithelium
The junctional epithelium is a stratified squamous non-keratinizing epithelium (like the furrows). Formed during tooth eruption as a result of the fusion of the oral epithelium of the gum (1) + the primary enamel cuticle. Its length is very small - from 0.25 to 1.35 mm. Interestingly, at the apical end (the one closest to the enamel-cementum junction) its width can be only 1-2 cells. But, despite its far from impressive size, the attachment epithelium performs a number of important functions:
- it is a barrier against bacterial plaques;
- this is access of gingival fluid with protective components to the site of inflammation;
- this is a quick update (every 4-8 days), recovery from damage;
- and, finally, the ability to phagocytose epithelial cells (according to some scientists).
In the figure “Formation of the connective epithelium”: REE – primary enamel cuticle; OE – oral epithelium; JE – junctional epithelium
It is he who is destroyed by marginal gingivitis, and then by periodontitis. And it is precisely with the destruction of the attachment epithelium that the inevitable deepening of the gingival sulcus is associated (the promised answer to the question above).
Pathologies
Factors that can trigger gum disease include mechanical damage, poor hygiene, infection, and the development of ulcers or cancer. Characteristic signs of deviation from the norm are loss of sensitivity, the formation of edema, bleeding and abundant accumulation of plaque on the surface. Common diseases include:
- Gingivitis is an inflammatory process that occurs as a result of chronic pathologies, errors in the selection of prosthetic structures, as well as tartar deposits.
- Periodontitis is an inflammation of bone tissue, often developing from a local to an extended form. It becomes the result of infection or food debris getting into the gum pockets, and, in the absence of proper treatment, leads to a weakening of the structure of the dentition.
At the first signs of abnormalities, it is recommended to undergo diagnostics at a dental clinic. Timely identification of the cause of gum disease allows comprehensive treatment to begin and helps to avoid serious consequences.
Interdental papillae
A number of authors also make interdental papillae (interdental gum) a separate point in the anatomy of the gums. This is the gum that fills the space between the teeth below their contact point. But in terms of their structure, these are all the same parts - marginal (top and edges) and attached (central part).
The shape of the interdental papilla may vary depending on the size of the interdental space. So, in the area of the incisors it is smaller - and the interdental gum there is triangular (in the photo). In molars, its shape is more like a trapezoid.
The shape of the interdental gum may also change as a result of its recession:
Or there may be no interdental papilla at all. For example, at the site of a trema or diastema, this space is tightly connected to the alveolar bone (attached gum):
Since we have sorted out the gum anatomically, it’s time to talk about its histology. Of course, it is full of its own characteristics, but in general, like any mucous membrane, it consists of epithelium and connective tissue (the lamina propria of the mucous membrane).
A small flowchart about the gingival epithelium, so as not to get confused (checkmarks on what we have already talked about):
A few words about the oral epithelium. It covers the entire gum from the tongue, cheeks and lips. That is, the outer surface of the marginal and the entire attached gingiva. It is parakeratinized, or partially keratinized (difference from completely keratinized - in the surface, stratum corneum, there are remnants of the nucleus and organelles).
All its layers are visible in the figure:
- basal (on the basement membrane);
- spiny;
- grainy;
- horny;
- connective tissue.
Cells in its composition:
- keratinocytes (epitheliocytes) – the main ones;
- melanocytes (in figure M);
- Langerhans cells (white arrow) – macrophages;
- Merkel cells – tactile receptors;
The oral epithelium is a mechanical, chemical, water and microbial barrier. On the plus side, there are more specific protective reactions: the epithelium can respond to stimuli by changing proliferation (start dividing and regenerating faster) or cell differentiation, signaling, or even death.
Histological structure
In accordance with the histological characteristics, two components are distinguished in the structure of the gums. These include stratified epithelium and connective tissue.
In the case of epithelium, the basis of the basal layer are cells in the shape of a cube or cylinder, on top of which are sequentially located spiny cells, protein grains (keratohyalin), as well as the outer stratum corneum. The structure of the latter consists of flat cellular elements that do not contain nuclei and are subject to keratinization, which leads to its periodic renewal - due to deeper layers.
The absence of nerve endings or blood vessels in the epithelium is determined by the functional task of the layer. The goal is to prevent pathogenic bacteria and microbes from entering the periodontal tissue. In this case, there is a natural barrier between the basal layer and the connective tissue base, which forms in the form of a membrane septum.
The gum's own plate is two-layered:
- The upper layer is structurally a connective tissue with a loose structure, forming papillae oriented towards the surface and extending into the epithelium. The sensitivity of the gums is caused by the passage of blood vessels, nerve endings, and the central or trigeminal nerve through them.
- The deeper layer is characterized by a mesh structure and is formed from collagen fibers produced by fibroblasts. Uniting with each other, they move into the periosteum area, due to which the gums remain immobile, and the elements of the dentition are arranged in strict sequence.
The connective substance that unites and strengthens connective tissue cells is the matrix, a product of proteoglycan and glycoprotein molecules. The supply of blood is ensured by the gum branches - the location of the capillaries close to the edge of the tissue causes increased sensitivity of these areas.
There is no inflammation with periodontal disease
When does the so-called periodontal disease, there is no inflammatory process in the gums. The clinical picture of “periodontal disease” differs sharply from periodontitis; it is with periodontitis of the tooth that inflammation occurs.
And injections into the gums, endless restorations of the necks of the gums - this is running in circles. Over time, again all the restoration fillings are chipped, and again these patients come to have these fillings restored again. And this happens endlessly
:
And the diagnosis of “periodontal disease” does not go away. As Desna ran away, she continues to leave. The fillings increase, that is, the teeth increase in size, because the gums sag more and more, and nothing useful happens.
When such a patient gets an appointment with me, unwinding his entire tangle of ordeals during the consultation, it becomes clear that all previously performed gum treatment consists of 3
factors:
- Lost time,
- lost money
- shattered hopes.
The diagnosis was incorrect and the treatment was appropriate for the incorrect diagnosis. What went wrong?
Patients should always go for a consultation with such a diagnosis... to an orthodontist
.
Because periodontal disease is an occlusal injury
.
What I see in these patients with signs of periodontal disease is a completely different diagnosis. This is an occlusal injury that can only be corrected by an orthodontist.
Summary -
In this article, we briefly listed the main stages of treatment necessary to quickly relieve inflammation. Removing dental deposits from teeth and anti-inflammatory therapy will relieve redness, swelling, bleeding of the gums, the gums will become denser, pale pink in color, and bad breath will disappear. However, the treatment of a disease such as periodontitis does not end there.
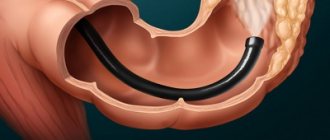
In the case of deep periodontal pockets, and when the gums move away from the teeth, it can be assumed with a high degree of probability that splinting of mobile teeth will be required, as well as one of the surgical methods for treating periodontitis (for example, flap surgery or open curettage of the gums). During flap surgery, a thin strip of marginal gum is removed, which is loose and not attached to the teeth and, accordingly, this reduces the depth of periodontal pockets, as well as the rate of progression of periodontitis.
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a periodontist, 3. National Library of Medicine (USA), 4. American Academy of Periodontology (USA), 5. “Therapeutic dentistry. Textbook" (Borovsky E.V.).
Always treat gum problems
When a patient comes to the doctor, he complains about something. What symptoms does he see a doctor with before receiving a diagnosis of periodontal disease? What worries him?
Literally, patients tell the doctor this: my gums have sagged, my gums have become exposed, my lower gums have receded. And for some reason the symptom of gum subsidence automatically means that the patient has the so-called. periodontal disease.
More experienced patients, who have already heard a lot of professional terms, who delve into the professional colloquial language of doctors, say this: “The necks of the teeth have become exposed a little, the teeth have become a little higher.” But, according to statistics, most patients complain about sagging gums.
And so, when patients come to the doctor with complaints about the problem of exposed tooth necks, the doctor diagnoses them with periodontal disease. Of course, he begins to treat them. And to treat it specifically for periodontal disease.
But time passes, money also goes away, and the question of why the gums recede and the necks of the teeth become exposed, why the gums recede, has not been resolved. And the patient still has periodontal disease.
Gum recession: why gums recede
The formation of gum recession occurs when the surface of the tooth root is exposed. Without consulting a dentist, you will never be able to determine the exact reason why your gums are receding. This is due to a whole range of possible reasons, and in addition there are a large number of predisposing factors that make the risk of recessions more likely. Let's look at them.
1) Occlusal trauma, overload of teeth –
Occlusal trauma means that the contacts between your lower and upper teeth are not ideal, and in some areas there may be so-called “super contacts” (areas of premature overbiting). Normally, when the jaws are closed, the contact of the premolars, canines and molars should first occur, and only lastly the incisors. But if your incisors close first, then after all the other teeth have closed, they will experience overload, which will lead to bone resorption and a decrease in gum level (see photo below).
In addition to improper contact between the upper and lower teeth, bruxism (excessive uncontrolled clenching of the jaws, most often at night) can lead to occlusal injury. Patients usually refer to this condition as teeth grinding during sleep. You can learn more about this disease using the link above.
Exposure of tooth roots as a result of occlusal trauma:
Excessive chewing pressure on the teeth for a long time leads to resorption of the bone around them. Accordingly, in parallel with the decrease in bone level, there is also a decrease in the level of the gums, which primarily becomes noticeable in the area of the lower anterior teeth. For example, if you are missing part of your lateral chewing teeth, this leads to a redistribution of the chewing load on the remaining teeth, which will cause them to be overloaded. The front teeth are not physiologically designed for chewing at all - their function is to bite off food. In the absence of lateral chewing teeth, chewing food occurs with the front teeth, which quickly leads to their overload.
The absence of even 1 chewing tooth on each side can quickly lead to a decrease in the bite height in the lateral parts of the jaws, and this in turn will lead to excessive contact of the upper and lower front teeth (which will also cause bone resorption and gum recession with exposure of the roots of the teeth) . Moreover, a decrease in bite in the lateral parts of the jaws can occur not only due to the loss of several teeth. This can also occur due to excessive abrasion of dental tissues (on the chewing surfaces of molars), due to errors in prosthetics or restoration of teeth with filling materials, as well as as a result of the gradual abrasion of old fillings.
What to do - if you do not have missing teeth, then you need either a “gnathologist” or a very good orthopedic dentist to carry out “selective grinding of teeth” (this procedure will normalize the contacts between the upper and lower teeth, removing all “super contacts”) . If you have a reduced bite height in the chewing parts of the jaws due to the absence of some teeth, you need prosthetics. We are talking about replacing missing teeth with artificial crowns, replacing old fillings on the chewing surfaces of molars with ceramic inlays... But you need to start with a consultation with a prosthetist.
2) Chronic generalized periodontitis –
We have already said above that one of the main reasons why gums recede is their inflammation. It all starts with a completely harmless superficial inflammation of the gums (gingivitis), which is manifested by bleeding gums, their swelling and pain when brushing your teeth. But in the absence of treatment or improper treatment of gingivitis, the attachment of the gums to the neck of the teeth is gradually destroyed, inflammatory bone resorption and the formation of periodontal pockets begin to occur.
Reduced gum level due to gum inflammation –
When bone destruction reaches a certain degree, tooth mobility also joins the symptoms. Destruction of the periodontal attachment, bone resorption, periodontal pockets, tooth mobility - these are all symptoms of the next stage of gum inflammation, which is called periodontitis. Accordingly, because When periodontitis occurs, the level of bone tissue around the teeth decreases, and the level of the gums will also decrease.
Important: please note that a decrease in the level of gums in the area of 1-2 teeth is possible even with the most initial form of gum inflammation - even with catarrhal gingivitis. And for this it is enough simply to have microbial plaque in the area of the necks of the teeth (+ the presence of some predisposing factors, for example, a thin gum biotype). But with chronic generalized periodontitis, subsidence of the gum level occurs immediately in the area of a large group of teeth.
What to do - you need to start with a consultation with a periodontist (this is a dentist who specializes in the treatment of gum inflammation). Treatment of periodontitis includes not only anti-inflammatory therapy and removal of dental plaque, but also splinting of movable groups of teeth and prosthetic replacement of missing teeth. Therefore, in addition to consulting a periodontist, you may also need to consult an orthopedic dentist.
3) Incorrect movements of the toothbrush –
If you brush your teeth with a horizontal motion (instead of a sweeping motion) every day year after year, this can lead to gum recession - especially in the area of the lower front teeth. Typically, such patients not only have receding gums, but also hard tissue defects of non-carious origin appear in the area of the necks of the teeth. Incorrect brushing technique plays an important role in the formation of gum recession - especially in the presence of predisposing factors (thin gums, small height of attached gums, concomitant catarrhal gingivitis, etc.).
4) After correcting the bite with braces -
After correcting the bite with braces, you can often notice a decrease in the level of the gums. What I want to say here... There are only a few good orthodontists, so most of them plan orthodontic treatment without taking into account factors such as the height of the attached gum, the biotype of the gum, the thickness of the cortical plate of the jaw in the area of the teeth being moved. And as a result, we have what we have...
5) In the presence of predisposing factors –
Below we present a number of factors that sharply increase the risks of gum loss and root exposure. In some cases, they themselves can be the cause of gum recession (such as a highly attached frenulum of the lower lip), but most often they increase the damaging effects of the causes that we described above. These predisposing factors relate to the individual anatomical features of the gum structure in different patients.
- If you have a thin gum biotype, thin biotype means a small gum thickness. With the same force of the damaging factor, in patients with thin gums, recession will occur faster and be deeper than in patients with thick gums.
- Thickness of the cortical plate of the alveolus - if your cortical plate of the jaw (the front wall of the alveolus) is too thin.
Let's look at this using the example of the lower incisors. The anterior surfaces of the roots of the lower incisors are covered with a thin layer of bone, on top of which soft gum tissue is already located. In some patients, this layer of bone may be too thin (less than 0.5 mm), which, in the presence of a damaging factor, leads to too rapid bone loss, followed by a decrease in gum height. In some patients it can be even worse. For example, on the front surface of the roots of the lower incisors (in the area of their upper thirds) there may be no bone plate at all. In this case, the upper third of the roots will be covered only by the gum. This situation creates a risk of a recession, i.e. the fact that the gums will recede and the tooth root will be exposed - maximum.
- The height of attachment of the frenulum of the lips - for example, the frenulum of the lower lip may be attached too high to the gum edge, and then the movement of the lips (during conversation and facial expressions) will lead to the frenulum “tearing” the edge of the gum from the teeth. The same will apply to the low-attached frenulum of the upper lip.
- Insufficient level of attached gum – the gum is usually divided into “attached” and “unattached” (see photo below). Above the dotted line is the attached gum, and below it is the non-attached mobile gum. The peculiarity of the attached gum is that it is firmly fused with the underlying tissues and therefore immobile. The unattached gum is mobile, and its peculiarity is that it follows the movement of the lips and cheeks.
Very often the gum recedes on a tooth that has a very small height of attached gum. There is a clear relationship - the lower the level of attached gums, the higher the risk of recession (recession of the gums and exposed roots). When the level of attached gum is low, dentists often recommend performing special surgical operations on the gums, which can increase the level of attached gum and prevent exposure of the roots of the teeth.
What tactics are used to treat periodontal disease?
I want to start with the fact that patients who come with a diagnosis of periodontal disease, they need, every single one, treatment... not from the periodontist to whom they initially turned.
If we talk about the tactics of managing patients with the so-called. periodontal disease, which then come to me again, it’s a shame to voice this, but the treatment of periodontal disease was carried out right up to injections of Lincomycin into the exposed gum.
According to statistics, almost always the treatment of periodontal disease in adults with medications is burdened with a course of some antibiotics and physical therapy.
And most importantly, the task of all these manipulations is completely unclear: what do doctors want to achieve in this way, to destroy some kind of flora or to stop some destructive processes in the gums? It is very difficult for me to say what happens to the competence of a doctor who injects antibiotics for the so-called. periodontal disease, but this is absolute blasphemy. Is it possible to cure periodontal disease by destroying the flora? As a result, the gums will never recover.
Treatment of gum periodontal disease reaches the point of absurdity
I would like to note the widest range of drugs and folk remedies that patients use to attempt self-treatment of periodontal disease at home. Among the folk remedies, one can note the treatment of periodontal disease with hydrogen peroxide, and even treatment with soda:
What about the use of various toothpastes for periodontal disease? What goals do patients have? The purpose of toothpaste is preventative, not curative. And no toothpaste will eliminate inflammation, because there is no such inflammation in periodontal disease.
It is not difficult to guess that in these combinations of procedures the question of how to cure periodontal disease remains open.