Symphysitis is a manifestation of instability of the cartilaginous connection of the bones of the pubis (symphysis) as a result of hormonal changes in the body. Most often, symphysitis appears during pregnancy under the influence of hormones that prepare the woman’s body for childbirth. The mobility of the joint leads to pain in the pelvic area, which occurs even during any movement. There are many ways to help reduce the intensity of pain. In most cases, after childbirth, symphysitis goes away on its own.
As a result, symphysitis appears
A woman's body undergoes many changes during pregnancy. One of them is changes in hormonal levels. Hormones are produced that are responsible for the preservation of pregnancy and the safe bearing of the baby. The hormone relaxin helps soften ligaments. Thanks to this, the pubic symphysis becomes mobile, and the internal size of the small pelvis increases by several millimeters. This facilitates the easiest passage of the fetus through the birth canal. In most cases, symphysitis appears in the third trimester of pregnancy, in rare cases - much earlier, around 22-24 weeks of pregnancy.
When the first symptoms of symphysitis appear, you should consult a doctor monitoring your pregnancy. This is necessary in order to exclude diseases that are dangerous for the mother and child - urinary tract infections or inflammation of the pelvic organs.
Treatment of symphysitis
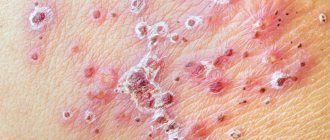
Photo source: shutterstock.com
Most often, there is no treatment for symphysitis during pregnancy and the disease heals with time. If measures to eliminate this diagnosis are taken on time, the prognosis for the disease is quite favorable. During pregnancy, excessive divergence of the pelvic bones is observed in 45% of expectant mothers; after their birth, this number decreases to 25%, and decreases significantly three months after the birth of the child. This is due to the stabilization of hormonal levels and a decrease in swelling of the pubic symphysis. The pain that has haunted the woman for so long also decreases.
It happens that excessive expansion occurs after the baby is born; this is the so-called postpartum symphysitis. It occurs as a result of the birth of a large fetus in a woman with a narrow pelvis, due to severe toxicosis or pathology of bone joints in the past. You can also get rid of postpartum symptoms of symphysitis with the help of a special bandage and a set of exercises. But too large a discrepancy will require special treatment, where physical therapy and medication are added to standard measures.
No pregnant woman is immune from symphysitis, even if such a diagnosis is not made by a doctor, pain may be present in the last weeks of the term. When the pelvic bones diverge, it is necessary to wear a special bandage, take calcium, appropriate vitamin complexes, and consume more dairy and fermented milk products. If inflammation is detected in the semi-joint, the woman takes antibacterial agents.
Aggravating factors
In addition to hormone production, there are several factors that provoke sprains of the pubic ligaments:
- disturbance of calcium-phosphorus metabolism;
- lack of vitamin D;
- increase in body mass index
- history of three or more pregnancies;
- injuries to the pelvic bones, even old ones;
- hereditary diseases of the musculoskeletal system;
- high fetal weight (the expected weight of the child at the time of birth is 4 kg or more);
- insufficient amount of physical activity of the mother.
Symphysitis: causes and treatment
Why symphysitis occurs has not yet been precisely established. There are two main theories to explain excessive divergence of the pubic bones:
- excessive production of relaxin, which leads to excessive relaxation of the symphysis pubis ligaments;
- disturbance of phosphorus-calcium metabolism and vitamin D deficiency.
In addition, the following factors contribute to the development of symphysitis:
- hereditary diseases of bones and joints, for example, a defect in collagen (protein of skin, ligaments, cartilage, bones), leading to excessive joint mobility;
- numerous births;
- past pelvic trauma;
- large fruit weighing more than 4000 g;
- sedentary lifestyle and excess weight;
- symphysitis during previous pregnancies.
If symphysitis is already present, then it is unlikely that it will be possible to completely get rid of it, but you can reduce its manifestations and the feeling of discomfort.
How to recognize symphysitis
The main clinical manifestations of symphysitis during pregnancy are:
- sharp shooting pains in the pelvic area;
- aching pain in the lumbar region, radiating to the abdominal cavity and inner thigh;
- the occurrence of acute pain when raising a leg, transferring weight from one leg to another, or spreading the legs;
- the occurrence of pain with the slightest physical activity, even when walking;
- a pronounced click when performing sudden movements in the pubic area;
- pain in the pubic symphysis during sexual intercourse;
- severe fatigue and fatigue.
The level of pain with symphysitis during pregnancy can vary from mild, almost unnoticeable, to very severe. The pain becomes significantly stronger at the following moments:
- when lifting objects;
- during physical activity in which the hips are actively involved;
- while maintaining a static body position for a long time without changing posture.
During pregnancy, moderate softening of the pelvic joints and stretching of the symphysis pubis (CP) occurs, which contributes to the favorable passage of the fetus through the bony pelvis. However, these changes can cross physiological boundaries, leading to excessive relaxation of the pelvic joints, which is accompanied by the appearance of pain and leads to rupture of the pubic symphysis during childbirth, especially with mechanical influences and surgical interventions.
Despite a fairly clear description of the symptoms of this disease, there is still no common point of view on the terminology of pathological changes in the joints of the pelvis during pregnancy. Thus, in the domestic literature (L.V. Vanina, 1954; L.S. Persianinov, 1964) terms such as “symphysitis”, “symphysiopathy”, “divergence” and “rupture of the symphysis pubis” are used [3], while Foreign authors suggest using the term “sympubis dysfunction” (JDP) [4, 5, 8, 14]. In ICD-10 (2003), pathological changes in drugs during pregnancy are not identified as a separate nosological unit.
The number of cases of symphysis pubis dysfunction varies from 0.12 to 56% [14, 16, 19]. Such large fluctuations in the frequency of DLS can be explained by the lack of a unified definition of this pathological condition, unified diagnostic criteria, as well as insufficient attention to this problem by both patients and doctors.
It should also be noted that, according to foreign literature, there is still no single view on the etiology and pathogenesis of DLS.
In the domestic literature of recent years, there are no publications on this problem. What is clear is that this pathology is associated with pregnancy and disappears after childbirth.
There is no data in the literature on diagnosing the severity of DLS, on the choice of delivery method depending on the severity of the disease, or on the effect of DLS on the condition of the fetus and newborn.
The purpose of our study was to assess the severity of DLS and select an adequate method of delivery in the interests of the mother and fetus.
Material and methods
115 pregnant women with DLS (main group) and 100 pregnant women with a physiological course of pregnancy (control group) were examined.
Clinical and laboratory methods for assessing pain on a 10-point scale, provocative tests (Trendelenburg, Patrick, etc.), ultrasound of the symphysis pubis, X-ray pelvimetry (digital), and magnetic resonance imaging (MRI) were used.
There were 59.1% primigravidas in the main group and 56.0% in the control group. The average age of primigravidas in the main group was 28.35±5.4 years, in the control group - 29.1±5.1 years.
In women with DLS, among extragenital diseases more often than in the control group, mitral valve prolapse was noted (20.9% versus 7.0%), varicose veins (13.9% versus 9.0%), diseases of the visual organs - myopia (19.1% versus 10%), Marfan syndrome - 2.6%, spinal osteochondrosis (4.3% versus 1.0%), which indicates the presence of phenotypic signs of connective tissue dysfunction.
Data on pregnancy complications in women of the main group are of undoubted interest. The most common of them are threatened miscarriage (44.3% versus 17.0% in the control group), isthmic-cervical insufficiency (20.0% versus 6.0%), multiple pregnancy (10.1% versus 2.0 %) and etc.
Pain in the area of the symphysis pubis in pregnant women with DLS appeared in the first trimester of pregnancy in 9.6% of cases, in the second trimester - in 21.6%, in the third trimester - in 62.6% and after childbirth - in 1.7%. Complaints from pregnant women about pain in the pubic and other pelvic joints were an indication for ultrasound, X-ray and MRI.
Ultrasound was performed with the patient lying on her back, using a standard transvaginal convex probe with an operating frequency of 3-3.5 MHz. The study began with studying the upper edge of the LS and gradually moved down along its course. Measurements were taken at several points, within the clearly visible boundaries of the pubic bones. As a result of the study, the maximum diastasis of the pubic symphysis was established.
X-ray examination after 38 weeks of pregnancy was carried out using a low-dose digital X-ray scanning unit "Siberia - N". Filming of the pelvis was carried out in two projections: anteroposterior and left lateral with the patient in an upright position. The surface exposure dose for two radiographs ranged from 52 to 70 mR, with the maximum permissible 1R. On a direct photograph, the transverse dimensions of the pelvis, the width of the symphysis pubis, the possible vertical displacement of the pubic bones, as well as the fronto-occipital size of the fetal head were measured. The direct dimensions of the small pelvis were measured on a lateral photograph. X-ray examination makes it possible to evaluate the size of the pelvis, width, structure of the symphysis pubis and adjacent pubic bones [1].
The MRI study was performed on a tomograph with a field strength of 1 T with the patient in a horizontal position on her back, less often in a position on her side.
Axial tomograms were used to measure the transverse dimensions of the small pelvis, the width of the pubic symphysis, its structure and the structure of the adjacent pubic bones [1].
Results and discussion
To make a diagnosis of DLS, the clinical picture was taken into account, which is characterized by many symptoms, but the main ones are discrepancy of the LS and pain in the area of the pubic symphysis. Almost all pregnant women with DLS (91.3%) indicated pain during palpation of the left limb and when changing body position. Approximately every tenth pregnant woman with DLS experienced edema and swelling above the pubis, a “duck walk,” pain with bilateral compression of the pelvis, tension of the gluteal and adductor muscles, and pain with palpation of the pelvic ligaments during vaginal examination. With a pronounced clinical picture of DLS, a positive Trendelenburg sign (19.1%), a positive Patrick sign (47.5%), a positive test for the inability to actively alternately raise straightened legs (7.82%), etc. were often observed.
To establish the diagnosis of DLS, differential diagnosis was carried out with other pathological conditions (diastasis of the symphysis pubis, osteitis of the symphysis pubis, lumbago, sciatica, herniated intervertebral disc, inguinal, femoral hernia) and for this purpose ultrasound, X-ray examinations and MRI were used.
To determine the severity of DLS, in addition to the severity of the pain component, it is important to assess the size of the discrepancy of the pubic bones, the severity of anatomical changes in the symphysis pubis and adjacent pubic bones.
In non-pregnant women, according to ultrasound data, the width of the symphysis pubis is 3.11±0.6 mm, as pregnancy progresses it increases and in full-term pregnancy it is 5.22±0.54 mm, after childbirth (4-5 days) it is 4.5±0.9 mm.
L.V. Vanina (1954), L.S. Persianinov (1964) distinguished 3 degrees of divergence of the pubic bones with DLS: I degree - by 5-9 mm, II degree - by 10-20 mm, III degree - more than 20.0 mm. Based on the data we obtained using modern research methods, we did not find a discrepancy of the symphysis pubis of more than 13.0 mm.
Based on ultrasound data, X-ray pelvimetry, MRI and clinical manifestations, we identified 3 degrees of discrepancy of the symphysis pubis: I degree - from 5 to 8 mm, II degree - from 8 to 10 mm, III degree - more than 10 mm.
I degree of divergence of the symphysis pubis with DLS was observed in 76.52% of pregnant women, II degree - in 15.65% and III degree - in 7.82%.
The main factors in determining the severity of DLS were the severity of the pain component in the symphysis pubis and the magnitude of diastasis of the pubic symphysis. Mild severity of DLS at a gestational age of 37 weeks or more was established in 53.05% of cases, moderate DLS in 36.52% and severe DLS in 10.43%. It should be noted that the severity of DLS increases as pregnancy progresses.
Since the etiology and pathogenesis of DLS have not been fully established, treatment is not always effective. It is known that this disease is associated with pregnancy, and therefore delivery is the best method of therapy. The goal of therapy is to relieve or reduce pain in the symphysis pubis.
In the first trimester of pregnancy, for pain in the symphysis pubis, paracetamol and multivitamins were usually prescribed, but often no positive effect was obtained. In the second trimester of pregnancy, in the treatment of 30 pregnant women with DLS, in addition to paracetamol, we used a drug containing 250 mg of calcium in 1 tablet, 50 IU of vitamin D3 and minerals (zinc, manganese, copper, boron), orally, starting with 2 tablets 2 times a day. for 2 weeks, followed by taking 1 tablet 2 times a day throughout pregnancy and lactation (prevention of rickets in children). The effect of such treatment in the form of reducing or eliminating pain in the symphysis pubis was established in only 53.3%.
The data of E.V. deserve attention. Mozgovoy et al. [2], who after 20 weeks of pregnancy during DLS prescribed this drug (20 patients) and its combination with ultraviolet irradiation (UVR) of the symphysis pubis (30 patients). Treatment was carried out under the control of bone metabolism and vitamin D levels in the blood plasma. When using a drug containing 250 mg of calcium, 50 IU of vitamin D3 and minerals, pain in the symphysis pubis decreased in 55.0% of pregnant women, and when combined with ultraviolet irradiation (10 sessions), complaints of pain during palpation of the symphysis remained in 25% and completely disappeared in 75%.
The literature provides data on the successful treatment of DLS using another drug, 1 tablet of which contains 500 mg of calcium and 400 IU of vitamin D3, at a dose of 1 tablet per day for 2 weeks (the course of treatment was repeated according to indications).
In the third trimester of pregnancy with DLS, in addition to paracetamol and calcium supplements, we recommended the use of pelvic support belts in combination with physical exercise. The positive effect of wearing elastic and especially rigid pelvic girdles is indicated by J. Depledge et al. [7], H. Ostergaard et al. (1993) and others. N. Kvorning et al. [11], N. Hope-Allan et al. [9], B. Stuge et al. [18] used acupuncture and acupressure and its combination with physical exercise to relieve pain in DLS. J. O'Grady [13] successfully used transcutaneous electrical neurostimulation. J. Scicluna et al. [17] used epidural analgesia to relieve severe pain.
The method of delivery for DLS depends on the size of diastasis and the severity of the pain component, on the characteristics of the structure of the symphysis pubis, the structure of the pubic bones, the size of the pelvis, the estimated weight of the fetus, presentation and condition of the fetus, the readiness of the birth canal for childbirth, concomitant obstetric and extragenital pathology, and the effectiveness of the procedure. treatment.
With a mild degree of DLS - unexpressed pain in the symphysis pubis (1-3 points), diastasis of the symphysis pubis less than 8.0 mm, normal pelvic sizes, readiness of the birth canal for childbirth, average fetal size, with cephalic presentation, in the absence of fetal suffering and extragenital pathology, we delivered women through the natural birth canal. The birth was carried out under cardiac monitoring.
In case of DLS of moderate severity, childbirth is per vias naturalis
considered possible if there was moderate diastasis of the symphysis pubis (from 8.0 to 10.0 mm), moderate pain in the symphysis pubis (4-6 points) and the absence of pronounced changes in the structure of the symphysis pubis and adjacent pubic bones during X-ray or MRI examination , normal pelvic sizes, readiness of the birth canal for childbirth, repeated births, average fetal size, cephalic presentation, absence of intrauterine fetal suffering and severe obstetric and extragenital pathology. The birth was carried out under cardiac monitoring. In the second stage of labor, the Mc Roberts maneuver (bending the legs at the hip and knee joints and spreading to the sides) and the Kristeller maneuver were not used.
With severe DLS, all 12 (10.43%) pregnant women were delivered by cesarean section.
We explain the high percentage of cesarean sections in women with DLS in the entire group (66.74%) by the heavy contingent of pregnant women entering our institution with various obstetric and extragenital pathologies. Even in the control group, the caesarean section rate was also high (41.0%) for the same reason. Caesarean sections were usually performed routinely in the lower segment of the uterus, through a transverse incision under epidural anesthesia.
The frequency of complications during childbirth in women with DLS in the form of untimely rupture of water, intrauterine suffering of the fetus, increased blood loss during childbirth was practically no different from that in women without DLS.
The total duration of labor in primiparous women with DLS was 8 hours 39 minutes ± 1 hour 42 minutes, in multiparous women - 5 hours 52 minutes ± 0 hours 52 minutes, and in the control group, respectively, 8 hours 5 minutes ± 2 hours 6 minutes and 5 hours 46 minutes ±1 h 3 min, i.e. no significant difference was obtained.
Among the complications of the postpartum period, hypogalactia, anemia, and lochiometra should be noted, but no significant differences with similar complications were found in women in labor who do not suffer from DLS. After childbirth, pain in the area of the symphysis pubis decreased and usually disappeared after 5-6 days. If sharp pain appeared immediately after childbirth or in the coming days, then traumatic damage to the symphysis pubis during childbirth was excluded. To clarify the diagnosis, special research methods (ultrasound, MRI, X-ray pelvimetry) were used.
The course of the postoperative period after cesarean section in women with DLS was usually favorable. Complications of the postoperative period included anemia (15.7%) and hypogalactia (3.94%). After abdominal delivery in women with severe DLS, severe pain requiring medical analgesia was observed in 5.26%. Pain in the LM area disappeared by 4-5 days after delivery without special treatment, although diastasis of the LM was recorded by ultrasound.
Of interest is the condition of children at birth and in the neonatal period in women of the main and control groups, delivered through the natural birth canal and by cesarean section. A total of 115 pregnant women with DLS gave birth to 118 children, of which 6 were premature (5.08%).
The assessment of newborns on the Apgar scale in the main group during spontaneous birth in the 1st minute was 7.8 ± 0.62 points, and during abdominal delivery - 7.6 ± 0.64 points, while in the control group it was 7.9 ±0.52 points after spontaneous birth and 7.6±0.8 points after cesarean section. The Apgar score at the 5th minute in the main group during spontaneous labor was 8.6±0.6 points, and during cesarean section - 8.2±0.52 points, in the control group it was 8.5±0, respectively .6 and 8.3±0.5 points.
The majority of children in the main group (83.9%) were placed in the physiological pediatric department, 11.01% in the intensive care unit, 23% in the low-birth-weight neonates department, and 1.64% in the neonatal surgery department (kidney hydronephrosis). Newborns in the control group were 86.4% admitted to the physiological department, 9% to the intensive care unit, and 3.6% to the low birth weight unit.
The average weight of newborns in the main group was 3488.3±478.3 g, and in the control group - 3435±476.3 g, i.e. no significant difference was found.
The early neonatal period in both study groups proceeded smoothly. The average duration of hospital stay in the main group among those in the physiological department after childbirth was 5.1 ± 0.4 days, and after cesarean section - 6.2 ± 0.5 days, in the control group - 5.2 ± 0, respectively. 5 and 6.1±0.3 days.
In conclusion, it should be noted that in pregnant women with DLS, the condition of fetuses and newborns does not differ from that of women in the control group.
Thus, the DLS problem is far from being solved. For the future, it is necessary to standardize terminology and a clear definition of DLS, and improve methods for its diagnosis. Further research is needed to identify the etiology and pathogenesis of DLS for prevention and etiotropic treatment, selection of a rational method of delivery and management of the postpartum period. The etiology of DLS during pregnancy has not been clearly established. It is believed that hormonal, metabolic (the role of calcium), biochemical, immune changes, anatomical features of the pelvic structure, connective tissue dysfunction and other factors play a role in the occurrence of this pathology. Among the possible causes, the role of relaxin is discussed in the literature [10], although not all authors agree with this [12]. There was no correlation between the concentration of progesterone and estradiol in the blood serum of pregnant women with the presence of pelvic pain [10]. A connection has been established between pelvic pain and an increase in the content of collagen types I, II and V and proteoglycans [10, 15].
The most common complaints with DLS are pain in the symphysis, often radiating to the lower abdomen, back, groin areas, perineum, and thigh. Pain with DLS most often (62.6%) appears in the third trimester of pregnancy. Its appearance can be explained by stretching of the joint, which leads to irritation of the nerve endings of the joint, impaired blood and lymph circulation (edema), and impaired tissue trophism. Contributing to the appearance of pain in the pelvis and other joints of the pelvis is the increasing lordosis of the lumbar spine as the duration of pregnancy increases, which leads to a change in statics and increased pressure on the pelvis, the tendons of the rectus and oblique abdominal muscles are stretched at the point of their attachment to the pubic bones, and the pressure of the presenting part increases fetus onto the pelvic ring. A deficiency of calcium and vitamin D3 in the pubic bones, which are involved in the formation of LS, plays a certain role.
The cardinal sign of DLS is diastasis of the left shoulder. When making a diagnosis, special attention is paid to the size of the discrepancy of the pubic symphysis. However, there is not always a direct relationship between the degree of symphysis discrepancy and the severity of the symptoms of the disease, which is consistent with literature data [6, 8].
We are inclined to explain the presence of pain in the joint in the absence of pronounced diastasis by pathological changes in the tissue of the pubic bones at the site of their connection with the cartilage tissue of the joint, which is visible using MRI.
conclusions
1. The main criteria for diagnosing DLS are pain in the left shoulder and its diastasis, confirmed by ultrasound, X-ray pelvimetry or MRI.
2. We recommend distinguishing between 3 degrees of severity of DLS (mild, moderate and severe), because the method of delivery and the outcome of childbirth for the mother and fetus depend on this.
Severity of the condition
In modern medicine, three degrees of the disease are expressed
- 1st degree - the width of the divergence of the bones of the pubic symphysis is 5-9 mm. The condition is tolerated quite easily; the pregnant woman experiences minor pain that occurs during long walks or during physical activity;
- 2nd degree - the width of the divergence of the bones of the pubic symphysis is 10-19 mm. Pain appears, noticeable with any intense movement;
- Grade 3 - the width of the divergence of the bones of the pubic symphysis is 2 centimeters or more. Painful sensations appear even at rest.
Diagnostics
Diagnosis of symphysitis may well be limited to radiography. The pictures clearly show the size of the diastasis and the location of the bones. When a rupture occurs, fragments of ligaments or cartilage may also be visible.
But during pregnancy , using x-rays is dangerous for the developing embryo, so today the Manual Medicine Clinic “Galia Ignatieva MD” uses modern imaging methods:
- Ultrasound;
- MRI, CT.
MRI is most often used in sports medicine.
Rice. 2. Ultrasound of the symphysis during pregnancy
However, differential diagnosis cannot be limited to instrumental studies. To exclude a number of pathologies during pregnancy with similar symptoms , the following is carried out:
- clinical blood and urine tests;
- biochemical blood tests (PCR, enzyme immunoassay);
- assessment of calcium in the blood.
Symphysitis will also be determined on a gynecological chair - examination with a mirror and palpation examination, if the diastasis is significant. The doctor may detect swelling of the pubis and a depression in the form of a vertical strip between the bones.
is the best way to identify symphysitis. The screen clearly visualizes areas represented by different types of cartilage, the condition and integrity of ligaments and soft tissues. The method helps to predict the behavior of the symphysis pubis during childbirth and promptly choose the method of delivery - natural or cesarean section.
How to reduce pain intensity
After confirming the diagnosis, the doctor leading the pregnancy should give some tips and recommendations that will help reduce the level of pain.
Most often this is:
- use of a special bandage;
- taking medications containing calcium and vitamin D;
- monitoring weekly weight gain and monitoring weight in case of excessive work, as excess weight increases pain;
- adherence to a sleep and rest regime, in some cases complete physical rest should be adhered to;
- applying a warm heating pad to the area of the ligaments (here the doctor must tell you about the importance of maintaining a thermal regime);
- light massage at home;
- use of a special orthopedic pillow for the pelvic area;
- lightweight gymnast;
- swimming in the pool (in the absence of contraindications from the doctor).
In some cases, it is permissible to take painkillers. They are prescribed by a doctor. Self-administration of medications during pregnancy without consulting a specialist is prohibited.
Prevention of pain in the symphysis pubis
Like any pathology, symphysitis is easier to prevent than to treat. This is not difficult to do, the main thing is to follow simple rules:
- Watch your diet! Your diet must include: milk and lactic acid products, low-fat cheeses, eggs, meat, poultry, fish, herbs, nuts.
- Do fitness for expectant mothers.
- Swim in the pool: water relieves stress on the spine and joints.
- Take a walk in the fresh air: exposure to sunlight produces vitamin D in the skin.
- Control your weight; extra pounds often contribute to symphysitis.
- Take vitamins and microelements.
- Wear a bandage.
What is the danger of symphysis rupture?
The divergence of the symphysis pubis after or before childbirth causes a lot of unpleasant symptoms in a young mother. However, this condition is not a threat to health or life. But if the divergence of the pelvic bones leads to rupture of the symphysis pubis during childbirth, then we are talking about a serious injury, that is, a pelvic fracture .
Photo of where the pubic bone is located
Provided that the bones have separated by 2 cm, we are talking about a stable fracture that rarely provokes complications. But if the symphyosis has diverged by 5 cm or more, then this condition seriously threatens health. Therefore, treatment of symphysitis after childbirth depends on the woman’s condition – sometimes surgical intervention is required.
After all, when the edges of the bones rupture, they sometimes damage the bladder, urethra, and clitoris. Hemorrhages sometimes develop in the joint area, and this subsequently leads to the development of arthritis . True, such a serious condition requiring surgery is quite rare.
Folk remedies
Photo: yandex.ru
Symphysitis should be treated by a qualified specialist. The use of various traditional medicines is strictly prohibited.
At home, a woman who has the problem in question should monitor her diet. First of all, preference should be given to dairy products (cheese, cottage cheese, milk, etc.), which are rich in calcium. You should also be careful about flour products and fatty foods, as their excess consumption leads to weight gain. In turn, excess weight increases the load on the pelvic ring, and as a result, pain increases.
With symphysitis, it is important to reduce excessive physical activity, refrain from climbing stairs, fast walking, and staying in one position for a long time (over 30 minutes - 1 hour). It is also recommended to perform specially designed physical exercises daily that strengthen the gluteal, thigh and perineal muscles. We suggest the following exercises, which should be performed several times a day:
- Take a lying position. Place your feet as close to your buttocks as possible. Then spread your bent knees to the sides as far as possible and stay in this position for a few seconds, after which you close your knees again. It is necessary to repeat this exercise from 5 to 10 times, gradually increasing the number of exercises.
- Take a lying position. Bend your knees and lift your pelvis so that you form a straight line with your body. It is recommended to perform this exercise 5 to 10 times daily, gradually increasing the number of exercises. If pain occurs, you should stop doing the exercise.
- Get on your knees and place your palms on the floor so that they point forward. The correct position should look like this: arms straight, knees bent at right angles to the body, back straight. As you inhale, round your back as much as possible and lower your head down. As you exhale, slowly return to your starting position. Then, while inhaling, bend your body down as much as possible. As you exhale, return to the starting position. The exercise should be repeated 5 – 10 times.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Diagnostic measures
First of all, a thorough physical examination of the patient is performed. The doctor determines the sensitivity and tone of the muscles of a particular area, resorting to the palpation diagnostic method. It is important to note that palpation can be used to study only the posterior articular sections and only in the case of a small amount of subcutaneous tissue. To make a final diagnosis, additional examination may be prescribed, including:
- Blood chemistry. Against the background of arthrosis of the symphysis pubis, an increase in the level of ESR is noted.
- X-ray. A diagnostic procedure that allows you to confirm or exclude traumatic damage to the pelvic bones.
- MRI, CT. These instrumental diagnostic methods make it possible to detect tumor formations.
- Transvaginal ultrasound (for women). They are carried out in order to exclude pathologies of the pelvic organs, which may be accompanied by pain localized in the area of the pubic symphysis.
The structure of the female pelvis
The pelvis is a closed ring formed by the pelvic bones, coccyx and sacrum. The pelvic bones are made up of the pubis, ilium and ischium. In addition to the main function - supporting the internal organs - the woman’s pelvis performs another very important function at one time - holding the baby during childbirth . Since the pelvis is adapted to perform this function, its cartilage and ligaments are able to “soften”. When a woman’s body releases a special hormone relaxin , the symphysis pubis, where the cartilage is located, also becomes softer and more mobile. As a result, the size of the pelvis gradually adjusts to the circumference of the child’s head.
Prevention
special method for preventing symphysitis . To prevent the development of anomaly it is necessary:
- control weight;
- to live an active lifestyle;
- perform exercises to maintain the muscle corset and reduce pain ;
- eat a balanced diet, introducing foods high in K, Ca, Mg into your diet;
- take vitamin and mineral supplements outside the season of natural fruits and vegetables;
- avoid pelvic injuries.
exercises , which increase blood supply to the pelvic organs, stimulate the process of ossification, and strengthen the pelvic floor muscles, can prevent symphysitis .
Therapeutic methods
Treatment of arthrosis of the pubic joint must necessarily be comprehensive. Its main task is to eliminate etiological factors. The first thing the doctor recommends that the patient do is to reduce the load on the problem joints, for which you need to avoid staying in one position for a long time and get a fixing bandage. Conservative therapy involves the use of the following pharmaceuticals:
- Non-steroidal anti-inflammatory drugs. They alleviate the patient’s condition, but are characterized by an exclusively symptomatic effect.
- Hormonal drugs. Prescribed for severe pain syndrome. It is not recommended to use for a long time.
- Chondoprotectors. They have a targeted effect on the affected cartilage tissue, promoting its regeneration.
- Muscle relaxants. Relieve muscle tension and reduce pain.
- Vasodilators. Designed to improve blood circulation in tissues, so that joints receive more nutrients.
Physiotherapy, massage, and acupuncture are useful to activate metabolic processes in the symphysis pubis. A set of gymnastic exercises perfectly helps to improve joint mobility, restore blood circulation and strengthen muscle fibers. An individual training program is developed for each patient, taking into account the stage of the disease and the degree of damage to the joint.
The operation is indicated for advanced forms of arthrosis, when traditional methods of treatment are powerless. Endoprosthesis replacement is carried out after a comprehensive clinical examination, which confirms the irreversible nature of the destruction.