Causes of bacterial sore throat in children
Among the pathogenic bacteria, it is necessary to highlight pneumococcus, Escherichia coli, streptococcus, and staphylococcus. In young patients, sore throat is caused by mycoplasma, chlamydia and ureaplasma. Slightly less frequently, bacterial tonsillitis occurs with opportunistic microflora that are constantly present in the body. The proliferation of microbes occurs against the background of weakened immunity, exacerbation of chronic infections (for example, sinusitis, sinusitis, caries), hypothermia, vitamin deficiency. Sore throat in children develops when the soft tissues of the mouth are injured and bacteria multiply after contact with dirty objects, toys, dishes, etc.
The pathogen enters the body after bodily contact or through airborne droplets. The peak of the disease occurs in the autumn-winter period and ends in mid-spring.
Reasons for appearance
The most common cause of tonsil damage is group A beta-hemolytic streptococcus. In 80% of cases, it is this pathogenic microorganism that leads to sore throat. In other cases, when diagnosing the disease, the following pathogens are detected:
- staphylococci;
- adenovirus;
- fungi of the genus Candida;
- Coxsackievirus group A.
The main method of penetration of microbes is through airborne droplets, but you can also become infected from a person infected with a sore throat by using common household products. Getting an infection and settling on the tonsils does not always lead to the development of a sore throat. The action of microbes is activated under the influence of provoking factors: hypothermia, sudden changes in ambient temperature, reduced immunity.
The development of the disease is also stimulated by certain irritants that regularly enter the throat: dust, smoke, pollen, wool. With frequent cases of the development of pathologies of the nasopharynx, which can be caused by the proliferation of adenoids or other diseases, the likelihood of developing a sore throat increases.
When purulent inflammation spreads to surrounding tissues, which was initially localized in the paranasal sinuses, the infection will affect the entire nasopharynx, which will also lead to the development of a sore throat.
Symptoms of bacterial sore throat in children
Babies under one year old are very difficult to tolerate the disease. Parents notice the following signs of illness:
- Drowsiness, decreased or lack of appetite, crying and moodiness.
- Refusing the bottle.
- Vomiting after eating.
- Difficulty swallowing food.
- Increased salivation.
- Temperature rises to 40°C.
Older children experience the same symptoms as adults. They complain of discomfort in the throat and pain when eating, so they eat practically nothing. Outdoor games give way to sleep. The voice becomes hoarse, and sometimes the pain in the throat radiates to the ears.
Complications of GABHS-pharyngitis
In most cases, GABHS pharyngitis resolves without complications. Non-purulent complications include acute rheumatic fever, post-streptococcal glomerulonephritis, childhood autoimmune neuropsychiatric disorders associated with streptococcal infection. Purulent complications of streptococcal pharyngitis include necrotizing fasciitis and bacteremia.
The differential diagnosis of GABHS pharyngitis includes both infectious and non-infectious causes of pharyngitis.
The main viral diseases manifested by acute pharyngitis:
- infectious mononucleosis - Epstein-Barr virus (EBV) and cytomegalovirus. More common in adolescents and characterized by fever, severe pharyngitis (which lasts longer than GABHS pharyngitis), anterior and posterior cervical or diffuse lymphadenopathy. Periorbital edema, mild hepatomegaly, and splenomegaly may be present. Patients prescribed ampicillin, amoxicillin (sometimes other antibiotics) may develop a characteristic rash;
- primary HIV infection —may cause an acute retroviral syndrome (similar to infectious mononucleosis) in sexually active adolescents or rarely in sexually abused children. Clinical signs of primary HIV infection include severe cervical or generalized lymphadenopathy and complaints of fever, weight loss;
- herpes simplex virus - pharyngitis caused by the herpes simplex virus, manifested by blistering rashes on the mucous membrane, lips;
- influenza - characterized by fever, cough, headache and myalgia, which occur during seasonal epidemics;
- other viral diseases - enteroviruses, adenoviruses, rhinoviruses, coronaviruses, respiratory syncytial virus, parainfluenza viruses.
The main bacterial causes of pharyngitis:
- streptococci of groups C and G - there is still a debate about the role of these bacteria in the etiology of acute pharyngitis;
- n eisseria gonorrhoeae (gonorrhea) is a relatively rare cause of pharyngitis. Most cases are asymptomatic or symptoms are nonspecific (eg, pharyngeal congestion, swelling or exudate in the tonsil lacunae);
- f usobacterium necrophorum (Lemierre's syndrome) is the cause of most cases of purulent thrombophlebitis of the jugular vein. Clinical signs include strep throat, high fever (39°C), respiratory symptoms, unilateral neck swelling or pain;
- diphtheria - rare in developed countries, but important to consider in patients from endemic areas. Unlike GABHS pharyngitis, which has an acute onset, the onset of diphtheria symptoms usually occurs gradually. A distinctive feature of diphtheria is the formation of a gray filmy coating that adheres tightly to the mucous membrane of the nose and throat, the removal of which leads to bleeding;
- others - tularemia (Francisella tularensis), Arcanobacterium haemolyticum, Mycoplasma pneumoniae.
Non-infectious causes of pharyngitis are diagnosed based on medical history. This may be irritation or dryness of the pharynx, a foreign body (for example, a fish bone), chemical exposure, radiating pain due to dental abscess, acute otitis media.
Treatment of bacterial sore throat in children
After the examination, the ENT doctor gives a referral to donate blood for a general analysis, culture to determine the microflora and its sensitivity to antibacterial drugs. Only based on the results of the examination, treatment tactics are selected and specific drugs of different dosages are prescribed.
The basic treatment regimen is as follows:
- Taking antibacterial agents. Bacterial sore throat cannot be avoided without taking antibiotics. The most commonly prescribed penicillin antibiotics and aminoglycosides in tablet form. Macrolides are prescribed for children. Streptococci are sensitive to these groups of antibiotics, so the proliferation of bacteria quickly stops. Local broad-spectrum antibiotics in the form of a spray relieve inflammation.
- Taking probiotics and eubiotics. They normalize the intestinal microflora after antibiotics.
- Taking antipyretic drugs. If the temperature is above 38°C, then paracetamol-based drugs are prescribed. At temperatures below 38°C, the body fights on its own.
- Rinse with antiseptics to combat pathogenic microflora and wash out pus.
- Taking local medications to relieve sore throat. Dissolving lozenges, tablets, and using a spray relieves local symptoms.
- Vitamin therapy. Vitamin B and C complexes strengthen the body's defenses, helping to recover faster.
- Taking antihistamines. Prescribed for severe swelling of the soft tissues of the throat.
In addition to drug therapy, strict bed rest must be observed. During the first three days, the likelihood of infecting other family members is highest, so you need to provide the patient with a separate sleeping place and household items.
Due to a sore throat, the usual diet is disrupted. The patient eats only liquid and pureed food in small portions, but often. You should drink 2.5-3 liters of clean water to relieve symptoms of intoxication, but you should not drink hot or cold water.
As a rule, improvement after the start of treatment therapy is recorded within 2-3 days. The general course of treatment does not exceed 10 days. If there is a noticeable deterioration in the condition, then this is a reason for hospitalization.
Important to remember! It is strictly forbidden to make compresses, warm the throat and legs, or do inhalations. Such manipulations will increase the proliferation of bacteria.
Surgery in the treatment of bacterial tonsillitis
Often, due to a weakened immune system, tonsillitis worsens frequently (more than three times a year). The tonsils become covered with purulent contents, causing pain and discomfort.
To prevent relapse, some otolaryngologists recommend surgical treatment - tonsillectomy. Surgery is performed under local or general anesthesia and involves excision (removal) of the tonsils.
The operation is also prescribed for complications, when inflammation of the tonsils has caused a soft tissue abscess (peritonsillar abscess).
Classification
Acute tonsillitis (tonsillitis) or primary inflammation can occur in catarrhal, lacunar, follicular, and less often necrotic form. Secondary acute inflammation of the palatine tonsils most often occurs against the background of existing inflammatory or infectious diseases - scarlet fever, diphtheria, typhoid fever, mononucleosis, as well as leukemia,
Chronic tonsillitis is a long-term inflammatory process in the tonsils, with rare or constant relapses of the disease. Exacerbations can be caused by viruses or bacteria, or against the background of acute respiratory viral infections, dental diseases, or a general decrease in immunity.
Specific features of bacterial sore throat
It is often difficult for parents to distinguish bacterial tonsillitis from other types of acute tonsillitis. Because of this, the patient’s condition often worsens.
- A sore throat caused by bacteria can be recognized by the following clinical picture:
- The lymph nodes in the neck and lower jaw become inflamed. On palpation they are sharply painful.
- There is no mucus or redness on the back of the throat.
- Pus accumulates on the tonsils in the form of white or gray-green dots, but it does not extend beyond them. With a viral sore throat, pus spreads over the entire surface of the throat and surface of the mouth.
Sore throat caused by bacteria differs from other types of acute tonsillitis in that the runny nose and cough are mild, diarrhea, nausea, vomiting and indigestion are absent.
Pus plugs in the tonsils
“Congestion in the tonsils” is a separate problem, mostly hygienic, causing bad breath, sometimes also a feeling of pressure or a foreign body.
What is tonsillitis? It is a cast of food that has fallen into a lacuna (a kind of pocket) of the tonsil, tonsil epithelium and bacteria (most often fusobacterium nucelatum, the main bacterium of dental plaque). But this is not pus, since there are no dead leukocytes and bacteria underdigested by leukocytes.
The conditions for the formation of “plugs” are usually dry mucous membranes of the tonsils, which occurs when nasal breathing is impaired and/or air with low humidity.
Often, if you solve the problem with nasal breathing and the humidity of the inhaled air, then the “traffic jams” disappear by themselves.
What's the moral? If there are “traffic jams”, but no sore throat, then you should pay attention to the state of nasal breathing. And only if the problem persists even with a well-breathing nose, should you look for a solution in the palatine tonsils themselves.
Complications of bacterial tonsillitis
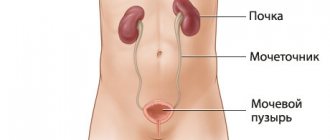
Depending on what causative agent of sore throat is identified and how long the treatment is delayed, the risk of complications increases. Thus, staphylococcal tonsillitis is dangerous due to the development of a pharyngeal abscess due to the spread of inflammation inside. Streptococcal tonsillitis threatens to damage the heart, kidneys and liver and can provoke rheumatism or glomerulonephritis, lower back pain.
The likelihood of complications with bacterial tonsillitis is higher than with viral tonsillitis, so you need to seek medical help in a timely manner and not attempt treatment on your own.
At the ENT CLINIC in Chertanovo, otorhinolaryngologists will quickly conduct an examination, identify the pathogen and prescribe treatment. Our specialists regularly undergo training and improve their skills; they use modern physiotherapeutic techniques and drug therapy regimens in treatment.