Author:
Chekaldina Elena Vladimirovna otorhinolaryngologist, Ph.D.
In some cases, this disease is treated by a therapist or pediatrician.
Quick transition Treatment of acute tonsillopharyngitis
Acute tonsillopharyngitis (angina) is an infectious inflammation of the mucous membrane and lymphatic structures of the oropharynx.
The most common causative agent of bacterial tonsillopharyngitis (hereinafter simply pharyngitis) in children and adolescents is group A beta-hemolytic streptococcus (Group A Streptococcus pyogenes, GABHS). GABHS infection accounts for 15-30% of the total number of cases of acute pharyngitis in children aged 5 to 15 years.
The main symptom of GABHS pharyngitis is a sore throat, with no other signs of acute respiratory viral infection (for example, runny nose, conjunctivitis, cough).
In children over 3 years of age, GABHS pharyngitis begins suddenly. In addition to a sore throat, fever, headache, abdominal pain, nausea and vomiting may occur. Upon examination (pharyngoscopy), diffuse inflammation of the mucous membrane of the posterior wall of the pharynx and tonsils, their hyperemia and swelling are diagnosed. A petechial rash on the roof of the mouth or a scarlatiniform rash on the body (an erythematous, papular rash that usually begins in the groin area and then spreads to the trunk and extremities, followed by desquamation) may be present. Enlarged and painful anterior cervical lymph nodes are palpated.
In children under 3 years of age, symptoms of streptococcal infection are usually atypical. Instead of a clearly defined episode of pharyngitis, they may experience prolonged nasal congestion, low fever, tenderness, and enlarged anterior cervical lymph nodes.
Manifestations in infants under 1 year of age include fussiness, decreased appetite and low temperature.
There is no single sign or symptom that reliably identifies strep throat as streptococcal. Only an assessment of the totality of symptoms allows us to talk about the probable presence of GABHS.
Causes of viral sore throat
As a rule, the virus enters the body when the body’s protective functions are reduced. Immunity may decrease after recently suffering from influenza, acute respiratory viral infections, as well as nutritional disorders (exhaustion). The following factors reduce the body's resistance to viruses:
- Poor nutrition and ignoring vegetables and fruits.
- Staying in an unventilated area. It is for this reason that preschoolers get sick.
- Stress.
The virus can enter by airborne droplets, contact, household and waterborne routes. Children often become infected with viral sore throat when visiting a swimming pool, kindergarten, or school. In close contact with a sick person, the likelihood of getting sick doubles.
Possible consequences of sore throat in children
Angina is one of those diagnoses that, with adequate and timely treatment, have a favorable prognosis for recovery. But if the treatment was incorrect, it is possible that complications will develop, which may appear immediately during the course of acute tonsillitis, or may become delayed and appear after recovery. Complications are also divided into local, which negatively affect the pharynx, and general, which affect other organs and systems of the body.
Local consequences of sore throat in children include:
- purulent lymphadenitis - inflammation of the lymph nodes that occurs with the formation of purulent accumulations, the disease is treated surgically;
- swelling of the larynx - the greater the swelling, the higher the risk of suffocation;
- otitis - the nasopharynx is connected to the ear through the auditory (Eustachian) tube, through which the infection easily penetrates into the middle part of the ear during coughing or sharp blowing of the nose, triggering an inflammatory process in it;
- peritonsillar abscess - a condition in which the cavity located in the tissues around the tonsils fills with pus;
- bleeding from the tonsils;
- the likelihood of transition to the chronic form of acute tonsillitis, that is, the development of chronic tonsillitis, when the symptoms of the disease will return throughout the year, subsiding only during remission.
Common complications include heart, kidney, and joint complications.
Friends! Timely and correct treatment will ensure you a speedy recovery!
All these dangers can certainly be avoided if the disease is diagnosed and treated in a timely manner.
Symptoms of viral sore throat
The clinical picture of viral sore throat is as follows:
- Body temperature rises, but not much. Usually the thermometer shows no more than 38°C.
- Against the background of elevated temperature, a feeling of aching in the muscles and joints appears.
- A throbbing headache develops in the forehead.
- The nose is stuffy and clear mucus is released.
- Cough with clear sputum that persists for several weeks even after successful treatment.
- Sore throat.
- A sore throat develops due to inflammation.
- Inflammation covers the tonsils, palate, and palatine arches. Despite the increased size of the tonsils, there is no white or yellow coating on them.
Types of sore throat
There is a classification of angina according to external manifestations and forms of progression, among which the most common can be identified:
- Catarrhal. The tonsils are enlarged, red, and in places covered with mucus and pus. The tongue is covered with a white coating.
- Lacunar tonsillitis. It has similar manifestations to follicular, but is more severe. Both purulent spots and purulent plaque appear on the tonsils.
- Follicular. The symptoms are similar to the catarrhal form, but more pronounced. Yellowish-white purulent dots appear on the tonsils - this is what inflamed follicles look like.
- Phlegmonous. Purulent melting of the tonsils, which occurs with a weakened immune system, massive infection with microbes, or with improper treatment of milder forms of tonsillitis. Most often it is one-sided.
- Herpes sore throat. On the tonsils there are rashes in the form of blisters, redness, acute pain and fever. Develops when infected with the Coxsackie virus.
Follicular and lacunar forms refer to purulent tonsillitis. Pus accumulates in the tonsils, which is released when pressed.
Treatment of viral sore throat
Before treatment, it is necessary to diagnose and identify the pathogen. If the viral nature of the occurrence is confirmed, then, as a rule, the treatment regimen is as follows:
- Taking antiviral drugs. They speed up the fight against viruses and reduce recovery time. Basically, the ENT doctor prescribes tablet forms of drugs, but in severe cases injections are used.
- Taking antihistamines. They reduce the severity of intoxication and reduce swelling of the throat.
- Use of painkillers, anti-inflammatory non-steroidal drugs.
- Taking antipyretics based on ibuprofen or paracetamol. Recommended only when the temperature rises above 38°C.
- Taking immunostimulants. To strengthen and restore the patient's immune system, immunostimulating agents are prescribed. In addition, they enhance the effect of antiviral drugs. Children are prescribed in the form of drops or suspensions.
- Gargling. Gargling with herbs, antiseptics, and ready-made preparations reduces pain in the throat and eliminates inflammation.
The otorhinolaryngologist recommends drinking as much water, fruit drinks, warm tea, juices, and herbal infusions as possible, since the disease causes dehydration. The liquid removes toxins and viruses from the body.
Throughout the illness, you should stick to bed rest and not have a sore throat on your legs. If you follow bed rest for 2-3 days, the recovery time is significantly reduced, and improvement in well-being occurs on the second day.
The air must be humidified and the room ventilated. It is imperative to adjust your diet, namely to exclude smoked foods, spicy foods, too hot or cold foods, which will irritate the inflamed tonsils.
Usually the disease goes away completely within 6-7 days.
Treatment for sore throat
The patient is hospitalized in the infectious diseases department only in complicated cases. Most often, angina can be treated on an outpatient basis. The treatment method consists not only in eliminating the general symptoms of angina, but also in influencing the causative agent of the disease. The patient is prescribed:
- Regular gargling with saline solution or special antibacterial agents. During treatment, the deep parts of the pharynx should be affected, so when rinsing, it is recommended to tilt your head back.
- Local preparations with antibacterial and analgesic effects: tablets, sprays, lozenges.
- Treatment with antipyretic drugs if necessary.
- Antibiotics, which are prescribed only after evaluating the results of laboratory tests of blood and smears. Antibacterial drugs may have varying degrees of sensitivity to a specific group of pathogenic microorganisms. When treating a bacterial infection, antibiotics of the penicillin group, macrolides or cephalosporins can be prescribed.
During treatment of angina, the patient should be kept in bed. It is recommended to eat gentle foods that do not irritate the throat, mainly vegetable and dairy products. Due to the high prevalence of sore throat, a sick person should use separate personal hygiene products and utensils, and limit contact with others.
It should be remembered that at the first signs of the disease you should consult a doctor. Ignoring the symptoms of sore throat or poorly treated disease can provoke complications and also contribute to the development of a chronic latent form, which will enter the acute phase when the immune system is weakened.
Preventive measures consist of increasing the body's defenses by taking vitamin complexes and a balanced diet, daily walks in the fresh air, eliminating irritating factors, quickly responding to characteristic symptoms, and limiting contact with infected people.
Specific features of viral sore throat
Viral tonsillitis differs from other types of tonsillitis in the milder course of the disease, as well as in the following:
- Signs of the disease increase gradually, not abruptly.
- The temperature rises slightly.
- Does not require antibiotics.
- Local symptoms are not very disturbing.
- The clinical picture is aggravated by diarrhea and nausea.
- A sore throat is accompanied by a cough.
- There are no purulent plugs on the tonsils.
At the ENT CLINIC in Chertanovo, otolaryngologists will successfully diagnose the disease and individually select an adequate treatment regimen. The clinic has modern physiotherapeutic treatment methods in its arsenal, which make it possible to effectively and quickly cure a sick child.
Diagnosis of sore throat
The success of treatment will depend on timely and competent diagnosis. The first stage of the examination is to examine the condition of the patient’s pharynx, during which the attending physician will assess the main signs of the disease: the degree of enlargement of the tonsils and the presence or absence of purulent plaque. It is also necessary to assess the degree of enlargement of the lymph nodes in the ears, neck and back of the head.
Taking blood tests will determine the degree of increase in leukocytes and ESR, characteristic of bacterial tonsillitis. With viral sore throat, the leukocyte level remains within normal limits or decreases slightly, and the erythrocyte sedimentation rate increases slightly.
To determine the causative agent of the disease, cultures of mucus from the oropharynx are examined in laboratory conditions. This is important for determining the class of the disease and competently prescribing medications for the treatment of sore throat. For complicated or particularly acute symptoms, the attending physician may prescribe an ultrasound of the neck.
Causes and routes of infection
The very name of the disease already makes it clear that the source of infection is a variety of viruses. These can be herpes viruses, influenza, Coxsackie viruses, ECHO viruses, adenoviruses, enteroviruses and others. Therefore, the disease is conventionally divided into adenoviral, influenza and herpetic.
The disease is highly contagious: you can become infected during a conversation, by sneezing, through dishes, toys, and food. Viruses that enter the body reach the surface of the tonsils and settle there. From the moment of infection, the patient remains a source of infection for another 30 days. Many factors increase the likelihood of developing the disease:
- cold season;
- improper and unbalanced diet;
- lack of personal hygiene;
- hypothermia (for example, caught in the rain, eaten cold ice cream);
- smoking in front of a child;
- bad ecology;
- climate change;
- weak immunity;
- the presence of a chronic source of infection in the body (for example, chronic tonsillitis);
- carious teeth;
- allergic reactions;
- tuberculosis, diabetes and other diseases;
- stressful situations.
Sore throats caused by influenza viruses or adenoviruses usually occur during the cold season, especially during outbreaks of epidemics, when the body's defenses weaken. Herpetic sore throats are more common in the summer. In order to understand in time that we are dealing with viral tonsillitis, it is necessary to be able to distinguish the main symptoms of the disease in a child.
Why does tonsillitis occur?
Among the possible causative agents of bacterial infection, group A beta-hemolytic streptococcus (GABHS) is of primary importance. It is the cause of the vast majority of cases of tonsillitis and is one of the most dangerous pathogens 2. Therefore, it is customary to divide acute tonsillitis into streptococcal, non-streptococcal (viral) and fungal.
Acute bacterial tonsillitis (tonsillitis) is transmitted from person to person by airborne droplets. Typically, the disease develops after contact with sick people, but in some cases healthy people who are carriers of the bacteria can become infected.
Possible complications
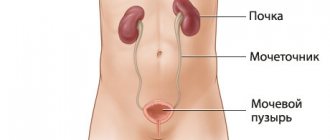
Correct and timely treatment of bacterial tonsillitis is aimed at minimizing the risk of complications. GABHS can affect not only the tonsils, and therefore requires a careful approach to treatment. Common complications of tonsillitis: • abscess in the pharynx; • endocarditis (inflammation in the heart caused by GABHS); • otitis (inflammation of the auditory canals); • sinusitis or sinusitis (inflammation of the sinuses); • kidney damage; • arthritis5.
The most common complication of incorrectly or untimely treated tonsillitis is chronic infection 4.
Treatment of bacterial tonsillitis
In the treatment of tonsillitis
bacterial origin, the key role is played by the use of antibacterial drugs.
They can only be taken if the infection is caused by bacteria. These groups of drugs are not used for prevention of acute respiratory viral infections. The drug is selected taking into account the most likely causative agent of infection. Relief may occur the very next day after starting treatment. If the drug is chosen correctly, the symptoms
go away quickly. However, the antibiotic course must be completed completely, otherwise there is a high risk of developing recurrent or chronic inflammation 2.
Additional drugs for the treatment of bacterial tonsillitis: • antiseptic local agents (sprays and aerosols); • local painkillers; • anti-inflammatory gargles; • antipyretic drugs.
Bacterial tonsillitis, especially provoked by GABHS, is dangerous due to its complications. Therefore, you need to carefully approach the treatment of the disease. It is recommended not only to take certain medications, but also to ensure complete physiological and psychological rest. Strict bed rest, plenty of warm drinks, normal sleep, and periodic ventilation of the room help speed up recovery.
Chronic bacterial infection
Chronic tonsillitis
does not show symptoms most of the time, but often flares up and gives the classic manifestations of a sore throat. An infection in the tonsils can be suspected if tonsillitis develops 2 times a year or more often 4.
It is important to carry out timely treatment of chronic tonsillitis so as not to resort to radical measures in the form of tonsil removal. One of the recommended drugs for the treatment and prevention of chronic tonsillitis is Imudon®
.
The drug contains lysates (particles of destroyed pathogens), which activate the throat’s own immunity and fight the causes of the disease and its symptoms: bacteria, viruses or fungi 6. It is especially important to note that Imudon®
acts not only on the surface, but also penetrates into the tonsils where infection often hides. It is this “hidden” infection that causes repeated episodes and leads to chronic tonsillitis.
Imudon®
does not irritate the mucous membrane, helps reduce inflammation 7, normalizes the microflora of the oral cavity 8 and does not cause resistance, unlike local antibiotics, which should be taken only if there is an urgent need, which should only be determined by a doctor. The use of any antibiotics - systemic or local - must be strictly justified and prescribed by a doctor. Selecting and taking them on your own can lead to negative consequences in the future.