18.12.2020 Sputum
- mucus produced by the trachea and bronchi, mixed with secretions from the nasal mucosa and saliva. What is it for? With it, dust and microbes are removed from the body, which inevitably get inside with our breath. This substance in itself is not a sign of disease: a healthy body generates approximately 100 ml of clear sputum every day - it is quietly swallowed and dissolved by gastric juice.
Another thing is a pathological process in which up to 1.5 liters of viscous mucus per day can be produced. In this case, it is coughed up and may look completely different. The color of sputum when coughing indicates the specifics of the disease and its severity.
Causes of productive cough
A cough is called productive,
accompanied by the release of mucus. White sputum, as well as other shades, is expectorated. A productive cough occurs when:
- acute upper respiratory tract diseases;
- chronic lung diseases;
- inflammation in the nasopharynx, which is accompanied by accumulation of mucus;
- allergies;
- presence of an addiction: smoking;
- reflux (penetration of stomach contents into the esophagus).
There are many diseases that begin their development with a nonproductive (dry) cough. During therapeutic measures, it becomes productive (white sputum is coughed up).
White sputum when coughing cleanses the respiratory system of pathogenic microbes.
If the pathological condition lasts more than three days, you need to see a doctor.
Classification
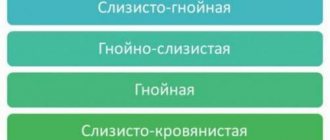
The consistency of sputum can be thick, viscous or thin and watery. When settling, in some cases it is divided into 2 or 3 layers. Based on physical properties (color, smell, transparency, other macroscopic characteristics), the following types of sputum are distinguished:
- Serous.
Isolated in acute left ventricular failure accompanied by pulmonary edema. Characterized by the absence of odor, watery consistency, and an abundance of foam. Serous sputum is usually colorless, sometimes has a pinkish tint. - Mucous.
The appearance of mucous discharge indicates the onset of inflammation of the respiratory tract or the attenuation of the activity of an acute pathological process. Sputum is coughed up in small quantities and is colorless, viscous mucus. - Mucopurulent.
Formed in the acute period of many respiratory diseases. This type of secretion is characterized by increased viscosity and the presence of yellow or green impurities. - Purulent.
Appears with severe inflammation, suppurative processes of the respiratory system. The consistency of the purulent secretion is liquid, the color is green or yellow-green, and sometimes there is a putrid odor.
Perhaps there are shocking photos of medical operations hidden here that show blood and guts.
Are you over 18 years old?
Yes
No
Purulent sputum
What does it mean if the discharge has no color (transparent)
If there is clear mucus, this does not mean that you can calm down and not consult a doctor. This type of sputum often occurs without coughing. The causes of the pathological condition lie in lesions of the nasopharynx.
If clear mucus comes out when you cough, in some cases this indicates infectious pathologies. Lack of color is usually characteristic of their chronic course. Colorless sputum is caused by:
- pathologies of the cardiovascular system (discharge is observed in a small volume);
- oncological diseases (accompanied by a strong cough, after which sputum comes out);
- laryngitis (cough lasts for a long period of time, little is secreted);
- allergic reaction (discharge caused by irritation of the internal membranes).
The causes of hyperproduction of mucus during coughing can be various factors. It is possible to establish the exact nature of its origin only with a complete diagnosis.
Symptoms
When mucous masses constantly “stand” in the throat, the patient wants to swallow them. Such actions (if the secretion is too thick) can cause vomiting and nausea. This condition usually occurs in parallel with other characteristic signs that patients complain about when visiting an ENT doctor:
- sore throat;
- a feeling of a lump in the throat that cannot be gotten rid of;
- a constant desire to cough, although the cough does not bring relief; coughing attacks are especially severe at night;
- discomfort when swallowing food;
- bad breath caused by pathogens multiplying in the throat;
- swollen lymph nodes;
- Loud snoring.
To understand how to treat a sore throat, you need to consult an ENT doctor to determine the cause of postnasal drip.
If the symptom is in an adult without fever
White sputum when coughing without fever in adults manifests itself in the following pathological conditions:
- allergy;
- heart failure;
- foreign objects in the air duct;
- inhalation of chemicals;
- nicotine addiction;
- chronic bronchitis in remission;
- neoplasms in the respiratory organs, gastrointestinal tract.
Infectious and non-infectious causes provoke white mucus. In the second case, it is easier to get rid of the pathological condition: you need to give up addictions and adhere to a healthy lifestyle.
About wet cough
Among the most common reasons for seeking medical help in the autumn and winter, the leading place is occupied by a wet cough.
Cough is a protective reflex that occurs in response to mechanical or chemical irritation of the lower respiratory tract and laryngeal receptors. A wet cough can be a symptom of one of the serious diseases such as: allergic rhinitis, bronchitis, pneumonia, lung cancer, congestive heart failure. Video: types and causes of cough
Doctors call a wet or moist cough a certain concept - “productive”, since with a wet cough there is a result - mucus from the bronchi moves out. The human body begins to independently cope with the cleansing of phlegm - this is how the healing process is carried out.
A wet cough accompanies respiratory tract infections such as acute respiratory viral infections and acute respiratory infections . Sometimes it happens that with an allergic rhinitis, a wet cough appears as a response to mucus that gets from the nose into the larynx. Sputum can form during bronchitis and pneumonia. All diseases associated with the formation of a wet cough require competent, comprehensive and effective treatment.
Foamy and viscous cough
When passing through the respiratory tract, sputum may become slightly foamy.
Normally, the volume per day should not exceed 10 ml. When it comes out, it is swallowed back. If everything is in order with a person’s health, the discharge has no odor.
Viscous sputum appears with allergies:
- if the pathological condition is severe;
- with frequent contact with a provocateur (allergen): the mucous membrane swells because of this, swelling occurs.
If the discharge is caused by an allergic reaction, there should be no admixtures of pus or blood clots in the mucus.
White or yellowish viscous sputum occurs with bronchial asthma and indicates a prolonged course of the disease. When the pathological condition worsens, the mucus becomes viscous and transparent. Sputum of this nature is called glassy.
If viscous mucopurulent discharge is observed, this indicates the addition of an infectious agent.
If viscous sputum occurs, you need to undergo diagnostics. If its consistency is quite thick, the mucus can clog the airways. This will lead to serious complications.
Why is mucus formed?
The production of mucous masses by the nasopharynx is a natural phenomenon. They perform a moisturizing and protective function. Mucous masses trap foreign particles, pollen, and bacteria that enter with the air and prevent them from descending lower into the trachea and lungs. As soon as these foreign agents enter the mucous membranes, the amount of secretion produced increases, and the person has a desire to clear his nose or cough. When the irritant is removed from the body, secretion production returns to its previous level.
Normally, a person does not notice the process of formation of mucous masses - they are swallowed along with saliva.
The accumulation of mucus in the throat becomes noticeable when it is produced continuously and thickens. The patient directly feels how mucous masses flow along the back wall of the pharynx and accumulate in it. During the daytime, the accumulation of sputum is not so disturbing - it is swallowed and does not greatly irritate the cough receptors. But if you take a horizontal position, for example, at night while sleeping, the mucous masses cannot freely pass inside and stagnate in the throat. This causes severe coughing attacks, which can even provoke vomiting.
When a person comes to an otolaryngologist and says: “I constantly swallow mucus in my throat,” the first thing the ENT doctor will do is find out why mucus accumulates in the throat.
Only after establishing the true cause of mucus in the throat, it will be possible to prescribe the correct treatment.
What other color can sputum be?
White sputum when coughing can be a response to pathogenic microflora in the respiratory system, a sign of the development of bronchial asthma.
Mucus can have other shades.
Its basis is
water with glycoproteins, fats, antibodies. Depending on the components, the color of the discharge also changes. It can vary from faint yellow to brownish.
Yellow
Yellowish discharge indicates the development of diseases:
- bronchitis;
- pneumonia;
- sinusitis.
A yellow tint usually appears when sputum is mixed with purulent discharge. This is a dangerous pathological condition that requires immediate medical attention. The sooner treatment is started, the better the prognosis. Yellowish sputum is also observed in heavy smokers.
Green
A greenish discharge indicates the following pathologies:
- bronchitis of various pathogenesis;
- lobar pneumonia.
The pathological condition may be accompanied by fever, difficulty breathing, and chest pain.
With blood
Red sputum indicates internal hemorrhage. In this case, clots and streaks of scarlet color are observed in the discharge. If the blood begins to clot, its color becomes rusty.
Sputum with blood is observed when:
- pneumococcal pneumonia;
- malignant neoplasms in the lungs;
- tuberculosis;
- pulmonary embolism.
Internal bleeding poses a serious threat not only to health, but also to life. Therefore, if you experience red sputum when coughing, you should immediately visit the hospital.
Brown
Brown mucus when coughing usually has a non-infectious cause and is associated with destructive processes in the lungs caused by exposure to tobacco smoke or other toxic substances (for example, at work).
It is impossible to establish an accurate diagnosis from sputum alone. You need to undergo diagnostics. Only a specialist in a clinic can do this.
Treatment
Help before diagnosis
To improve the discharge of viscous sputum, the postural drainage method is used: patting and tapping on the chest, being in a position with the head end down. Patients in satisfactory condition are recommended dosed physical activity. Special breathing exercises work effectively. Thick sputum production is a symptom of serious illness, so you should consult a doctor.
Conservative therapy
The main drugs for eliminating viscous sputum are mucolytics. Medicines consist of proteolytic enzymes and other active substances that thin bronchial mucus, improve expectoration, and eliminate congestion. To increase the effectiveness of mucolytics, they are combined with secretomotor drugs, which increase the volume of mucous secretions and accelerate their elimination. For etiopathogenetic purposes, therapy is also used:
- Antibiotics
. Prescribed for prolonged pneumonia, aggravated chronic bronchitis and bronchiectasis. They are selected taking into account the antibiogram. As a rule, a combination of 3-4 drugs intended for long-term use is selected in the treatment regimen for tuberculosis. - Bronchodilators
. Medicines from the group of beta-2 agonists and M-anticholinergics expand the lumen of the airways and improve the removal of viscous sputum. They eliminate the phenomena of shortness of breath and obstruction, and are effective for providing emergency assistance during an attack of suffocation. - Anti-inflammatory drugs
. Mild forms of pulmonary diseases respond well to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs). Inhaled corticosteroids are also used, which relieve swelling of the bronchi and reduce mucus production. For long-term therapy, those suffering from bronchial asthma are prescribed sodium cromoglycate. - Antiallergic drugs
. Tablet forms are used: antihistamines, leukotriene receptor inhibitors. For atopic bronchial asthma in the period of remission, allergen-specific immunotherapy is performed.
Physiotherapeutic techniques are effective for liquefying viscous sputum: inhalations with alkaline solutions and medications, vibration massage of the chest, electrophoresis. Patients are recommended to take exercise therapy and regular breathing exercises. For chronic respiratory diseases, courses of speleotherapy and sanatorium-resort treatment are indicated.
conclusions
- White, frothy sputum produced in moderate quantities (no more than 100 ml per day) is normal. It is produced by the glands of the trachea and large bronchi. The purpose of the secretion is to cleanse the respiratory system from pathogenic microorganisms.
- If the sputum changes its consistency, color, acquires a specific odor, or contains admixtures of pus and blood, you should immediately contact a medical facility. This may indicate the development of dangerous pathological conditions.
Shortness of breath in bronchial asthma
Frequent attacks of shortness of breath during exacerbation of the disease are characteristic. There is a violation of breathing frequency, as well as rhythm and depth.
The shortness of breath that accompanies patients with asthma manifests itself precisely when exhaling. The time to exhale increases due to the narrowing of the lumen.
Often an attack of shortness of breath “forces” the patient to take a sitting position. A person suffering from asthma raises his shoulders, rests his hands on his knees, and begins to take large gulps of air. This situation is commonly called orthopnea in medicine.
An attack of shortness of breath helps a person suffering from asthma to remove excess carbon dioxide from the body and saturate it with oxygen[1].
Diet for bronchial asthma
Following a diet significantly speeds up the healing process. Among other things, this allows you to avoid food allergens.
People with asthma should not eat:
- smoked meats;
- fatty meats;
- citrus;
- seafood;
- strawberries;
- eggs;
- nuts;
- chocolate;
- apricot;
- peach;
- tomatoes.
Can be eaten:
- chicken;
- doctor's sausage;
- oat cookies;
- Rye bread;
- fruit and vegetable salads;
- coffee;
- tea;
- cereal porridge with butter;
- uncooked soups.
You should limit the consumption of foods such as sugar, milk, salt, sour cream and baked goods. It is also worth following a diet: eat small portions, but 4-5 times during the day[5].
Bibliography:
[1] Ovcharenko S.I. Bronchial asthma: diagnosis and treatment / S.I. Ovcharenko // RMJ, 2002. – No. 17 (10). – 766 p.
[2] Fedoseev B. G. Possibilities of preclinical diagnostics and mathematical prediction of the risk of bronchial asthma (dissertation) / B. G. Fedoseev. - M.: State Educational Institution VP "St. Petersburg State Pediatric Medical Academy", 2005. - No. 2. - P. 35-40.
[3] Tereshchenko S. Yu. Efficacy of various modes of maintenance anti-inflammatory therapy for mild/moderate bronchial asthma in children / S. Yu. Tereshchenko // Allergology. - 2006. - No. 2. - 13-23 p.
[4] Gushchin I.S. Cetirizine is a standard H1 antihistamine [electronic resource]. – Access mode: www.health–medix.com. – (Date of last access: 10/16/17).
[5] Diet No. 9 [Electronic resource]. – Access mode: https://www.medicina.ru. – (Last access date: 10/1/17).
[6] Instructions for use of the medicinal product for medical use Cetrin®. – Registration number: P N013283/01
Diagnostics
The initial examination of a patient with complaints of mucous sputum is often performed by a general practitioner, who, if necessary, gives a referral to an otolaryngologist or pulmonologist. To make a preliminary diagnosis, it is enough to collect complaints, auscultate the lungs, and visually examine the tonsils and pharynx. The plan for clarifying diagnostic studies includes the following methods:
- ENT examination.
With direct and indirect laryngoscopy, the doctor assesses the condition of the laryngeal mucosa, identifies signs of inflammation and hypertrophy. Using a fibrolaryngoscope, a biopsy of atypical areas is performed. If a chronic runny nose is suspected, anterior and posterior rhinoscopy provides valuable information. - X-ray of the OGK.
Carrying out an x-ray in two projections allows us to identify changes typical of inflammatory or tumor processes of the bronchopulmonary system. To clarify the diagnosis, targeted studies are prescribed: fluoroscopy and MRI of the chest organs. - Endoscopic diagnostics.
During bronchoscopy, the mucous membrane of large and medium-caliber bronchi is visualized. The method is used to diagnose chronic bronchitis, neoplasia, fibrotic changes. Using endoscopy, biopsies for histological examination and bronchial lavage water are taken. - Sputum analysis.
Culture of bronchial mucus is necessary to identify viral or atypical bacterial infections. When microscopy of mucous sputum, attention is paid to pathognomonic crystals and spiral-shaped accumulations of mucus. To exclude tuberculosis, microscopy of the material after special staining is required.
Among laboratory methods, a general blood test is informative, allowing one to differentiate inflammatory and other pathologies of the respiratory system. In a biochemical study, acute-phase indicators are studied. Serological tests aimed at searching for antibodies to pathogenic microorganisms are recommended. To measure the function of external respiration and diagnose chronic diseases, spirometry and peak flowmetry are indicated.
Sputum analysis