Community-acquired pneumonia is an infectious disease characterized by an inflammatory process in the lungs. The disease most often develops during influenza epidemics and acute respiratory viral infections. Patients with mild pneumonia can be treated on an outpatient basis. In cases of moderate to severe pneumonia, they are hospitalized in a therapy clinic.
The Yusupov Hospital employs professors and doctors of the highest category, who are leading experts in the field of pulmonology. To diagnose the disease, innovative examination methods are used to identify the pathogen, the localization and extent of the pathological process, and the severity of the disease. Doctors take an individual approach to the treatment of each patient, prescribing the most effective modern drugs with minimal side effects.
Causes of community-acquired pneumonia
Community-acquired pneumonia is conventionally divided into 3 groups:
- pneumonia that does not require hospitalization;
- pneumonia requiring hospitalization of patients in a hospital;
- pneumonia requiring hospitalization of patients in intensive care units.
The therapy clinic is staffed by experienced doctors and nurses. They treat each patient carefully. The rooms are equipped with air conditioning to ensure comfortable temperature conditions. Patients receive complete nutrition, rich in proteins and carbohydrates, and are provided with individual hyena products.
Patients with severe pneumonia are hospitalized in the intensive care unit. Resuscitation doctors monitor the functioning of the respiratory and cardiovascular systems around the clock and determine the level of oxygen saturation in the blood. If there are indications, artificial ventilation of the lungs is performed using stationary and portable expert-class devices.
The following types of community-acquired pneumonia are distinguished: pneumonia in patients without impaired immunity and pneumonia in patients with impaired immunity against the background of the advanced stage of AIDS or other diseases associated with impaired immune system.
Aspiration pneumonia develops in patients with swallowing disorders. Vomit can enter the respiratory tract during a disturbance of consciousness, stroke, acute traumatic brain injury, or during an epileptic attack.
Community-acquired pneumonia develops when microorganisms enter the respiratory tract. There are the following routes of infection for pneumonia:
- microaspiration of oropharyngeal contents;
- inhalation of aerosol containing microorganisms;
- hematogenous spread of microorganisms from foci of infection located outside the lungs;
- spread of infection from neighboring organs.
Pneumonia develops in the event of a weakening of specific or nonspecific protection, a large number of bacteria that have penetrated into the alveolar part of the lungs, or the penetration of microorganisms that are highly aggressive.
The most common causative agent of community-acquired pneumonia with a mild course is pneumococcus. Currently, great importance is attached to the occurrence of pneumonia in the presence and treatment of mycoplasma and chlamydia, Haemophilus influenzae and gram-negative enterobacteria, viruses and legionella. In patients with aspiration pneumonia, the more typical pathogens are gram-negative enterobacteria and anaerobic microflora.
Treatment
It is fundamentally important to determine the patient’s management tactics - whether he should be hospitalized or whether treatment can be carried out on an outpatient basis. For these purposes, you can use the CURB-65/CRB-65 scale, which involves assessing a number of indicators (presence - 1 point, absence - 0):
C —impaired consciousness
U - blood urea nitrogen more than 7 mmol/l (not taken into account in CRB-65)
R — respiratory rate ≥ 30 per minute.
B - systolic blood pressure < 90 mm Hg or diastolic blood pressure < 60 mm Hg. Art.
65 - age 65 years and older
Explanation:
0 points - the patient belongs to group I (mortality 1.2%) and is treated on an outpatient basis.
1–2 points correspond to group II (mortality 8.15%), patients in this group are subject to hospitalization with observation and dynamic assessment of the condition.
3 points and above - patients are subject to emergency hospitalization; mortality in this group can reach 31%.
Symptoms and diagnosis of community-acquired pneumonia
Pneumonia (community-acquired pneumonia) is manifested by clinical symptoms such as weakness, fatigue, nausea, lack of appetite, and impaired consciousness. Patients are bothered by a cough with sputum production and chest pain.
When examining a patient, the doctor may detect cyanosis, the lag of one half of the chest during breathing. During percussion, a shortening of the sound above the lesion is determined. During auscultation, weakened or bronchial breathing, crepitus, dry or moist rales are heard.
The diagnosis of pneumonia without radiological signs of pneumonia is invalid. Doctors at the Yusupov Hospital do x-rays of the lungs in two projections or large-frame fluorography. If the clinical picture does not correspond to radiological data, computed tomography is performed.
The purpose of microbiological research for community-acquired pneumonia is to isolate the pathogen from the source of infection. In a general blood test, the number of leukocytes and the erythrocyte sedimentation rate increase.
The diagnosis of pneumonia is considered established if the patient, against the background of an infiltrate in the lung tissue detected on an x-ray, has at least two clinical signs:
- acute onset of the disease with high body temperature;
- cough with sputum;
- physical signs of compaction of lung tissue;
- leukocytosis.
Diagnostics
The “gold standard” for diagnosing pneumonia is chest radiography . If pneumonia is caused by “typical” bacterial pathogens, then lobar condensation syndrome with air bronchograms is characteristic. In pneumonia caused by atypical microorganisms, bilateral basal interstitial or reticulonodular infiltrates are detected. With any pathogen, inflammation mainly affects the lower lobes of the lungs.
In staphylococcal pneumonia, radiographs show abscess formation, multilobar lesions, spontaneous pneumothorax, and pneumatocele. For pneumonia caused by K. pneumoniae, the upper lobes are typically involved in the process; destruction of the pulmonary parenchyma with the formation of abscesses is also recorded. Abscesses also occur in community-acquired pneumonia, the causative agents of which are M. pneumoniae, S. pneumoniae, and C. pneumoniae.
False-negative results on chest x-rays of patients with community-acquired pneumonia can occur when:
- neutropenia
- the body loses too much fluid
- early stages of the disease (up to 24 hours)
- pneumocystis pneumonia
The doctor may prescribe a CT scan as a diagnostic method because this method is considered highly sensitive.
Laboratory research methods
In the ICU, patients with pneumonia are tested for vital signs and arterial blood gases. A general blood test shows the number of leukocytes at the level of 15x109/l, which indicates the bacterial nature of the disease. But pneumonia can be caused by bacteria in some cases with lower white blood cell counts. To assess the severity of the disease, you need to perform certain biochemical tests :
- glucose
- urea
- liver function markers
- electrolytes
Microbiological examination
This study is needed to decide on therapy. The following microbiological studies are relevant:
- Gram stain and culture of sputum or lower respiratory tract material
- blood test
- study of Legionella spp and S. pneumoniae antigens in urine
- analysis of pleural fluid, if available
- study of material from the lower respiratory tract using PCR or culture
- study of material from the lower respiratory tract using direct immunofluorescence
- serological tests for Legionella spp. and atypical pathogens initially and over time in the absence of PCR diagnostics
Bacteriological testing in patients on mechanical ventilation is carried out using tracheobronchial aspirate. In 30-65% of all cases, doctors receive negative results. This can be explained by the absence of sputum in 10-30% of patients with community-acquired pneumonia, and 15-30% of patients were already given antibiotics before this test, which affected the results.
Among the express methods for diagnosing pneumonia, the detection of microorganism antigens in urine is relevant. Their sensitivity is 50-84%. Also, in some cases, the PCR method is used, but with it, interpretation of the results can be difficult. Serological tests are usually performed to identify atypical bacteria.
Analysis of sputum and aspirate may show a false negative result due to the fact that the sample is “contaminated” with microflora that lives in the oropharynx. Therefore, they resort to transtracheal aspiration, bronchoscopy with protected brush biopsy and BAL, transthoracic fine needle aspiration.
Treatment and prevention of community-acquired pneumonia
Most patients with signs of community-acquired pneumonia can be treated on an outpatient basis. The antibiotic is chosen empirically, before receiving the results of a microbiological study, since any delay in antibiotic therapy for pneumonia is accompanied by an increased risk of complications.
The choice of initial therapy depends on the severity of the disease and clinical signs of pneumonia. To treat mild pneumonia on an outpatient basis, doctors prescribe oral amoxicillin and amoxicillin clavulanate. If pneumonia caused by atypical pathogens is suspected, oral macrolides or respiratory fluoroquinolones (levofloxacin, moxifloxacin) are used.
At the therapy clinic, pulmonologists prescribe comprehensive treatment for community-acquired pneumonia. Indications for parenteral antibiotic therapy are:
- disturbance of consciousness;
- severe pneumonia;
- violation of the swallowing reflex;
- functional or anatomical causes of impaired absorption.
For mild pneumonia, doctors use amoxicillin clavulanate, ampicillin, and parenteral cephalosporins of the second and third generations. Alternative drugs include intravenous macrolides or respiratory fluoroquinolones. If aspiration pneumonia is suspected, amoxicillin clavulanate or a combination of b-lactams with clindamycin or metronidazole is prescribed.
For severe pneumonia, a combination of third generation cephalosporins and macrolides is used. An alternative regimen is a combination of fluoroquinolones with third-generation cephalosporins. After receiving an adequate response to parenteral administration of antibacterial drugs, they switch to oral antibiotics.
Prevention of pneumonia includes a set of specific and nonspecific measures. To prevent pneumonia, it is necessary to observe a work and rest schedule, ventilate work and living areas several times a day for 30 minutes, regularly do wet cleaning, and eat well. It is recommended to play sports, do breathing exercises, quit smoking and alcohol abuse, and promptly sanitize foci of chronic infection. Vaccination against pneumococcal infection is carried out for older people with concomitant pathologies that increase the risk of developing the disease. For this, the Pneumo 23 vaccine (made in France) is used.
Forecast
The mortality rate of patients with severe community-acquired pneumonia hospitalized in the ICU is high and ranges from 22 to 54%. An unfavorable prognosis may be due to the following factors:
- performing mechanical ventilation
- patient age 70 years or older
- bacteremia
- bilateral localization of pneumonia
- need for inotropic support
- sepsis
- P. aeruginosa infection
- ineffectiveness of initial (initial) antibiotic therapy
The fatality rate is high when community-acquired pneumonia is caused by Legionella spp., S. pneumoniae, P. aeruginosa, or Klebsiella pneumoniae.
Can pneumonia occur separately from ARVI and influenza?
- Maybe. This is an infectious disease that is transmitted from person to person. Everyone in the body has a complex and multi-stage defense mechanism that does not allow viruses and bacteria to penetrate into the deep respiratory tract: microbes settle during aerodynamic filtration, on the mucous membranes, in the larynx, in the branches of the bronchi - so to speak, “at the bends”.
The bronchi also contain ciliated epithelium, which is in constant motion towards exit into the oral cavity. Mucus is secreted there, which carries the germs back. Plus the immune system works.
Pneumonia is not only a complication of viral diseases. It was during its study that, for example, they discovered legionella, which loves to live in air conditioners. In 1976, more than 200 military veterans attending an American Legion convention in Philadelphia fell ill. Several dozen later died from this previously unknown disease. There was just air conditioning there.
The massiveness of the dose and high virulence - infectiousness, in other words, played a role. This is exactly what we are seeing now with coronavirus. It itself is highly contagious and active, so the body, especially if it is weakened, cannot protect itself from it. Although it is known that about 20% of those infected are asymptomatic.
District hospital.
Dmitry Lyamzin.
Types of disease
Depending on the pathogen that caused the inflammatory process, the following types of inflammation of the left lung are distinguished:
- bacterial;
- viral;
- fungal;
- parasitic.
According to the prevalence of the inflammatory process, focal, segmental, lobar and lobar left-sided pneumonia are distinguished. The most common type is left-sided lower lobe pneumonia. The lower lobe of the left lung is poorly ventilated and therefore stagnant processes develop there. Bacteria that enter the lower parts of the lung multiply quickly and cause an inflammatory process.
Left-sided upper lobe pneumonia is less common, since the upper parts of the lung are well supplied with blood and ventilated, and congestive processes in them are excluded even when the patient is on bed rest. Inflammation of the upper lobe of the left lung develops against the background of a serious immune deficiency or due to the pronounced pathogenic properties of the pathogen.
Left-sided segmental pneumonia affects the pulmonary segments within one lobe. With lobar pneumonia, the inflammatory process can spread throughout the entire left lung.
There are 3 degrees of severity of left-sided pneumonia:
- light;
- average;
- heavy.
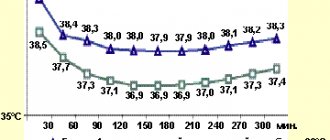
A mild degree of pneumonia is characterized by mild intoxication, no impairment of consciousness, and an increase in body temperature to 38°C. Blood pressure is normal, tachycardia is no more than 90 beats per minute, there is no shortness of breath at rest, a small focus of inflammation is detected by X-ray.
With a moderate degree of pneumonia, there are signs of moderate intoxication (clear consciousness, sweating, severe weakness, body temperature rises to 39 ° C, blood pressure is moderately reduced, tachycardia is about 100 beats per minute), respiratory rate is up to 30 per minute. peace. Radiographs show pronounced infiltration.
Severe pneumonia is characterized by signs of severe intoxication (fever 39-40°C, clouding of the breath, adynamia, delirium, tachycardia over 100 beats per minute, collapse), shortness of breath up to 40 per minute at rest, cyanosis. X-ray reveals extensive infiltration. Patients with mild inflammation of the left lung can be treated on an outpatient basis, but with moderate or severe clinical course of the disease they require inpatient treatment.
How to treat pneumonia
— This is primarily antimicrobial therapy. Plus symptomatic treatment - mucolytics, bronchodilators. This is individual for each patient. General: antibiotics.
However, you need to understand that antibiotics do not work on the virus. That’s why we always say that if you have ARVI or influenza, you can’t “prescribe” these drugs to yourself. This way you will only weaken the immune system, and if the microbial component also joins, then the body’s reserves will be exhausted, and this can lead to more serious complications.
For pneumonia during swine flu, there were several antiviral drugs with proven effectiveness. Now, with coronavirus infection, it is quite difficult to decide on therapy, since experience in using certain medications is only being gained.
It’s good that the epidemic did not start here, we have the opportunity to use the developments of our Moscow colleagues, they regularly review methods. On October 1, we already had the eighth version of the methodological recommendations.
Doctors, hospital
unsplash
What are the dangers of pneumonia?
- Respiratory failure and generalization of the process - that is, sepsis. In addition to the lungs themselves, the heart, kidneys, and brain are also affected. There may be extensive pulmonary edema, infectious-toxic shock, multiple organ failure. This can ultimately be fatal.
If a person has suffered a mild form of pneumonia, then it is recommended to avoid hypothermia for a month. In the case of covid pneumonia with a large volume of lung damage, there is a high probability that respiratory failure will remain for a long time, maybe even forever.
This is due to the fact that so-called pneumosclerosis occurs when the lung tissue is replaced by connective tissue that is not capable of breathing. Such people complain of constant shortness of breath and the inability to endure intense physical activity.
People need long-term rehabilitation, including physical therapy. A diet high in proteins, vitamins, and fiber is required.
Sometimes the help of a psychotherapist is required, as we observe cognitive impairment due to hypoxia. Plus, many survivors of severe forms of COVID-19 may have a persistent fear of death.