Testicle
Testicle, testis, is a paired gland in the shape of an ellipse in the lower part of the scrotum. The length of the testicle of an adult male is 4.5 cm, width - 3 cm, thickness - 2 cm, weight - about 25-30 g.Components of the testicle: medial and lateral surface, facies medialis et lateralis , anterior and posterior edges, margo anterior et posterior , upper and lower ends, extremitas superior et inferior . It is attached to the spermatic cord, being tilted with its upper end forward and its lateral surface slightly backward. On the posterior edge is the so-called epididymis epididymis . The testicle consists of parenchyma enclosed in a dense connective tissue tunica albuginea ; from which the testicular septa go inward, septula testis , which divide the gland into testicular lobules, lobuli testis .
The mediastinum of the testis, mediastinum testis, is a thickening of the tunica albuginea of a wedge-shaped spongy structure. It consists of conical-shaped lobules from 100 to 250. The lobule consists of tubules 70–100 cm long and 140 microns in diameter. The seminiferous tubules contain the seminiferous elements from which sperm develop. At the apex of the lobule, 3–4 seminiferous tubules merge into straight seminiferous tubules, tubuli seminiferi recti .
Having entered the mediastinum of the testicle, the straight seminiferous tubules anastomose with each other, forming the testicular network, rete testis . From this network in the mediastinum, up to 18 efferent testicular canaliculi, ductuli efferentes testis, are formed, which pierce the tunica albuginea and enter the head of the epididymis.
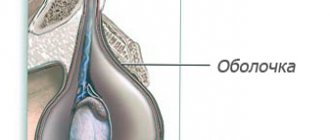
The testicle with its epididymis is enclosed in the tunica vaginalis testis . forming a closed serous cavity around them. Like all intraperitoneally located organs, the testicle is directly covered by a visceral plate, lamina visceralis , which passes along the posterior edge of the testicle into the parietal plate, lamina parietalis .
The visceral plate fuses along its entire length with the tunica albuginea: the area free from it, through which nerves and vessels enter the testicle, is present only from the posterior part. The epididymis, epididymis , is a long and narrow structure lying along the posterior edge of each testicle. The epididymis consists of three parts, it contains the upper part - the head of the epididymis, caput epididymidis , the middle - the body of the epididymis, corpus epididymidis of a triangular shape, and the east of the epididymis located below, cauda epididymidis, the continuation of which is the vas deferens, ductus deferens .
The head of the epididymis is formed by the so-called cones of the epididymis, lobuli epididymidis (coni epididymidis) . On the head of the epididymis there is a testicular appendage, appendix testis appendix epididymidis ), a rudimentary organ consisting of connective tissue. Above the head there is another rudimentary formation - the appendage appendage of the testicle, paradidymis, in which there are blind protrusions, the so-called deviating ducts, ductuli aberrantes (upper deviating duct, ductulus abberans superior ), which have lost connection with the excretory duct. The epididymis is covered with a visceral plate, next to which is located the slit-like sinus of the epididymis, sinus epididymidis.
Testicular diseases: testicular torsion
During adolescence, young people who play sports or ride a lot of bicycles may experience testicular torsion. This condition is a sharp twisting of the spermatic cord with rotation of the nucleus around its axis. Symptoms include sudden, very severe pain (often at night) with rapidly increasing swelling of the scrotum, accompanied by nausea and vomiting.
Testicular torsion
If such ailments occur, you need to see a urologist as soon as possible. The doctor must surgically correct the torsion within 4-6 hours, since torsion leads to poor circulation, which can lead to testicular infarction. Then it will be impossible to save the organ and it will have to be amputated.
Losing one testicle does not threaten fertility, but many men become very emotional about the procedure and view amputation as a “diminishing masculinity.”
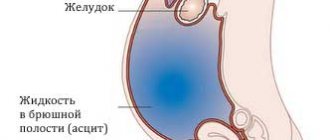
Hydrocele of the testicles in a child
In childhood, testicular hydrocele is usually congenital in nature and often (in 80% of cases) goes away on its own.
Congenital hydrocele in a child most often occurs due to embryonic disorders during pregnancy. In the fetus, not only the testicle, but also part of the peritoneum, called the “vaginal process,” descends into the scrotum. Under normal conditions, the hole in the processus vaginalis should close; if this does not happen, then water begins to accumulate in the child’s scrotum.
When the opening of the processus vaginalis closes, the child’s hydrocele disappears on its own. In other cases, if testicular hydrocele begins to bother your child and he has difficulty urinating, you should immediately consult a urologist! Only a specialist can distinguish testicular hydrocele from an inguinal hernia and provide adequate assistance. Also, an older child may experience acute hydrocele of the testicle, which appears, for example, due to injuries to the genital organs (in this case, lymphatic fluid mixed with blood and pus accumulates in the cavity between the testicle and its membranes). This condition requires emergency medical attention.
Postoperative period
Rehabilitation is an important stage after surgery, during which it is very important for patients to follow the instructions of the attending physician. Wearing a suspensor is a must, as this ensures good blood circulation in the scrotum and minimizes the load on the spermatic cords.
The specialist prescribes antibacterial and painkillers for the patient’s quick recovery. Recommendations after plastic surgery of the testicular membranes are as follows:
- Avoid heavy physical activity for two months.
- Abstain from sexual intercourse for three weeks.
- Avoid direct UV rays and swimming in open water for the first month.
After surgical treatment of dropsy, relapses are extremely rare. A man needs to be prepared for the fact that hematomas or swelling of the scrotum may form at the site of the intervention, which will go away on their own.
The operations described are considered the most effective and therefore quite common. It is important to trust their performance only to experienced surgeons in order to get rid of the pathology without complications.
Diagnosis of hydrocele of testicular membranes
Diagnosis of testicular hydrocele includes a number of studies that can be used to correctly diagnose:
- Initial examination and palpation (palpation) of the scrotum and external genitalia;
- Ultrasound examination of the scrotal organs. Ultrasound examination allows you to accurately determine the amount of fluid, the structure of the testicle, the presence of organs from the abdominal cavity (intestinal loops) in the scrotum;
- In complex cases, in the presence of testicular formations of unknown origin, additional studies are required to confirm or exclude other diseases.
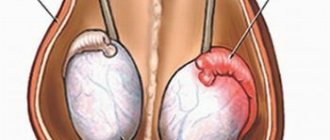
Testicular diseases: varicocele
Varicose veins of the spermatic cord, caused by defects in the venous valves, are a common cause of infertility. The scrotum has many vessels that drain blood away from the testicle. If their valves do not function, blood stagnation and varicose veins occur.
Varicocele
Slow blood flow causes an increase in scrotal temperature. Overheating of the testicle provokes changes in the composition of sperm and hormonal disorders.
Varicose veins of the testicle are not very painful. There is a feeling of heaviness in the testicle and a nagging pain in the groin. A doctor can easily recognize the disease by examining the testicles and performing an ultrasound.
Varicose veins come in different sizes, from small ones that you can barely feel to large ones that look like a bunch of grapes. The only effective method of getting rid of the pathology is surgery (classical or laparoscopic).
Testicular diseases: inflammation of the testicles - orchitis
Inflammation of the testicle is rare, but it is very painful. The pathology is accompanied by swelling of the testicles and high temperature, reaching up to 40 ° C.
Infection occurs in two ways:
- when bacteria or viruses enter the nucleus with blood from another source of inflammation in the body;
- pathogens enter through the vas deferens, usually caused by urinary tract infections.
Almost always, the epididymis is affected first, then the testicle itself. The swelling continues until a hydrocele forms (the content of the scrotum increases due to the accumulation of serous fluid).
Orchitis
In young men, a common cause of orchitis is mumps, a viral disease. The symptoms are the same as for a bacterial infection, but treatment occurs without antibiotics. After a few days, the inflammation goes away on its own.
In contrast, acute bacterial orchitis is treated with antibiotics. This is necessary to avoid an abscess that requires surgery.
Treatment of hydrocele (hydrocele)
Treatment of hydrocele of the testicular membranes (hydrocele) is only surgical.
Today, there are two methods for removing accumulated fluid from the testicular membranes: 1. puncture of the fluid; 2. opening the cavity of the testicular membrane with fluid, the second stage is removal of accumulated fluid and subsequent suturing of the wound.
The puncture gives a temporary positive effect, alleviating the patient’s condition. Performed using a syringe. Puncture is a quick method of providing assistance to the patient; subsequently, there is a constant accumulation of fluid in the membranes of the testicle.
Radical surgery performed for dropsy is performed under spinal anesthesia and is painless. The duration of hospitalization is one day. Upon discharge, the patient is given recommendations to limit physical activity for 1 week, wear tight underwear and bandages for one week.
Preparation for surgical treatment
The preparatory process for surgery is standard. Before the operation, the patient must undergo an examination: the doctor will examine the groin area, then perform an ultrasound to determine the volume of accumulated fluid. If necessary, additional diagnostic procedures may be prescribed.
Before surgery, it is important to recover from colds and other inflammatory reactions. The operation is postponed until the patient has completely recovered from such diseases. Before plastic surgery, a man needs to shave his scrotum and pubis; this can be done at home.
Symptoms of hydrocele of the testicular membranes
Signs of hydrocele:
- an increase in the size and volume of the scrotum. In this case, it is often impossible to palpate the testicles. Smoothing of the skin of the scrotum is noted;
- dull aching pain in the scrotum. In acquired chronic forms of dropsy, pain is not observed;
- symptom of fluctuation when pressing on the enlarged half of the scrotum (protrusion of the membranes of the contralateral testicle from the place of pressure is noted);
- body temperature may rise;
- discomfort associated with difficulty wearing underwear and walking;
- rupture of testicular contents due to thinning of the testicular wall, observed when a large amount of fluid accumulates.
The amount of hydrocele may vary. In advanced situations, the amount of hydrocele can reach several liters and cause discomfort during sexual intercourse, walking, and even when urinating. With congenital forms of dropsy, the amount of fluid increases during the day and decreases during sleep.
An acute form of hydrocele of the testicular membranes occurs as a result of orchiepididymitis, inflammation of the spermatic cord. There is an increase and redness of the corresponding half of the scrotum. This condition may be accompanied by an increase in body temperature.