Escherichia coli in urine or otherwise Escherichia Coli belongs to the group of opportunistic microorganisms and can normally exist in the human body. Its detection in urine in large quantities is a pathology. This is a sign of inflammatory diseases of the genitourinary system.
If it is detected once, it can be assumed that the rules for collecting urine for laboratory analysis were violated. Therefore, before taking any measures, you need to find out the reasons for its appearance in the urine. Parents of young children often face a similar situation.
Reasons for the presence of E. coli in urine
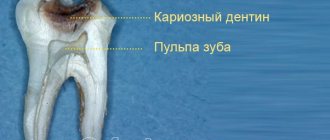
Escherichia coli is a gram-negative rod-shaped bacterium that is a representative of the normal microflora of the human gastrointestinal tract (GIT). In small quantities, it is harmless and even necessary for the human body, since it is involved in important processes.
It ensures the normal functioning of the gastrointestinal tract, promoting the digestion process. But if for one reason or another it penetrates and multiplies in an environment where it should not be, the normal functioning of individual organs and systems of the body is disrupted.
Very often this bacterium penetrates into the genitourinary system. Most often this is a consequence of violation of personal hygiene rules. In women, this occurs due to the peculiarities of the anatomical structure: the urethra and anus are located close to each other. This also occurs among representatives of non-traditional sexual orientation.
Escherichia coli is the causative agent of various diseases of the urinary organs, they are characterized by severe symptoms. The permissible amount of Escherichia Coli bacteria in urine is 105 mt/ml. If higher values are detected, it is recommended to repeat the analysis to exclude a false result or confirm the presence of pathology.
No ads 1
Escherichia coli lives in the lower intestine and can enter the genitourinary system under the following conditions:
- insufficient care of the genitals;
- promiscuity and unconventional sex;
- presence of sexually transmitted infections;
- chronic diseases of the genitourinary system.
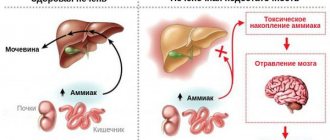
Pathological activation of E. coli occurs with decreased immunity and hormonal imbalance. Also, people suffering from diabetes are more susceptible to this. Escherichia coli is often detected in urine due to improper collection of material for analysis. In order to prevent the possibility of misdiagnosis, it is necessary to follow the rules for collecting urine.
First of all, you need to thoroughly rinse your urinary organs, and then your hands. If possible, the analysis should be collected in a sterile disposable container; it can be purchased at any pharmacy. If there is none, then the other container used must be thoroughly rinsed and dried. It is better to skip the first portion of urine.
Urine should not be stored for longer than 2–3 hours. If such a need arises, then you need to close the lid tightly and place the container in the refrigerator, but no more than 2 hours. If you need to collect urine for analysis from infants, then it is better to use a special urine collector, which can also be purchased at the pharmacy.
Violation of the rules of genital hygiene is a common cause of the penetration of E. coli into the genitourinary system
Bursitis
Vascular angiography is performed to determine the boundaries of the inflammatory process. Contrast arthrography is a diagnostic procedure during which a liquid contrast agent (urotrast, cardiotrast, diodone) is injected into the joint cavity, and then X-rays are taken.
If septic bursitis is suspected, aspiration of synovial fluid is performed for analysis using Gram staining and bacteriological culture.
Which doctors should I contact?
The diagnosis and treatment of bursitis is carried out by a doctor - an orthopedic traumatologist or (for purulent bursitis).
Treatment of bursitis
Therapy for the disease must be comprehensive. It begins with ensuring the rest of the pathological joint, relieving swelling and pain. To do this, it is necessary to reduce or completely eliminate movements in the affected joint and minimize the load. For this purpose, orthoses, bandages and other fixing orthopedic devices are used.
Cold compresses reduce swelling and inflammation. Compression bandaging (squeezing the joint with elastic bands or other devices) reduces pain. Traditionally, drug treatment for bursitis begins with the prescription of non-steroidal anti-inflammatory drugs, which help to quickly relieve inflammation and reduce pain. Chondroprotectors are used to restore joint tissue. Antibiotics are prescribed only for bacterial inflammation of the periarticular bursa.
Modern methods of treating acute bursitis include intra-articular injections with glucocorticosteroids. This allows you to reduce the risk of relapse of the disease and quickly relieve pain, reduce swelling of the synovial membrane of the bursa.
Corticosteroid injections are not recommended for septic bursitis.
In addition, to reduce the severity of pain, swelling and accelerate the regeneration of damaged joint tissues, local remedies are used:
- compresses with dimexide, which have a strong absorbable effect;
- ointments with chondroitin sulfate, glucosamine, and collagen;
- ointments with non-steroidal anti-inflammatory components.
In case of septic bursitis, the inflamed bursa is opened and drained, the pus is pumped out and the joint cavity is washed with antibiotics and antiseptics.
Repeat aspiration may be indicated if swelling, tenderness, and erythema persist. In some cases, the patient may be recommended intravenous antimicrobial therapy. In the subacute period, during the chronic course of the process, physiotherapy sessions are required (ultrasound, microcurrents, electro- and phonophoresis, UHF, dry heat, balneotherapy, paraffin therapy), which can effectively relieve local symptoms of bursitis.
Surgery to excise the bursa is a last resort and is used only in very advanced cases of the disease.
Complications
If inflammation develops near a joint, its mobility may be limited and subsequent muscle atrophy.
In most cases, the duration of the disease is limited to one to two weeks and does not pose a serious danger to human health. However, when an infection occurs, the risk of developing an inflammatory process increases, and serous inflammation quickly turns into purulent inflammation. The spread of the purulent process to surrounding tissues can occur as a phlegmonous inflammation with necrosis of the bursa wall and the formation of subcutaneous and intermuscular phlegmon. In advanced cases, long-term non-healing fistulas form.
The breakthrough of pus into the joint cavity leads to the development of purulent arthritis.
Complications can also develop as a result of untreated bursitis - such complications include scar adhesions, tendon rupture, salt deposition in the cavity of the synovial bursa, arthritis (inflammation of the joint), osteomyelitis (inflammation of the bone), sepsis (blood poisoning), complete immobility of the joint (contracture) .
Prevention of bursitis
Preventive measures are aimed at eliminating the causes and risk factors of bursitis:
- thorough cleansing of wound surfaces, treating the wound with antiseptics for cuts, scratches and abrasions;
- timely treatment of infectious and chronic diseases;
- eliminating the possibility of traumatic joint damage;
- moderate and varied physical activity;
- correct warm-up technique before training;
- fight against excess weight;
- prevention of possible injuries with the help of protective devices for joints - knee pads, bandages and others;
- unloading of joints in the presence of occupational risks (if you have to kneel for a long time, you must not forget about knee pads; when working at a computer, provide comfortable support for the forearm, etc.) and undergoing annual preventive examinations.
Sources:
- Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition, volume 3.
- Akhtyamova N.E. Modern approaches to the treatment of bursitis (recommendations for an outpatient surgeon) // RMZh. – 2021. – No. 3. – P. 193–196.
- Bursitis of the elbow joint. Clinical recommendations. All-Russian public organization Association of Traumatologists and Orthopedists of Russia. Moscow. 2021.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
What diseases does it cause?
With stable immunity in humans, E. coli may not manifest itself for a long time, being in the urinary tract. But over time, the patient develops certain unpleasant symptoms characteristic of the inflammatory process in the urinary system:
Severe pain in the lower abdomen in women
- frequent urge to urinate;
- lower abdominal pain;
- burning and discomfort when urinating;
- content of blood and pus in the urine;
- temperature increase;
- pain when urinating.
Most often, E. coli, having penetrated the bladder, causes cystitis and pyelonephritis. Almost half of all cases of pyelonephritis are diagnosed; the disease is caused by the bacterium Escherichia coli. Escherichia coli is detected in urine culture. The bacterium, having penetrated the urinary tract, attaches to the walls of the urethra.
This is dangerous due to the development of serious infectious pathologies such as chlamydia and urethritis.
In men, E. coli in the bladder indicates the development of prostatitis, epididymitis or orchitis. In women, Escherichia coli can cause endometritis, adnexitis, cystitis, and urethritis. Pathology can be suspected by the way urine acquires a sharp, unpleasant odor; women may experience discomfort during sexual intercourse; nagging pain appears in the lumbar and kidney areas. In men, potency decreases and prostate pain appears.
Pain with cystitis
Almost every woman has had cystitis at least once in her life.
Moreover, painful sensations are very characteristic of it.
When emptying the bladder, the patient experiences acute pain - as if she is being stabbed with a thousand sharp objects.
If urination occurs, a burning sensation is felt, a false urge to empty the bladder continues, discomfort in the lower third of the abdomen and pelvis.
Cystitis often occurs together with urethritis, since the urethra and bladder are affected.
Principles of treatment
If E. coli is detected in the urine, treatment involves changing the diet, taking medications and following preventive measures. Since E. coli causes diseases of the genitourinary system, table No. 7 is recommended for patients with such pathologies. It involves limiting protein and fluid intake.
According to this diet, dishes are best baked, boiled, stewed, or steamed. It is necessary to exclude salty, spicy and fried foods. Since Escherichia coli is a bacterium, antibacterial drugs are prescribed to destroy it. First, it is advisable to determine the sensitivity of the microflora by urine culture.
Before the test results are obtained, broad-spectrum antibacterial drugs are prescribed:
- macrolides;
- cephalosporins;
- carbapenems;
- penicillins.
To prevent imbalance of intestinal microflora and recurrence of the disease, along with antibiotics, it is necessary to take probiotics, eubiotics and prebiotics. During the treatment period, it is useful to include lactic acid products in the diet. If the disease is accompanied by pain, fever or deterioration in general health, the patient is prescribed non-steroidal anti-inflammatory drugs (NSAIDs).
These include Ibuprofen, Analgin, and Diclofenac. Depending on the severity and intensity of symptoms, these drugs are administered orally or intramuscularly as injections. Since E. coli in the urine often provokes the development of cystitis, antispasmodics are prescribed to treat this disease. They are used both in the form of tablets and as a solution for injections.
The basis for treating E. coli in urine is taking antibiotics
Uro-hyal for cystitis
Now we will talk a little about the new Russian drug Uro-hyal, which has proven its effectiveness in treating cystitis.
This solution contains hyaluronic acid, which lines the mucous membrane of the bladder with an elastic coating.
And you can treat cystitis without fear of damaging this wall during therapeutic action.
Uro-hyal is indicated for chronic recurrent cystitis, radiation and interstitial cystitis.
Prevention
Strict adherence to personal hygiene rules is the main way to prevent the penetration of E. coli into the urine. Underwear needs to be changed every day. Girls and women are not recommended to wear thongs. During menstrual bleeding, after childbirth and during pregnancy, it is important to maintain genital hygiene. Before washing, you need to wash your hands with soap.
In addition, to prevent the penetration of Escherichia coli into the urine, it is necessary:
- Healthy food;
- include fermented milk products in your daily diet;
- use of personal hygiene products;
- avoiding alcohol consumption;
- refrain from anal sex;
- use a condom when changing sexual partners.
During pregnancy, a woman is recommended to have a urine culture every 3 months. At this time, the risk of activation of pathogenic E. coli increases, as the body’s immune defense decreases. This measure will allow you not to miss inflammatory diseases of the genitourinary system.
Contagiousness of cystitis
Most often, as we have already discussed, infectious cystitis occurs from E. coli.
And such opportunistic microflora is not infectious to other people.
Sexual transmission of infection is not typical for cystitis.
But having unprotected sex can lead to cystitis or its relapse.
Exacerbations of cystitis are always accompanied by severe pain in the lower third of the abdomen, which serves as an obstacle to sex.
You cannot become infected with any form of cystitis directly from a person.
But by following certain rules of conduct in sexual life, you can avoid the causes that lead to cystitis.
It is necessary to be tested for STIs twice a year.
Regular sex and normal sexual activity increase your chances of not getting cystitis more than long periods of abstinence.
Timely treatment begins with a complete cure for cystitis.
And correct and regular adherence to preventive measures will help avoid recurrent cystitis.