Periodontal diseases are a series of pathologies accompanied by damage to the hard and soft tissues surrounding the teeth, which are inflammatory, idiopathic, dystrophic or neoplastic in nature. According to independent experts from the World Health Organization, inflammatory gum disease is diagnosed in 95% of the adult population of the planet. The prevalence of periodontopathies in Russia, depending on age, ranges from 48.2% (in children 10-12 years old) to 86.2% (in 44 years old), and by the age of 65 it reaches 100%. The most common disease found in adolescents is gingivitis, and in older people - periodontitis. If not treated in a timely manner, periodontopathy can cause tooth loss and the development of purulent-inflammatory pathologies of the maxillofacial area.
WHAT IS PERIODONTAL
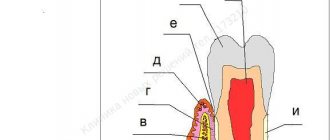
The periodontium is the complex of tissues surrounding the tooth. These include not only the gums, but also the bone socket in which the tooth root is located, and the tooth ligaments that hold the tooth in the socket, intertwined with the tooth root and bone. All these tissues represent a single system that performs several important functions at once: fixation of teeth, perception and regulation of chewing load, control of the work of masticatory muscles, protection against penetration of pathogenic bacteria and a number of damaging factors into the bone tissue.
HOW DOES GINGIVIT MANIFEST, AND WHY DOES IT OCCUR?
With superficial inflammation of the gums (if only soft gum tissue is involved in the process), we are dealing with gingivitis. Inflammation can occur in the area of 1 - 2 teeth (local gingivitis) or all teeth (generalized gingivitis).
Inflammation of the gums usually begins with damage to the gums, for example, when eating, brushing teeth, an incorrectly applied filling or crown, or a chemical burn. In this case, pathogenic microorganisms penetrate the injured gum and intensify the inflammatory response. The presence of soft plaque, tartar, and poor oral hygiene are mandatory conditions, and very often an independent cause of the onset and maintenance of the disease.
Gingivitis is often observed in people with malocclusions, crowded teeth and their incorrect position. A short frenulum of the upper and lower lips is also a risk factor for periodontal disease.
Smoking plays an important role (spasm of blood vessels occurs, gum nutrition deteriorates), decreased body defenses (immunodeficiency), lack of vitamin C and other risk factors.
In the acute stage of the process, pain, burning, swelling of the gingival margin, and bleeding when brushing teeth are usually noted. If the cause of the disease is not eliminated, then acute gingivitis becomes chronic, which does not go away on its own without treatment. In this case, the gums turn blue and periodically bleed when brushing your teeth and eating. There is an unpleasant odor from the mouth.
Severe forms of gingivitis, such as ulcerative gingivitis, are observed in severe general diseases of the body. For example, with diabetes or a serious immunodeficiency disease. In this case, the temperature rises, painful ulcers covered with a film appear on the dirty gray gums, and general health worsens.
With gingivitis, the teeth remain stable, since the process does not penetrate deep into the periodontium, the so-called periodontal pocket does not form, and the bone tissue of the tooth socket does not dissolve. Can there be consequences if gingivitis is not treated?
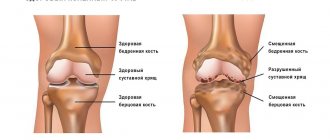
If gums are not treated in time, gingivitis will develop into periodontitis. This is a much more serious and dangerous disease than gingivitis. Often it becomes irreversible, since periodontitis affects and destroys the deep tissues of the periodontium - the ligaments of the tooth and the bone tissue of the jaw.
Gingivitis
This is a superficial inflammation of the gum, without disturbing its attachment to the tooth. The ligamentous apparatus of the tooth is not destroyed, and when negative factors are eliminated, everything returns to normal.
Causes of gingivitis
The main cause is soft plaque that forms on the teeth and between the teeth after eating. Microorganisms settle in plaque. The accumulation of microbes and their metabolic products in the gingival sulcus area leads to gum inflammation.
Symptoms of gingivitis:
- bleeding gums when brushing and eating solid foods;
- smell from the mouth;
- itching, burning in the gums;
- swelling and redness of the gums;
- when taking certain medications, during orthodontic treatment.
Types of gingivitis:
- catarrhal;
- ulcerative-necrotic (characteristic is the appearance of painful ulcers on the gums, covered with a white coating);
- hypertrophic (characterized by gum growth and the formation of false gum pockets) is more common in children and pregnant women.
Regardless of the type, inflammatory processes do not affect dental tissues or destroy teeth, so it is relatively easy to defeat the disease. It is important to pay attention to gingivitis in time, otherwise this gum disease threatens periodontitis.
Treatment of gingivitis comes down to professional oral hygiene. It includes: removal of dental plaque; polishing roots and teeth with polishing pastes; If necessary, anti-inflammatory therapy is carried out. Then, teeth and gum care products are selected and training is provided on the rules of brushing teeth and gums.
WHAT FACTORS PROMOTE THE DEVELOPMENT OF PERIODONTITIS?
The causes of periodontitis are the same as those of gingivitis. Often periodontitis is associated with chronic gingivitis. If the traumatic factor persists, microorganisms actively continue to multiply in the damaged gum. Their toxins and enzymes destroy the gums deeper and deeper.
As a result, the connection between the gum and the tooth (the bottom of the periodontal sulcus) is disrupted - a very important protective formation that protects the tooth ligaments and bone from infection. A periodontal pocket appears, and now bacteria, plaque, etc. rush into the depths of the periodontium - this is where periodontitis begins. Next, gradual destruction of the tooth ligaments occurs, and the bone tissue melts.
Periodontitis can be acute or chronic. Typically, acute periodontitis occurs when there is deep, strong trauma to the gums (for example, a long artificial crown, a toothpick). In this case, the periodontal connection may be immediately disrupted - gingivitis and periodontitis occur simultaneously.
Generalized periodontitis is characteristic of serious general diseases of the body - diabetes, other endocrine diseases, radiation sickness, severe diseases of the gastrointestinal tract and cardiovascular system. It is almost impossible to cure such periodontitis without general treatment of the underlying disease.
In the chronic process, pain and swelling are not as pronounced as in acute periodontitis, the amount of tartar and soft plaque increases, the bad breath increases, the gums begin to settle, exposing the neck of the tooth, teeth become sensitive to cold, hot, sour and salty. Tooth mobility appears, unnoticeable at first, but steadily increasing.
Suppuration of periodontal pockets is often observed. Pus is released from under the gum when pressing on the gum edge with a finger. Sometimes, in the absence of outflow of pus, periodontal microabscesses occur - in this case, the patient already requires surgery.
Periodontitis can be one of the causes of some common diseases. The microorganism that causes stomach ulcers is often found in dental plaque. Other bacteria living in dental plaque can lead to the formation of microthrombi (blood clots). Penetrating into the blood (with bleeding gums), they increase the risk of cardiovascular diseases, including myocardial infarction. The entry of microorganisms into the blood can lead to septic endocarditis. There is information about the relationship between chronic dental and periodontal diseases and kidney damage. Remember that the focus of chronic infection in the oral cavity is the entry point for pathogenic bacteria into the body.
Systemic diseases associated with loss of supporting periodontal tissues16,21
The new classification of periodontal diseases also includes systemic diseases and conditions that affect the supporting tissues of the periodontium.16 It is known that there are rare systemic disorders, such as Papillon-Lefevre syndrome, that usually lead to the early presentation of severe periodontitis. Such conditions are grouped as “periodontitis as a manifestation of systemic disease,” and the classification should be based on the underlying systemic disease.16 Other systemic conditions, such as neoplastic diseases, may affect the periodontal system independent of plaque-induced periodontitis,21 such clinical findings should also be classified based on the primary systemic disease and grouped as “Systemic diseases or conditions affecting the supporting periodontal tissues.” However, there are common systemic diseases, such as uncontrolled diabetes mellitus, with variable effects that modify the course of periodontitis. They appear to be part of the multifactorial nature of complex diseases such as periodontitis, and are included in the new clinical classification of periodontitis as an identifier in determining stage and category.20 Although common modifiers of periodontitis can significantly alter disease manifestation, severity, and response to treatment, modern data do not support a unique pathophysiology in patients with diabetes and periodontitis.22
DIFFERENCES PERIODONTOSIS FROM PERIODONTITIS
Periodontal disease is a degenerative lesion of all periodontal tissues; this process never occurs in an acute form and is not associated with exposure to bacteria. There is a slow, uniform resorption of the bone tissue of the teeth cells and subsidence of the gums with exposure of the roots of the teeth. Periodontal disease is always a generalized process, that is, all teeth on both jaws are affected. Bone tissue atrophy is usually painless, continuous and, if left untreated, leads to the complete disappearance of the ligamentous apparatus, the walls of the tooth sockets and their loss. Inflammatory phenomena are associated with periodontal disease quite rarely.
The exact cause of the disease is still unknown. It is believed that the onset of the disease is associated with impaired blood circulation in periodontal tissues and endocrine disorders. The development of periodontal disease is promoted by diabetes, cirrhosis of the liver, gastric ulcer, neurogenic diseases, cardiovascular pathology (atherosclerosis), hypovitaminosis and a decrease in the body's overall resistance.
Local factors, for example, the impact of microorganisms on the periodontium, can only aggravate the course of the disease, therefore, in periodontal disease, the primary process is the resorption of bone tissue and the ligamentous apparatus of the tooth, and superficial changes in the gums are secondary.
Periodontal disease progresses slowly. Clinically, it manifests itself with significant changes in the periodontium. This is subsidence of the gums, exposure and increased sensitivity of the necks of the teeth, itching in the gums. Teeth remain stable for quite a long time.
A characteristic sign of periodontal disease is the presence of so-called wedge-shaped tooth defects - damage to the enamel of the teeth near the gums in the form of fairly deep oval cavities. Currently, this phenomenon is explained by a malnutrition of the tooth, inferior enamel and dentin, combined with very strong pressure on the toothbrush during frequent brushing. Periodontal disease is characterized by the absence of periodontal pockets.
New classification of periodontitis
The 1989 workshop recognized that periodontitis has several distinct clinical presentations, varying ages of onset, and rates of progression.7,8 Based on these variables, workshop participants classified periodontitis as prepubertal, juvenile (localized and generalized), adult periodontitis, and rapidly progressive. A 1993 European workshop determined that the classification should be simplified and proposed dividing periodontitis into two main areas: adult periodontitis and early-onset periodontitis.9 Participants at the 1996 workshop decided that there was insufficient new evidence to change the classification.10 Important changes to the classification of periodontitis were made in 1999,11-13 which has been used for the last 19 years. Periodontitis has been classified as chronic, aggressive (localized and generalized), necrotizing, and as a manifestation of systemic disease.
Since the 1999 workshop, much new information has emerged from population-based studies, basic science studies, and prospective studies assessing environmental and systemic risk factors. Analysis of these data prompted the 2021 workshop to develop a new classification system for periodontitis.14
Over the past 30 years, the classification of periodontitis has been changed several times in an attempt to bring it into line with new scientific data. The seminar participants agreed that, according to modern knowledge in the field of pathophysiology, three forms of periodontitis can be distinguished: necrotizing periodontitis
15
periodontitis is a manifestation of systemic disease
, 16 and forms of the disease previously defined as “chronic” or “aggressive” are now grouped under one category, “periodontitis.” 14,17–20 In revising the classification, the workshop agreed on the classification of periodontitis , supplemented by a multifaceted staging and scoring system that can be adapted over time as new evidence becomes available.20
Determination of the stage of the disease depends largely on its severity at the time of consideration, as well as on the complexity of disease management, while the classification provides additional information about the biological features of the disease, including anamnesis-based analysis of the rate of disease progression, assessment of the risk of further progression, expected adverse effects. treatment outcomes and an assessment of the likelihood that the disease or its treatment will adversely affect the patient's overall health.14,20 There are four categories (stages 1 to 4) and are determined by several variables, including clinical attachment loss, number, and percentage bone loss, probing depth, presence and degree of angular bone defects, furcation lesions, tooth mobility and tooth loss due to periodontitis. The assessment includes three levels (A - low risk, B - moderate risk, C - high risk of progression) and includes, in addition to aspects related to the progression of periodontitis, general health and other influences such as smoking or level of metabolic control in diabetes. Thus, the classification allows the clinician to include individual patient factors in the diagnosis, which are critical for comprehensive case management (Table 3). For a complete description of the new classification, please refer to the consensus report on periodontitis14 and the document defining periodontitis.20
Table 3.
| Periodontitis: a consensus report Papapanou, Sanz et al. 2018 | Determination of the stage and severity of periodontitis: structure and proposals for a new classification, definitions Tonetti, Greenwell, Kornman. 2018 |
Forms of periodontitis
1. Necrotic periodontal diseases
Herrera et al. 2018
a. Necrotizing gingivitis
b. Necrotizing periodontitis
c. Necrotizing stomatitis
2. Periodontitis as a manifestation of systemic diseases
Jepsen, Caton et al. 2021 Albandar et al. 2018
The classification of these conditions is based on the underlying systemic disease according to International Classification of Diseases (ICD) codes.
3. Periodontitis
Fine
et al. 2021 Needleman et al. 2021 Billings et al. 2018
a. Stages: based on severity of disease1 and complexity of treatment2
I degree: initial periodontitis
II degree: moderate periodontitis
III degree: severe periodontitis with possible tooth loss
IV degree: severe periodontitis with possible loss of dentition
b. Scope and distribution3: localized; generalized; affecting molars and incisors
c. Categories: based on risk of rapid progression4, expected response to treatment5
1) Category A: low development rate
2) Category B: medium development rate
3) Category C: high speed of development
1Severity: interproximal attachment loss at the site of greatest loss; X-ray bone loss and missing teeth
2 Treatment complexity: probing depth, type of bone destruction, furcation lesions, number of remaining teeth, tooth mobility, bone crest defects, masticatory dysfunction
3Attached to the stage as an identifier: localized - less than 30% of teeth, generalized - more than 30% of teeth
4Risk of progression: direct evidence from radiographs or attachment loss, or indirect from the relationship of bone loss to patient age
5Expected response to treatment: phenotype, smoking, hyperglycemia
WHY IS PLAQUE A MAIN CAUSE OF PERIODONTAL DISEASE?
Bacterial plaque is a sticky, colorless film that constantly forms on teeth. If plaque is not removed, it will harden and form a rough, porous growth called tartar. Bacteria in tartar produce toxins (poisons) that irritate the gums, causing them to become red, tender, swollen, and bleeding. As the disease progresses, toxins can lead to periodontal destruction and the formation of pockets that fill with plaque. The bone that supports the teeth is subject to constant destruction. Consistently removing plaque through brushing, flossing, and professional care can minimize the risk of gum disease. However, if no treatment is given, the affected teeth may become loose and eventually fall out.
WHAT IS A PERIODONTAL EXAMINATION?
The history of the disease (anamnesis) is carefully determined. When did it first start, what was done for treatment, do parents and close relatives have this disease, etc. Careful collection of data makes it possible to determine risk factors and sometimes even predict the course of the disease. This is followed by a careful examination of the oral cavity: the frenulum of the lips and tongue, the dental arches as a whole and, if necessary, each tooth separately, as well as fillings, crowns and orthodontic appliances are assessed.
One of the main examination methods is probing the periodontal pocket of each tooth at six points. The presence of tartar and soft plaque, bleeding, suppuration, tooth mobility, etc. is assessed. This labor-intensive analysis is painlessly performed in 15 - 20 minutes using a special electronic probe of the automated computer clinical diagnostic system Florida Probe (USA). The patient’s personal data is stored in the computer’s memory, which makes it possible to predict the course of the process and select treatment, as well as evaluate the dynamics of the disease and the effectiveness of the treatment.
An orthopantomogram is a necessary element in the diagnosis of periodontal diseases. This image shows the teeth, jaw bones, and the partitions between the teeth. Digital orthopantomographs (such as the ones in our clinic) allow you to obtain excellent images with minimal radiation exposure to the patient and evaluate them on a computer screen using auxiliary computer programs.
WHAT IS MEAN BY PERIODONTAL TREATMENT
After collecting all the necessary information, the periodontist will discuss the condition of your gums with you and suggest the most optimal treatment. Most importantly, it must be comprehensive - that is, treatment must cover all identified causes and associated factors that support the disease. Only in this case can it be possible to completely cure or stabilize periodontal disease for a long time.
Treatment will be much more effective if the patient strictly follows all instructions and strictly follows the chosen treatment plan.
Typically, a comprehensive treatment plan consists of general and local treatment and includes all or part of the methods listed below.
ELIMINATING TRAUMATORY FACTORS DURING TREATMENT
Treatment begins with the elimination of traumatic factors - low-quality fillings and crowns with an overhanging or very deeply embedded edge in the gum, bridges, traumatic teeth, etc. are removed.
The so-called selective grinding of teeth is carried out in order to eliminate excessive traumatic load when chewing from overloaded teeth. At the same time, small areas of the teeth are slightly undermined, which do not allow the upper and lower rows of teeth to meet correctly, thereby causing them to be overloaded.
This is an absolutely harmless procedure, since the ground areas of the teeth are polished and coated with fluoride preparations. In this case, caries does not occur.
Professional oral hygiene The next stage of treatment (performed in 100% of cases) is professional teeth cleaning: it allows you to remove even tartar located deep under the gum (this is the strongest traumatic factor). In addition to tartar and soft plaque, dense dark plaque (from smoking, drinking tea, coffee, and other dyes) is simultaneously removed - this allows you to restore the beautiful appearance of your teeth. After removing tartar and plaque, the doctor will definitely polish the cleaned surface of the root and crown of the tooth.
Nowadays, several methods of removing dental plaque are common. Cleaning teeth with a stream of air mixed with cleansing powder and water (the most famous representative is the Air Flow system) perfectly cleanses teeth of soft plaque, dark plaque from tobacco or coffee, even in hard-to-reach places. Ultrasonic scalers are capable of removing tartar of almost any size.
Removing tartar is one of the most important and effective stages in the treatment of periodontal diseases.
Anti-inflammatory therapy Drug therapy of gums allows you to relieve inflammation - cope with pain, swelling, and reduce bleeding gums. Typically, periodontal pockets are washed with antiseptic solutions (chlorhexidine, iodinol, etc.), and various medicinal substances are used (enzymes, antimicrobial, hormonal, anti-inflammatory drugs). Often the gums are covered with a special bandage after the medication is administered.
Self-absorbing Diplen-Dent films impregnated with various medications (antibacterial, improving blood circulation, etc.) are very convenient. Such films are glued by the patient independently to the affected areas of the gums (for example, before going to bed) and, gradually dissolving, release the medicine directly into the gums. In the morning, all you have to do is remove the remaining film from the oral cavity.
Physiotherapeutic treatment There are many methods of physiotherapeutic treatment of periodontal diseases. Laser therapy is most widely used in our clinic. Therapeutic laser radiation has a very wide range of therapeutic effects - relieves pain, improves blood circulation, metabolism, stimulates immune defense.
Gum massage can be performed by a doctor or independently. At home, use your index finger to massage the area of the interdental papilla of the gum with up and down movements (6 to 10 movements per papilla). The massage ends with hygienic rinses. Massage should not be used if the disease is exacerbating or if there are erosions or ulcers on the gums.
Surgical treatment Periodontal surgery is a radical and one of the most effective methods of treating moderate and severe periodontitis. With the help of small operations, it is possible to eliminate periodontal pockets, remove overgrown infected soft tissues, eliminate suppuration of the gums (microabscesses), replant bone tissue or bone substitutes, lift receding gums and close small root exposures.
Every year new developments in the field of surgical treatment, modern materials and treatment methods appear. One of the promising innovations is surgical treatment using cellular technologies, which allows stimulating the restoration of bone tissue. This technology is widely used in our clinic. Surgical treatment is always carried out after removal of dental plaque and therapeutic treatment, when all acute symptoms of gum inflammation subside. All interventions are performed under local anesthesia and rarely take much time. Usually all postoperative phenomena subside after 2 - 3 days, and the sutures are removed, or they dissolve within a week.
The effect of such operations often lasts for a long time. A lot will depend on maintaining oral hygiene, following preventative rules and overall health.
Rational prosthetics and splinting Prosthetics of missing teeth and their permanent splinting (i.e. joining teeth together using a prosthesis or special light-curing threads) are the final stage of the treatment of periodontal diseases. It allows you to fully restore the function of chewing, eliminate aesthetic defects (in the absence of teeth visible when smiling), and unite all the teeth together, as intended by nature.
In this case, the load is distributed evenly throughout the entire dentition, which allows the supporting teeth to function much longer. Even the absence of one tooth causes a number of changes in the bone tissue of the jaw. If, after successful therapeutic and surgical treatment of the gums, rational prosthetics and splinting are not carried out, then the disease may worsen again in the very near future.
Prosthetics are carried out using both removable and fixed dentures, depending on the condition and number of teeth.
After completion of treatment, we advise you to strictly follow all the doctor’s recommendations. Be sure to visit your doctor at least 1-2 times a year for a follow-up examination and professional oral hygiene.
Therapy of periodontal pathologies
The treatment regimen is individual and depends on the characteristics of the clinical course and the severity of the pathology. As part of complex therapy, therapeutic, surgical, orthodontic and orthopedic treatment is usually carried out. Therapeutic treatment includes professional cleaning, treatment of gum pockets, anti-inflammatory and antimicrobial therapy. Surgical treatment includes various types of curettage, gingivectotomy, curettage of the pathological lesion with the introduction of osteogenic materials. Dental units with a high degree of mobility must be removed. Effective orthopedic methods for gum disease are splinting and selective grinding. Splints tighten movable dental units and fix them in the desired position, which avoids their premature loss. To improve blood supply and tissue regeneration, physiotherapeutic procedures are widely used - vacuum and hydrotherapy, electrophoresis.
One of the modern methods of periodontal treatment is the use of the Vector ultrasonic unit, designed to remove subgingival dental plaque and polish the root surface. The device is an innovative development of German scientists and is currently successfully used in many modern dental clinics. The operating principle is based on the use of ultrasonic waves. The destruction of the attachment of plaque and tartar to the root surface occurs due to the effect of ultrasonic cavitation. Ultrasonic waves are supplied with a special solution containing microparticles of calcium hydroxyapatite. This significantly improves the degree of teeth cleansing and reduces tissue sensitivity. The “Vector” device contactlessly removes dental plaque and at the same time has a positive effect on periodontal tissue: interstitial metabolism is restored, cells are saturated with nutrients, and tissue resistance to infectious and inflammatory processes increases. Treatment of periodontitis with the Vector device is relatively painless. As a rule, anesthesia is not required, but in case of increased sensitivity, patients can be given local anesthesia in the form of a gel that is applied to the gums. The effectiveness of treatment is evidenced by the regeneration of periodontal tissue and the achievement of a long-term state of remission.
HOW MUCH WILL THE TREATMENT COST?
The cost of periodontal treatment will depend on the type and amount of work planned. When considering an investment in your own health, consider that treating gum disease is cheaper and better for your health than restoring a tooth lost due to untreated periodontal disease.
New direction – aesthetic surgical periodontology
Recently, such a direction as aesthetic surgical periodontics has appeared and is actively used in surgical periodontology. She deals with the correction of changes in the position of the gingival margin relative to the neck of the tooth, and gum growths. Aesthetic surgical periodontics includes a large number of new surgical techniques, depending on the clinical situation and the desired aesthetic effect.
Who treats periodontal problems?
A periodontist treats diseases of the periodontium and oral mucosa. A periodontist knows all diseases of the oral cavity and treats the root system of teeth, periodontium, and sockets. Close collaboration between your primary care dentist and your periodontist will bring the most positive results.
The portal will allow you to find patient reviews about their treating doctors, which will help you choose the best specialist. The advantages of searching for a specialist on the portal: you see the rating of the doctor and the clinic, each clinic has specialists in different fields, which is important when treating periodontal disease. By going to the clinic’s website, you can find out the hardware and technical capabilities, and compare prices for the services provided.
ARE THERE METHODS FOR PREVENTION OF PERIODONTAL DISEASES?
- Prevention of periodontal disease consists of several simple points:
- Brush your teeth 2 times (morning and evening) after meals. Use a toothpaste recommended by your doctor to protect your gums. Use an electric toothbrush - it perfectly cleans your teeth and massages your gums.
- Do professional oral hygiene at least 2 times a year, and at the same time you can undergo an examination by a periodontist. Do not use any medications for the treatment or prevention of periodontal disease (gels, ointments, tablets, etc.) without consulting your dentist.
- Do not eat only soft and delicate foods - your teeth should receive normal, natural stress.
- Your diet should be well balanced, contain the required amount of proteins, fats, carbohydrates, and vitamins. If you are deficient in vitamins, take multivitamin complexes.
- Lead a healthy lifestyle.