Content
- Causes of inflammation of hemorrhoids in pregnant women
- What to do for hemorrhoids during pregnancy?
- Action plan when planning pregnancy
- A case from the practice of a proctologist
- Removal of hemorrhoids with laser
Hemorrhoids often develop during pregnancy and childbirth. In some cases, it also becomes inflamed. Sometimes the inflammation is very significant and is accompanied by severe pain. The duration of exacerbation of hemorrhoidal disease during pregnancy is from 1-2 weeks to several months. It happens that hemorrhoids begin at 5-6 months and bother you until the end of pregnancy.
If hemorrhoids become inflamed during pregnancy, then after childbirth there is almost always an exacerbation of hemorrhoidal disease.
How long can hemorrhoids bother you after childbirth? Very different: from 1 week to several months, until the woman consults a proctologist. Most often, surgery is not possible in this case.
Treatment of hemorrhoids in pregnant women and the postpartum period
It is important to remember that prevention of hemorrhoids is the most effective method of preventing the development of complications!
First of all, it is necessary to normalize the frequency and nature of stool. To do this, you need to remember the following rules:
- Drink 2-2.5 liters of fluid daily (if there are no contraindications);
- Follow a diet high in dietary fiber (fiber): boiled broccoli, baked apple, baked pumpkin, etc.;
- Do not spend a lot of time on the toilet, as this is a predisposing factor to thrombosis of hemorrhoids;
- Don't use toilet paper - use a bidet or hygienic shower;
- Lead a physically active lifestyle.
If thrombosis of hemorrhoids occurs, to the above recommendations you should add sitz baths with a solution of chamomile or a weak solution of potassium permanganate (2-4 minutes) and applying Hepatrombin-G ointment to the hemorrhoids for 7-10 days to relieve thrombosis and reduce pain.
In all cases of hemorrhoid symptoms, you should consult a coloproctologist.
What to do for hemorrhoids during pregnancy?
Extensive experience in proctology (about 20 years) and the use of lasers (5 years) allowed us to develop treatment tactics that allow us to preserve and improve the health of our patients.
Necessarily! Just as you have the courage to go to a gynecologist before planning a pregnancy, also go to a proctologist.
We must clearly remember that during pregnancy, no matter how much hemorrhoids bother you, they can only be treated conservatively: ointments, suppositories, laxatives. Recently, people have been trying not to prescribe venotonic tablets. There is evidence that these drugs have an adverse effect on the fetus.
Health care plan for expectant mothers regarding hemorrhoidal disease
- You are 18-25 years old , planning your FIRST pregnancy , your butt has never bothered you (there were no inflammations or painful nodes in the anus, no pain during bowel movements, no blood in your stool) - most often you don’t need to go to a proctologist. If you are worried about not knowing, come, we will conduct an examination and find out if there are hidden, asymptomatic problems.
- You are 18-25 years old , planning a SECOND pregnancy , your butt has never bothered you, including during your first pregnancy and after childbirth - go to a proctologist. 50-70% of patients have hemorrhoids, often small. During the second pregnancy, the probability of inflammation of the nodes is more than 50%, after childbirth - even more!
- You are 18-25 , planning your FIRST pregnancy , you have already had problems before: inflamed nodes, pain during bowel movements, bleeding - you MUST go to a proctologist.
During pregnancy, the probability of inflammation of the nodes is more than 50%. After childbirth, almost everyone experiences a severe exacerbation. - Girls over 25 years old when planning their FIRST pregnancy , even if the butt has never bothered you, go to a proctologist. Why? Nowadays a huge number of young people study or work SITTING. Your fitness 3 times a week for 1-2 hours does not compensate for 8-10 hours of daily sitting. Previously, hemorrhoids were a driver's disease, but now they have become a disease of office workers, students and even schoolchildren. This happens, no need to be surprised.
My head can’t contain all the stories that I heard, when everything was fine (well, or a little not good, but not much), and at 6-7 months of pregnancy it became bad - the nodes became inflamed and “I didn’t know, I don’t care.” They said that we need to go to the proctologist!” NOW YOU KNOW!
After the FIRST and even more so after the SECOND birth, there will almost always be dilatation of the veins of the external hemorrhoidal plexuses. They may not become inflamed yet, but this, alas, is temporary. During pregnancy, inflammation is very likely.
Hemorrhoids - varicose veins in the anus, caused by hyperplasia of the cavernous bodies of the rectum, are the most common proctological disease. It is believed to affect more than 10% of the population aged 30 to 50 years. According to various authors [1, 2, 14], hemorrhoids occupy one of the first places in coloproctology, and its prevalence is high and amounts to 140-180 people per 1000 adults.
In women, hemorrhoids appear or worsen mainly during pregnancy and childbirth. According to statistics, hemorrhoids are 5 times less common in nulliparous women than in women who have given birth at least once. In this case, the age criterion also plays an important role: during pregnancy at 30 years of age, the disease occurs 3 times more often than during pregnancy at 20 years of age. According to N.V. Moon et al. [5], hemorrhoids occur in 7.7% of non-pregnant women, 25.7% of pregnant women and 49.8% of postpartum women. Pregnancy, although not the main pathogenetic factor of hemorrhoids, often reveals it and aggravates its clinical course. On the other hand, hemorrhoids in pregnant women often complicate the course of labor and the postpartum period [1, 10, 11].
The views of researchers on the etiology of this disease are very contradictory. If Hippocrates attributed the cause of hemorrhoids to bile and mucus, then in subsequent centuries many different theories were put forward and disputed. Congenital insufficiency of the venous system, venous congestion, and disruption of the mechanism of the rectal sphincter were mentioned as the main pathogenetic factor. At the same time, none of the hypotheses based on the pathology of the venous system could explain the origin of the main symptom characteristic of hemorrhoids - the discharge of scarlet blood. The answer to this question was given relatively recently, in 1963, when cavernous vascular plexuses were discovered located in the submucosal layer of the caudal part of the rectum. Cavernous bodies are located in the area of the base of the anal columns diffusely or, more often, grouped mainly in three zones: on the left lateral, right anterolateral and right posterolateral walls of the anal canal. It is in these areas that hemorrhoids most often subsequently form. It has been proven that, in addition to veins and arteries, these vascular formations contain elastic connective tissue and smooth muscle cells. By regulating blood flow in the anal canal area, hemorrhoidal plexuses provide the basic functions of the rectum: retaining feces and defecation, providing an effective immune barrier between the internal environment of the body and the outside world. A hemorrhoid is a hyperplastic change in the cavernous tissue of the rectum, caused by an increased influx of arterial blood into the cavernous bodies through arteries with obstructed outflow through the efferent venules. The development of dystrophic processes in the anatomical structures that form the fibromuscular framework of internal hemorrhoids contributes to their gradual displacement in the distal direction [6, 19].
A major role in the development of hemorrhoids is played by impaired blood outflow through the venules from hyperplastic cavernous bodies of the distal rectum and anus. These cavernous bodies are present normally and are formed at the 3-8th week of embryonic development and are located in the area of the base of the Morganian columns. Cavernous bodies differ from ordinary veins of the submucosal layer of the rectum in the abundance of direct arteriovenous anastomoses. This is precisely the explanation for the fact that in hemorrhoids bleeding is arterial in nature. Hemorrhoids usually occur in individuals with pronounced groups of cavernous bodies. Other factors in the occurrence of hemorrhoids are congenital functional deficiency of connective tissue, impaired nervous regulation of the tone of the venous wall, increased venous pressure due to constipation, prolonged work in a standing or sitting position, heavy physical labor, and pregnancy.
The main pathogenetic factors in the development of venous pathology during pregnancy are:
- dishormonal changes;
— functional state of the vein walls;
- increase in circulating blood volume;
- changes in the blood coagulation and anticoagulation systems;
- increased intra-abdominal pressure.
A certain role in the occurrence of hemorrhoids is attributed to the abuse of alcohol and spicy foods, as a result of which the arterial flow to the cavernous bodies of the rectum increases. With prolonged exposure to unfavorable factors, along with predisposing factors, hyperplasia of the cavernous bodies occurs and the hemorrhoidal node itself is formed [4, 10, 12].
There are internal hemorrhoids, located above the pectineal line under the mucous membrane of the rectum, and external, located below the pectineal line under the skin. Approximately 40% of patients have a combination of external and internal hemorrhoids - mixed hemorrhoids. External hemorrhoids are observed infrequently - in less than 10% of patients [3, 7, 20].
With external hemorrhoids, the nodes are localized on the outside, and they should not be confused with prolapsed internal hemorrhoids. Most often, external nodes manifest as thrombosis. As a rule, bleeding from external nodes does not occur, since they are not injured during defecation. But constant stagnation of blood in them can lead to the formation of blood clots in them. Externally, the external hemorrhoidal node can be of different sizes, from 3 mm or more, which depends on its blood supply. An external hemorrhoid is usually covered by skin, while a prolapsed internal hemorrhoid is usually covered by the mucous membrane of the anal canal.
With internal hemorrhoids, there are varicose hemorrhoidal veins, which are located deep in the anal canal, so such hemorrhoids are not visible during a normal examination. In order to see them, you have to resort to special research methods: anoscopy, rectoscopy. Also, such nodes can be identified during digital rectal examination.
There are three degrees of internal hemorrhoids:
1st degree - hemorrhoidal veins are located in the anal canal, may not be palpable, cause subjective complaints by maintaining inflammation or causing bleeding.
2nd degree - nodes protrude from the anus when straining and disappear on their own.
The 3rd degree is characterized by prolapse of hemorrhoids that cannot be reduced on their own.
Hemorrhoids can occur acutely or chronically, but essentially these are phases of the same process. In acute hemorrhoids, inflammation occurs in the nodes, which, in addition to other symptoms, leads to severe pain in the anus. Spasm of the rectal sphincter increases swelling, leads to stagnation of blood in the lower rectal plexus and thrombosis of external hemorrhoids. In some cases, acute inflammation is accompanied by swelling of the perianal area and necrosis of the nodes. The often occurring tissue swelling and inflammatory infiltration create the impression of pinched hemorrhoids [2, 21].
The acute course of hemorrhoids is divided into three stages:
Stage I is characterized by thrombosis of hemorrhoids without inflammation.
Stage II is characterized by the addition of inflammation.
Stage III is characterized by widespread thrombosis of external and internal hemorrhoids with inflammation of the subcutaneous tissue, swelling of the skin of the perianal area, necrosis of the mucous membrane of the hemorrhoids.
During chronic hemorrhoids there are four stages:
In stage I, minor changes are noted in the ligamentous apparatus of the rectum, which is responsible for holding hemorrhoids in the anal canal, i.e. There was no prolapse of hemorrhoids.
In stage II, changes in the ligamentous apparatus of the rectum are expressed to such an extent that prolapse of hemorrhoids is noted during the act of defecation, but they themselves are reduced into the anal canal. In this case, bleeding may or may not be observed.
Stage III is characterized by such changes in the rectum that the prolapsed nodes no longer correct themselves, and the patient is forced to reset them himself after each act of defecation.
In stage IV, there is already a constant prolapse of hemorrhoids, and it is almost impossible to set them back. This is due to pronounced changes in the ligamentous apparatus of the rectum.
With chronic hemorrhoids, scarlet blood is released during bowel movements, prolapse of hemorrhoids, dull, incessant pain in the anus, and itching. A typical symptom complex of the chronic course of the disease consists of repeated bleeding, usually associated with defecation and prolapse of hemorrhoids from the anus. Bleeding as the leading symptom of hemorrhoids is observed in more than half of patients. Continuous bleeding from the anal canal is a complication of the disease. Prolonged bleeding from hemorrhoids leads to anemia. The second most common symptom characteristic of hemorrhoids is prolapse of hemorrhoids. There is a direct relationship between the increase in the duration of the disease, its stage and the frequency of prolapse of hemorrhoids. Anorectal bleeding, in addition to the main symptom of hemorrhoids, is a characteristic symptom of other diseases of the colon: malignant tumors, diverticulosis, nonspecific ulcerative and granulomatous colitis. Under the guise of hemorrhoids, especially when bleeding from the rectum, diseases such as polyps and colorectal cancer often occur. Therefore, for any manifestations of intestinal discomfort and, especially, when blood is released from the rectum, it is necessary to perform a digital examination, rectoscopy, colonoscopy or irrigoscopy. One rule must always be followed: at the slightest suspicion of a tumor, always take a biopsy and completely examine the colon [6, 9, 19, 21].
In modern conditions, the problem of hemorrhoids in pregnant and lactating women occupies a special place [1, 4, 13]. The clinical symptoms of hemorrhoids during pregnancy do not differ from those during the normal course of the disease. Most often these are pain in the anus, rectal bleeding and anal itching [5, 15, 22].
Often pregnant women are diagnosed with hemorrhoids in an asymptomatic stage. These women do not present complaints characteristic of hemorrhoids, but upon examination, hemorrhoidal nodes are found in typical places on the walls of the anal canal. Timely identification of pregnant women with clinically asymptomatic hemorrhoids and implementation of preventive measures in them makes it possible in many cases to prevent its development, which complicates the course of childbirth and the postpartum period [1, 13].
The clinical picture of hemorrhoids in pregnant women develops gradually. Initially, unpleasant sensations appear in the anus, especially after defecation. As the duration of pregnancy increases, more pronounced signs of hemorrhoids appear - pain, enlargement of hemorrhoids, bleeding, anal itching, tenesmus, etc. [1, 15, 22].
About half of women who have hemorrhoids during pregnancy experience an exacerbation of the disease after childbirth. As a rule, already with the onset of labor, pain in the anal area increases sharply. During the second stage of labor, when the fetal head passes the pelvic cavity, the vessels of this area, including the rectum, are sharply compressed. Venous outflow is disrupted, blood stagnation and tissue hypoxia increase. This creates additional conditions for the opening of arteriovenous anastomoses directly into the lumen of the cavernous cavities of the rectum. The longer the second stage of labor, the more pronounced these processes are. Hemorrhoids swell, increase sharply in size, and become tense. During pushing, the anal sphincter opens, the distal end of the rectum gapes, and both external and internal hemorrhoids are clearly visible. They enlarge before our eyes, become bluish and dense. After the end of the pushing, the internal nodes decrease somewhat, and with subsequent pushing, the picture repeats. When the fetal head erupts, internal hemorrhoids, if they are sufficiently pronounced, are squeezed out and sometimes their walls rupture. After childbirth, as the anal sphincter gradually contracts, the internal nodes become smaller and reduce on their own, but often, if the sphincter contraction occurs quickly, these nodes are pinched and acute hemorrhoids occur [1, 4, 13].
Conservative treatment, the main goal of which is to eliminate pain and inflammation and normalize blood circulation in the rectal area, is carried out for acute hemorrhoids and in the early stages of chronic hemorrhoids. Conservative drug treatment can be general - drugs that increase the tone of the veins, improve blood flow through small vessels and cavernous veins, and local - wound healing, analgesic and antipruritic ointments, suppositories, microenemas and baths [8, 16, 18].
Prevention of exacerbations is also of great importance, which includes:
- combating stool disorders (getting rid of constipation and improving bowel function without prolonged straining);
- proper nutrition (a diet rich in fruits and vegetables; a strict prohibition of any alcoholic beverages, salty, hot, spicy, pickled, peppered dishes, as these products increase blood flow to the veins of the pelvic floor and primarily the hemorrhoidal venous plexuses);
- proper hygiene after defecation;
- prevention of physical inactivity (physical therapy and hygienic gymnastics help improve the function of the large intestine, increase the tone of the muscles of the anal area and abdominal wall, and reduce congestion in the pelvic veins).
The development of hemorrhoids during pregnancy, as well as its complications, especially in the postpartum period, significantly affects not only the patient’s condition, but also her quality of life. When choosing a drug for treating a pregnant or lactating woman, one should take into account its safety both for the patient herself and for the fetus and newborn, which significantly limits the doctor’s choice [1, 10, 17].
For asymptomatic hemorrhoids, women are prescribed only preventive measures.
In stages I-II of the disease, treatment is carried out with suppositories and ointments, infusions of medicinal herbs, and the prescription of drugs taken orally. After defecation, it is possible to use rectal suppositories containing analgesic components. For spasm of the anal sphincter, it is possible to add suppositories with oil.
When hemorrhoids are combined with anal fissures, or acute hemorrhoids, conservative treatment is carried out in a hospital. It includes rest, diet, cleansing enemas, laxatives, novocaine blockades in the anus, local treatment with suppositories and ointments.
In case of prolapse of internal nodes, without symptoms of acute inflammation, they limit themselves to careful repositioning of the nodes after defecation (it is better to do this in a warm sitz bath). When there is a urge to defecate, small-volume cleansing enemas are recommended. Women are strictly prohibited from heavy physical labor and certain types of domestic work.
Pregnant women suffering from hemorrhoids with prolapse of internal nodes and frequent exacerbations of the disease are subject to hospitalization and surgical treatment. The timing of the operation is determined individually. Patients with such complications are treated with surgical (hemorrhoidectomy - excision of nodes) or minimally invasive treatment methods (minor or bloodless operations). These methods include sclerotherapy, ligation, infrared photocoagulation and laser coagulation. If the pregnant woman’s condition allows, all interventions are postponed to the postpartum period. Exacerbation of hemorrhoids, especially in combination with postpartum perineal trauma, is the most common disease that affects the quality of the postpartum period.
Currently, in obstetric practice for hemorrhoids, Procto-Glivenol is widely used, which is available in the form of rectal cream (1 g contains tribenozide 50 mg and lidocaine hydrochloride 20 mg) and rectal suppositories (1 suppository contains tribenozide 400 mg and lidocaine hydrochloride 40 mg).
The therapeutic effectiveness of Procto-Glivenol for hemorrhoids is due to the combination of two components: tribenoside and lidocaine. Tribenoside has a venotonic and anti-inflammatory effect. The venotonic effect is manifested by improving vascular tone, reducing venous stagnation, reducing the permeability of capillaries and venules and improving microcirculation. The anti-inflammatory effect is manifested by an inhibitory effect on some endogenous substances (bradykinin, serotonin, histamine), which act as mediators in the development of inflammation and pain. Lidocaine has a local anesthetic effect.
The above properties of Procto-Glivenol allowed it to take one of the leading places among antihemorrhoidal drugs, which is explained by the optimal composition, high efficiency and safety of use, especially during pregnancy (starting from the second trimester) and during breastfeeding, since it is during these periods that safety drugs is especially relevant.
Material and methods
We assessed the effectiveness and tolerability of Procto-Glivenol (cream and rectal suppositories) in the treatment of hemorrhoids in pregnant women. 85 pregnant women with clinical signs of hemorrhoids were examined.
All patients were divided into three groups depending on the stage of the disease. The 1st group consisted of pregnant women with asymptomatic hemorrhoids, who underwent preventive measures, including a diet with limited spicy foods and a sufficient amount of plant fiber, physical therapy, walks, and using the anal toilet after defecation. Group 2 consisted of patients with complaints of bleeding, anal itching, and pain during defecation. These women, in addition to the above measures, were treated with suppositories and cream with procto-glivenol from the second trimester of gestation. Group 3 (4 pregnant women) included patients suffering from hemorrhoids subject to surgical treatment. These were women with prolapse of internal nodes and with a history of frequent exacerbations, with heavy hemorrhoidal bleeding, as well as with acute hemorrhoids in the stage of necrosis of the prolapsed strangulated nodes. Pregnant women of group 3 were consulted by a proctologist, together with whom general tactics for further management were developed. These patients were also prescribed Procto-Glivenol according to individual regimens for preoperative preparation.
Procto-Glivenol cream was used for external hemorrhoids, applied to the affected areas in a thin layer 2-4 times a day, and after the pain disappeared - once for 7 days. Procto-Glivenol suppositories were used for internal hemorrhoids 2 times a day for 5-7 days, after the disappearance of painful sensations, once a day for another 7 days.
Results and discussion
It has been established that identifying pregnant women with clinically asymptomatic hemorrhoids and carrying out the special preventive measures described above make it possible to prevent the development of the disease, which complicates the course of childbirth and the postpartum period.
Clinically, the symptoms of hemorrhoids during pregnancy were almost no different from those among other categories of patients with this diagnosis. Of 85 pregnant women with clinical signs of hemorrhoids, pain in the anus was observed in 40 (47.1%), bleeding of nodes - in 28 (32.9%), anal itching - in 26 (30.6%). 55 (64.7%) of the observed women had external hemorrhoids, which was characterized by the appearance of hemorrhoids in the form of warty formations or folds, dense to the touch and not decreasing in volume upon palpation. In internal hemorrhoids (30-35.3%), the nodes were located between the folds of the mucous membrane, could be either single or multiple, collapsed when pressed and filled when coughing. In addition, in 13 (15.2%) pregnant women, hemorrhoids were combined with an anal fissure. It should be noted that if in pregnant women aged 20 to 30 years, hemorrhoids are detected in approximately every fifth, then after 30 years - in every second.
When assessing the results of therapy, the severity of remaining clinical symptoms was assessed by patients as average by the 7th day of treatment and as weak by the 15th day. At the same time, such a clinical symptom as pain during defecation was observed in 9 (10.5%) patients by the 7th day of treatment, and was not observed in any pregnant woman by the 15th day, bleeding - in 5 (5.9%) and 2 (2.4%), anal itching - in 6 (7.1%) and 2 (2.4%) women on the 7th and 15th days of treatment, respectively.
Clinical tolerability was assessed by patients and doctors on a scale: excellent, good, average, poor. Tolerability of treatment with Procto-Glivenol was excellent and good in 96% of cases.
conclusions
1. Procto-Glyvenol is the drug of choice for the conservative treatment of hemorrhoids and the prevention of its complications during pregnancy. The use of Procto-Glivenol, both in the form of cream and rectal suppositories, is an effective way to treat pregnant women with hemorrhoids.
2. The speed of action and good tolerability make it possible to recommend Procto-Glivenol for widespread use in obstetric practice.
A case from the practice of a proctologist
Now let's consider this situation. I wrote about her in my telegram channel “Doctor-heals”.
During the first pregnancy and after childbirth there were thromboses of nodes, veins, and blood. Well, everything is as it should be during an exacerbation of hemorrhoidal disease. Then everything went away. There are small folds left near the anus, which do not hurt, but only spoil the beauty. I’ll tell you a secret - THIS IS HEMORRHOIDS!, my dears.
And now you are planning your second pregnancy. Here we have the development of two very common options for further events:
- The first option is not at all smart: I closed my eyes and “drove through the intersection for luck, according to the principle “maybe I’ll get through”... This doesn’t happen often. The logic of the reasoning is simple: “Since hemorrhoids don’t bother you now, they won’t bother you during your SECOND pregnancy either.” Yeah! Blessed are the ignorant... Why, if hemorrhoids were inflamed during the FIRST pregnancy, then during the SECOND pregnancy they will not become inflamed. Maybe 1-2 out of 100 won’t, but that’s with my mother’s prayers... For the rest, it will be whatever it is. Don't say you didn't know. We didn’t think so – yes, I believe it. Now you know, I thought for you and told you.
- The second option is smarter, but the life principle: “trust, but verify” has not been canceled. As a conscientious patient, I went to the proctologist, and he said that there is no need to do anything now, anyway, after childbirth it will be larger, then we will operate. Re-read the first version of the story, well, you will get pregnant and what will happen next. Have you reread it? Now you know. In general, with this topic, “as for childbirth... it’s not necessary, anyway...” Dear, my dear readers, think about this phrase! She is very ambiguous! Let's look at similar situations. There is no need to treat your teeth either; they will fall out on their own (or they will pull them out if they hurt too much). There is no need to remove a polyp or mole either; when there is cancer, then we will operate. There is also no need to operate on appendicitis, but if there is already peritonitis... There is no need to undergo treatment in general either, everyone dies in the end anyway.
Of course, if we consider the issue of hemorrhoids in a woman who wants to get pregnant from the perspective of a proctologist 20-30 years ago, then yes, one operation is better than two. “And when there are larger hemorrhoids, we will cut them off, sew everything up, and if you don’t get pregnant, there is a high chance that you will no longer have hemorrhoids.”
But times are changing!
Now a proctologist can use a laser to remove 1-2 veins the size of a buckwheat grain, if necessary, not to mention the internal nodes, and live in peace. Have children, raise them to your joy.
You treat your teeth before pregnancy, knowing that during pregnancy they are more destroyed. Otherwise you will be left with stumps in your mouth. And after childbirth, they have to be treated repeatedly throughout their lives. And teeth are basically a bone structure, it is more stable than veins - soft tissue.
Prevention measures
Hormonal changes that occur in the body of the expectant mother inevitably affect the tone of the vascular walls, which leads to disruption of the outflow of blood from the veins of the lower extremities and rectum. In order to minimize the risk of hemorrhoids during pregnancy, it is recommended to follow these rules:
- A pregnant woman's diet should be dominated by ingredients rich in plant fiber, vitamins and microelements. Fatty and fried foods, dairy and fermented milk products with a high percentage of fat content, baked goods, confectionery products, seasonings, spices, and foods rich in starch should be excluded.
- Every day, in the morning, it is recommended to do light exercises or walk in the fresh air for 15-20 minutes.
- Pregnant women are recommended to lie in a horizontal position on their back several times a day, placing a pillow under their pelvis.
These simple measures will help maintain peristalsis in the large intestine, and also improve the outflow of venous blood from the lower extremities and pelvic organs.
Removal of hemorrhoids with laser
After this small operation, which is performed on an outpatient basis and without pain, during pregnancy there is a more than 90% chance that hemorrhoids will not bother you. In 5-10% of pregnant women, slight swelling appears in the anus (there is still living tissue there, and swelling also occurs on the legs). Sometimes small veins, up to several millimeters, may appear and become inflamed. This is not at all comparable to inflammation of an entire hemorrhoid. But this is my reinsurance.
For almost 5 years of practice, not a single patient I operated on came during pregnancy with large inflamed nodes, wrote to me in the messenger or called me.
Yes, 5-10% may have small nodes after childbirth. We will remove it with a laser again and live in peace.
A phrase I have repeatedly heard from patients: “It’s good to be without hemorrhoids!” speaks for itself.
How is the operation performed?
We remove hemorrhoids with a laser through small punctures of the skin near the node. The operation is painless and is performed under local anesthesia. After it, sometimes half of the patients experience discomfort for up to 30 minutes. You go home 1 hour after the operation and go about your business, but without much stress.
If someone is in fitness, then in 2-3 weeks, please train.
A small but important point - all this applies to small or medium-sized hemorrhoids.
If the hemorrhoids are large enough or old (several years), or in those who have had surgery before, the recovery is a little more uncomfortable in the first week or two after surgery. A little - actually a little. Don’t be afraid, you took the Nise tablet if necessary and nothing bothers you.
With long-term hemorrhoids, the skin around the anus may stretch and anal fimbria may form. At the request of the patient, we will make the butt beautiful - we will remove these fringes.
Symptoms of hemorrhoids at different stages
During the period of bearing a child, hemorrhoids often occur in an asymptomatic (latent) form, accompanied by characteristic signs only at the stage of active progression. At the initial stage, this disease can be expressed in the form of discomfort during bowel movements and slight pain in the rectal area. At the initial stage of development of the pathological process, light bloody discharge from the anus may appear. At the stage of active progression, the following clinical signs of hemorrhoids appear:
- itching in the rectal area;
- bloody and mucous discharge from the anus;
- the appearance of characteristic hemorrhoids in the perianal area;
- nagging pain in the rectum, radiating to the sacrum and lumbar region.
At the third stage of development of this disease, a woman feels an increase in clinical symptoms, an increase in the size of hemorrhoids and a general malaise associated with the inability to lead a normal lifestyle. At stage 4 of the disease, the expectant mother increases the risk of massive bleeding and other complications associated with thrombus formation.
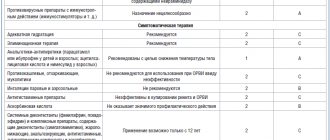
Classification of painkillers by release form
Hemorrhoids are a well-studied problem, so prevention and treatment methods always guarantee a good result. Despite the wide selection of drugs in pharmacies, only the attending physician can prescribe complex therapy after a thorough diagnosis of the problem. The form of release of drugs is selected depending on the individual preferences of the patient and the complexity of the symptoms. The most effective and acceptable forms of drug release are suppositories, ointments and tablets.
Candles
In an acute inflammatory process, it is extremely difficult to anesthetize a pronounced pain syndrome, because First you need to stop the swelling. Many proctologists advise the use of local anesthetics, which simultaneously relieve inflammation, relieve pain and promote the regeneration of anal fissures. The main advantages of local drugs:
- Minimum contraindications and side effects;
- Acts directly on the source of inflammation;
- Effective rate of absorption and symptom relief.
Unlike tablets, suppositories are used only for internal hemorrhoids. The neurotropic principle of action of the drug allows you to relieve pain by blocking the conduction of nerve impulses from the location of the “bumps” to the neurons of the brain.
Ointments and gels
Used for external and internal hemorrhoids. The main advantages of the drugs are ease of use, uniform distribution of the active substance and high absorption rate. The analgesic effect is achieved by relieving swelling and inflammation, narrowing the vessels of varicose veins, regenerating cracks and the antibacterial effect of the ointment. Among the names of popular products are Proctosan, Relief Advance, Proctosedyl.
Painkillers for hemorrhoids
Efficient and effective systemic drugs in the fight against the symptoms of hemorrhoids are venotonic and agnioprotective tablets. According to the principle of action, drugs can be divided into 2 types:
- Tablets that have only an analgesic effect. Their action is aimed at reducing painful symptoms. Painkillers have many contraindications, and the course of treatment cannot exceed several days.
- Systemic tablets with a dose-dependent effect can not only relieve attacks of pain, but also have a beneficial effect on the general condition of blood vessels. They affect the cause of the disease, increase venous tone, improve lymphatic drainage, increase vascular stability, thereby reducing inflammation of the nodes. Effective healing of cracks and microtraumas of the anal mucosa is achieved due to its regenerating properties. The most recommended tablets from this group are called “Phlebodia” and “Detralex”.
Before diagnosing yourself and treating the symptoms of the disease, you should consult a proctologist. Many drugs have contraindications and a special dosage regimen, without taking into account which you can harm your health and aggravate the course of the disease.
How to deal with hemorrhoids
It is important for pregnant women to pay attention to their diet, difficulties with bowel movements, stool retention, and discomfort when going to the toilet. Remember: it is better to start working on the situation at the first unpleasant manifestations in order to reduce the risks of developing hemorrhoids and establish a natural physiological process
The most important conditions for the comprehensive fight against hemorrhoids and improving the quality of life of a pregnant woman are:
- increasing physical activity (of course, if possible);
- balanced diet rich in fiber;
- consuming a sufficient amount of fluid in order to normalize the functioning of the gastrointestinal tract, soften stools and mildly comfortable cleansing of the intestines2,4. Moreover, when pregnancy is accompanied by constipation, it is important to pay special attention to this.