Diabetic foot is a broad concept that refers to the destruction of the skin, bones and nerves in the feet that develops in patients with diabetes and can lead to the death of the limb.
The main cause of diabetic foot syndrome (DFS) is damage to blood vessels by atherosclerotic plaques and mediocalcinosis (hardening of the vessel walls), characteristic of diabetes mellitus. Blood flow is disrupted, ulcers and gangrene develop, and wounds may not heal at all.
In addition, diabetics develop peripheral nerve damage (neuropathy), which reduces the sensitivity of the skin of the legs and the secretion of sweat. Patients with neuropathy do not feel pain from minor injuries and may not notice them until the wounds turn into trophic ulcers.
A dangerous factor for complications in diabetes is severe immunodeficiency. It promotes the unlimited spread of infection through soft tissues and the development of general blood infection - sepsis.
Only a comprehensive impact on all factors of the syndrome can successfully prevent amputation and death of these patients.
Effect of diabetes on feet
If blood glucose levels are consistently high for 5-10 years, metabolism is disrupted. This leads to the formation of trophic changes in the bones, skin, muscles, blood vessels, and tendons. The legs suffer first - diabetes is often accompanied by excess weight and varicose veins.
Also, patients with diabetes have reduced immunity, as a result of which wounds, scratches, and ulcers take months to heal. The pathology is accompanied by a violation of the nerve conduction of the skin, as a result of which a person simply does not feel damage to the skin. All this leads to the development of diabetic foot. Untimely treatment can lead to serious complications, leading to serious consequences: from amputation to death.
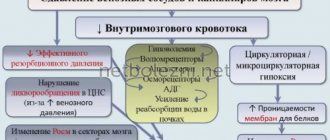
Angiopathy
In diabetes, damage to blood vessels often occurs - angiopathy. They become covered with atherosclerotic plaques, which leads to circulatory failure in the foot. It looks a bit like rusty pipes. Very little water comes out of the tap due to rust blocking the inside of the pipes. The same thing happens when blood vessels are clogged. If the vessels in the legs become clogged or completely blocked, the skin and tissues will suffer first from poor circulation. The process of delivering oxygen and nutrients to the limb will be disrupted, which means cell death in the affected area.
- Decreased ability to fight infection
- The ability to heal wounds will decrease.
- Signs of blood vessel damage
- Pain in the lower leg when walking,
- A change in the normal color or temperature of the feet,
- Leg pain at night or while resting.
If nerve damage is combined with poor circulation, the risk doubles. You are more likely to get injured (because you don't feel pain) and the injury will lead to infection or ulceration. Healing will not occur due to poor circulation, which will inevitably lead to gangrene.
Risk factors for developing diabetes include poor diet and glucose control, poor circulation, smoking, and diabetes mellitus of more than 10 years.
Diabetic foot symptoms
The pathology may not manifest itself as obvious symptoms for a long time. However, there are a number of indirect signs indicating the development of diabetic foot syndrome:
- lameness;
- swelling, swelling of the legs at the slightest physical activity;
- heaviness in the legs when walking;
- periodic numbness of the lower extremities;
- dry skin of the feet, the formation of deep cracks that constantly become inflamed and take a long time to heal;
- the appearance of small rashes, ulcers on the skin of the feet;
- feeling of heat in the legs when touched;
- frequent formation of calluses and blisters;
- change in foot color;
- thickening, deformation of nails;
- the constant presence of non-healing ulcerative defects on the feet.
Without proper treatment for diabetic foot syndrome, the situation will worsen. The main signs of advanced pathology are:
- the foot stops sweating;
- the skin of the foot turns pale/purple;
- necrosis of the foot and fingers appears;
- joint dislocations are possible, but due to low sensitivity the patient does not feel damage.
Ignoring the symptoms can lead to a secondary infection, which in 90% of cases ends in amputation of the limb. Therefore, at the first suspicion of the development of pathology, it is necessary to consult a doctor who will diagnose diabetic foot syndrome and select the correct treatment tactics.
Causes
Often, diabetic foot syndrome is a consequence of diabetes mellitus, which is accompanied by atherosclerosis, coronary heart disease, arterial hypertension, smoking, and alcohol abuse.
However, a diabetic leg ulcer can also be caused by a seemingly harmless cause. People suffering from diabetes may not pay attention to calluses, corns, cracked heels, or ingrown toenails that appear due to tight shoes. Meanwhile, these small injuries provoke the disease.
Diabetes mellitus negatively affects the functioning of the entire body, but the lower extremities suffer the most (especially since they bear a serious daily load). Saturation of the blood with excess sugar and glucose destroys blood vessels - large and small (a distinction is made between macro- and microangiopathy in diabetes), bones and muscles. Due to anatomical features, blood circulates in the legs of any person worse than in other parts of the body, so it is the feet that are the first to suffer from total circulatory problems in diabetes.
Types of diabetic feet
The classification of diabetic foot syndrome is as follows:
- Neuropathic. Diagnosed in 70% of cases. Accompanied by deformation of the nervous system. Degenerative changes in the body are so strong that the patient does not feel touch on the affected foot, does not feel pain from cracked feet, or ulcers on the sole. The wounds on the feet have smooth edges, the limb is hot when touched.
- Ischemic. Accompanied by circulatory disorders in the lower extremities. The main symptoms are cold feet, severe pain when walking, lymphostasis in the calf muscles and ankle. The ulcers have ragged edges and are localized mainly between the fingers, which makes their treatment much more difficult.
- Neuroischemic. The most dangerous form of diabetic foot, combining the symptoms of the two above. It is simultaneously accompanied by a violation of the peripheral nervous system and blood circulation in the lower extremities.
Only a doctor can give clinical recommendations for diabetic foot syndrome, depending on the severity of the disease, its form, and the individual characteristics of the body. You should not risk your health and ignore the symptoms of the disease. A timely visit to the doctor will help avoid irreversible consequences of the pathology.
Neuropathy
Neuropathy - damage to sensory nerves occurs in 70% of patients with diabetes. Nerves in the legs are particularly susceptible to damage because poor diet and high sugar levels destroy the myelin sheath. In the neuropathic form, where a diabetic patient loses sensation in the legs, any microtrauma may go unnoticed until serious ulcers develop.
Signs of foot neuropathy:
- Numbness of the skin
- Tingling
- Pain or burning of the skin of the legs (some forms of neuropathy may cause pain)
Stages of pathology development
Regardless of the form of the disease, it develops sequentially. When moving to a new stage, existing symptoms become more acute and new ones are added.
The course of diabetic foot, regardless of classification, is as follows:
- Initial stage. It is characterized by changes in the shape of the foot, bone deformation, and the formation of blisters and calluses.
- Stage 1. Accompanied by the formation of ulcers and necrotic wounds, while the deep structures of the skin are not damaged.
- Stage 2. Ulcerative and necrotic skin lesions deepen into the dermis, affecting muscles, joints, and tendons.
- Stage 3. The ulcer deepens to the bone tissue, and in the vast majority of cases a wound infection is associated. An abscess and osteomyelitis develop.
- Stage 4. It is characterized by the formation of limited gangrene on the supporting part of the foot. The tips of the fingers turn black, the destructive process has smooth and clear edges. At this stage, the limb can still be saved through surgery.
- Stage 5. Accompanied by a significant increase in the area of tissue death. Gangrene affects the lower leg. In this situation, the process is irreversible, and the only option to save the patient’s life is amputation.
Exercise therapy
For diabetic feet you can do:
- Exercise 1. Starting position - sitting on a chair, legs lowered down and brought together. Alternately bend and straighten your toes 5 to 10 times, first on one leg and then on the other.
- Exercise 2. The starting position is the same. First, you should raise your toes up for 5 to 10 seconds, keeping your heel pressed to the floor. Then the toes should be lowered and the heel raised up (also for 5 - 10 seconds). Repeat the exercise 3 – 5 times.
- Exercise 3. The starting position is the same. Raise one leg 5 - 10 cm above the floor and begin to perform circular movements with your foot, first in one direction (3 - 5 times), and then in the other. Repeat the exercise with the other leg.
- Exercise 4. The starting position is the same. First, you should straighten one leg at the knee, and then bend it at the ankle joint, trying to pull the toes as low as possible. Hold your leg in this position for 5 - 10 seconds, then lower it and repeat the exercise with the second leg.
- Exercise 5. The starting position is the same. Straighten your leg at the knee, then straighten it at the ankle joint, trying to reach your toes with your fingers. Repeat the exercise with the second leg.
Physical therapy (physical therapy) and special gymnastics can have a certain positive effect on diabetic feet. The purpose of physical exercise in this case is to improve blood supply to ischemic tissues of the lower limb. However, it is worth remembering that in the ischemic form of the disease, the mechanism of damage is the blockage of the blood vessels through which blood flows to the tissues, so excessive loads can lead to increased pain and the development of complications. That is why you should immediately exclude any exercises and activities associated with increasing the load on the feet (walking, running, cycling, lifting weights, staying in a “standing” position for a long time, and so on).
Diabetic gangrene of the foot
If you ignore the symptoms of diabetic foot, you are likely to develop dry or wet gangrene. Its main symptoms are pain, blackening of the limb, and lack of sensitivity in the affected area. Gangrene may be accompanied by suppuration, nausea, chills, and elevated body temperature. Pathology never occurs suddenly - it is the result of ignoring signs of progression of diabetic foot. If gangrene is present, conservative treatment methods are not used. Depending on the extent and type of necrosis, the patient is indicated for necrectomy or complete amputation of the limb.
How does SDS develop?
The pathogenesis of the formation of diabetic foot is due to three main reasons:
- Damage to the blood vessels of the lower extremities;
- Diabetic neuropathy is the most common complication of diabetes;
- Infection, which usually always accompanies the first two factors.
The predominance of certain disorders: either the clinical picture of neuropathy, or changes in the peripheral blood flow, determines the symptoms of diabetic foot, which represent 3 forms of the pathological process. Thus, we distinguish:
- Neuropathic variant, which is characterized by damage to the nervous system, both somatic and autonomic. The classification of neuropathy in diabetes is quite extensive, but the main driving force for the development of DFS is considered to be a decrease in the conductivity of nerve impulses in sensory and motor peripheral nerves, as well as a violation of all types of sensitivity (vibration, tactile, thermal). Neuropathy, as a sign of diabetic foot, can occur in three scenarios: diabetic foot ulcer, osteoarthropathy with the formation of a Charcot joint, and neuropathic edema.
- Neuroischemic or mixed form, including signs of both neuropathies and ischemic lesions caused by pathological processes affecting the nervous system and the main vascular bed.
- An ischemic type that develops as a result of atherosclerotic changes in the walls of the arterial vessels of the legs and leads to disruption of the main blood flow.
Isolated forms, in particular neuropathic and ischemic, are less common, except at the beginning of the process. As a rule, over time, a mixed form is formed: if DDS is initiated by ischemia, then it will not be possible without the participation of nerves, and vice versa - neuropathy will sooner or later involve the participation of vessels, which in diabetics are very quickly and often affected by atherosclerosis.
Prevention of diabetic foot
In order not to have to deal with the treatment of diabetic foot syndrome, you need to fight the pathology even before its manifestation. There are some simple tips that will help prevent the development of the disease.
What shoes to wear
If you have diabetic feet, you should wear only comfortable shoes with a strong last. It should not be narrow, press or rub, and have a soft sole. It is better to purchase shoes in the afternoon, when the foot swells. It is also recommended to give preference to models with adjustable foot width. Be sure to check that the insole inserted inside the shoe lies flat and firmly and is not deformed.
If the foot is deformed or there are ulcerative skin lesions, special orthopedic shoes are needed.
How to take care of your feet
You should check your feet daily for cuts, cracks, sores, blisters, and other skin changes. If you can't see hard-to-reach areas, use a mirror. Daily examination is extremely important, because sensitivity in diabetic feet is significantly reduced. Even after receiving serious damage, you simply may not feel it.
You should also take proper care of your feet. Foot hygiene should be performed daily. Wash your feet with soap, gently wipe with a soft towel, and thoroughly dry the spaces between the toes. Change your socks regularly.
Basic rules for foot care
Diabetic feet need to be cared for daily, following simple rules of prevention:
- careful hygiene, including the interdigital space;
- treatment of keratinized areas with pumice;
- moisturizing dry skin with cream;
- Regularly changing socks. Socks and stockings must be made of natural fabric and selected exactly in size so that folds and gathers do not form and the tissues of the foot and lower leg are not compressed;
- wearing loose, comfortable shoes.
In addition, it is important to carefully trim your nails in a straight line, not to use medicinal products without a doctor’s prescription, to do daily exercises to improve blood flow, and to undergo regular medical examinations.
What not to do:
- walk barefoot even after all ulcers and other injuries have healed;
- be exposed to hypothermia;
- warm your feet by rubbing, steaming and using a heating pad;
- cover the damage with a band-aid without consulting a doctor. You should only use special dressings prescribed by your doctor.
Diagnostics
Diagnosis of diabetic foot involves examination by an endocrinologist and neurologist. At the appointment, the specialist performs a sensitivity analysis of the foot and listens to the blood flow in the arteries of the foot. In order to make a diagnosis, it is necessary to undergo a comprehensive examination, including:
- X-ray examination aimed at assessing the condition of the bones in the affected area;
- a blood test, based on the results of which a specialist will determine the severity of the inflammatory process;
- Dopplerography and ultrasound to assess the condition of the vascular bed in the affected area;
- X-ray contrast angiography of blood vessels, with which the doctor will assess the general state of blood flow in the affected limb.
Diagnosis of diabetic foot syndrome is a key point in selecting the correct treatment tactics. The sooner you consult a doctor, the higher the likelihood of avoiding surgical intervention and limiting yourself to conservative methods of therapy.
Who is at risk
Patients with diagnosed type II diabetes are most at risk, since tissue damage occurs quickly in them, and in patients with type I - only after 6 years. Also at risk are people with the following disorders:
- conditions after a heart attack or stroke;
- tendency to thrombosis;
- high degree of obesity (III, IV);
- constant jumps in sugar levels;
- alcohol and smoking abusers.
Treatment of diabetic foot
The main clinical recommendation for the treatment of diabetic foot is compensation of the underlying disease. It is necessary to carefully monitor your blood sugar levels, avoiding sudden jumps. If there are signs of developing diabetic foot syndrome, you should immediately consult a doctor. He will prescribe one of the conservative treatment methods that will help stop the progression of the pathology.
Tablets
Treatment of diabetic foot syndrome involves taking the following medications:
- Antispasmodics. Necessary to reduce pain.
- Agnioprotectors. Medicines help control the symptoms of the disease and stabilize the pathological process.
- Pentoxifylline. A drug necessary to improve blood microcirculation in ischemic lesions of the extremities.
- Lipoic acid, Actovegin. These medications are needed to normalize tissue metabolism and increase the utilization of glucose by cells.
- Detralex, Troxerutin. Necessary for restoring the functions of vascular walls and improving the functioning of lymphatic vessels.
- Antibiotics. Prescribed in case of infectious complications.
- Medicines to lower blood pressure. Indicated for patients with high blood pressure.
Only a doctor can prescribe tablets, based on the current stage of the diabetic foot and the general condition of the body.
Folk remedies
DFS can be treated at home only in the early stages. Therapy with folk remedies consists of regularly treating wounds and ulcers to avoid infection. When choosing one of the traditional methods, remember: such treatment cannot replace medication. Alternative medicine is permissible, but only after agreement with the attending physician, as a complement to the main therapy.
Ointments
When treating diabetic foot, you can use antimicrobial agents in the form of ointments and special gels. It is necessary to monitor the condition of your feet, treating your feet with fatty creams daily (if they are dry). Do not apply the product to the spaces between the fingers. You should not choose an ointment on your own - purchase the medicine only after consulting a doctor. An incorrectly selected remedy can only worsen wound defects.
Flow
When the development of diabetic foot begins, diet and control of sugar levels, proper foot care, periodic examination of the feet and timely monitoring by a doctor are extremely important. In this case, complications rarely develop. In European countries where podiatry services are developed, the development of diabetic gangrene is very rare. The number of amputations due to diabetes in Europe has decreased tenfold, but in Russia diabetic gangrene is the main cause of high amputation rates.
Surgery
If diabetic foot ulcers penetrate into blood vessels or bones, surgery is necessary. Modern medicine has the following methods for treating SDS:
- Angioplasty. Involves vascular plastic surgery and restoration of blood circulation. The operation allows you to save the limb.
- Necrectomy. The affected areas of tissue are excised to stop the spread of the pathological process.
- Endarterectomy. The doctor clears the arteries of blood clots and atherosclerotic deposits to restore normal blood flow in the affected limb.
- Autovenous shunting. The vascular surgeon creates an artificial network of blood vessels to supply the affected foot with enough blood.
- Arterial stenting. Indicated in case of blockage of the walls of blood vessels. A special metal frame is installed inside the artery of the lower limb, expanding its lumen.
How to determine the severity of foot damage?
People with “diabetic foot” need to undergo a full examination at least once a year, which includes an assessment of the condition of their feet. Early diagnosis is very important for timely treatment of identified problems. Consultation with a neurologist, surgeon, vascular surgeon, or podiatrist is necessary. Leg disorders most often develop slowly. It is important to evaluate the condition over time in order to identify minimal deviations at the initial stage.
The podiatrist checks the condition of the skin of the feet, the presence of calluses, and areas of hyperkeratosis. Checks feet for fungal infections, cracks, and foot deformities. If necessary, treats feet and prescribes treatment.
Assessment of vascular condition
The vascular surgeon assesses the condition of the skin of the legs, feels their pulsation, and measures the pressure on the popliteal and femoral arteries. For a more detailed analysis of blood flow in the legs, rheovasography and Dopplerography of the vessels of the lower extremities are prescribed. These methods make it possible to determine the speed and nature of blood movement, the condition of the vascular walls, vascular patency, the intensity and volume of blood flow.
Sensitivity assessment
The neurologist checks reflexes with a neurological hammer, temperature, tactile, pain, and vibration sensitivity of the legs.
The doctor checks tactile sensitivity using a simple monofilament test. Monofilament is a piece of nylon thread weighing 10 g, secured in a convenient holder. During diagnosis, it is placed so that it is located perpendicular to the skin. In this case, at the moment of contact, the monofilament should reach a bent state. The doctor touches certain points on the plantar part of the foot for 1.5 seconds, and then asks the patient about the sensations. If a person does not feel pressure when touching the monofilament, then sensitivity is weakened. And such a patient belongs to the risk group for developing foot wounds.
Vibration sensitivity in diabetic feet is analyzed using a graduated tuning fork with a frequency of 128 Hz. After installing its leg on a certain area of the leg or foot, the duration of the patient’s sensation of vibrations is assessed.
Pain sensitivity is tested by applying tingling stimulation with a needle.
Temperature sensitivity is determined by a “Tip-therm” tester, one end of which is made of plastic and the other of metal. The doctor alternately touches the big toe, dorsum of the foot, inner ankle, and skin of the lower leg with metal (cold) and plastic (warm) surfaces. Normally, the patient should feel the touch of these materials differently.
Self check
To independently assess the sensitivity of your feet to touch, you can use a feather or a piece of cotton wool. It’s easy to run it along the sole of your foot and analyze your sensations. Temperature sensitivity can be checked by touching hot or cold water first with your hand and then with your foot and comparing the sensations. Normally they should be the same. If you feel that the water is hot with your hand, but not with your foot. This may indicate a loss of the ability to sense temperature.
Self-diagnosis does not provide an objective assessment of the situation, so it is better to see a doctor and undergo standard tests.
Recommendations for patients with diabetic foot
Treatment of DFS requires an integrated approach. Patients need:
- Stick to a diet. It is necessary to give up fast carbohydrates, processed foods, fried and fatty foods. The patient should increase the consumption of plant foods.
- To refuse from bad habits. Smoking and alcohol are strictly prohibited. All this is a serious risk factor for the progression of diabetic foot syndrome.
- Get a professional pedicure. It is extremely important to prevent ingrown nails, which can lead to the development of an inflammatory process.
- Do not walk barefoot even with healed wounds. It is necessary to wear socks or tights made from natural fabrics that do not compress the limbs.
- Avoid sudden temperature changes. This puts a serious strain on the vascular bed, leading to poor nutrition of the limbs.
- Ensure free flow of blood to the legs. Every hour you need to do exercises, exercise your feet, and prevent blood stagnation in the lower extremities. While sitting on an armchair or sofa, place your feet on a stool or pouf to keep them elevated.
- Exercise. The best options are yoga, walking, swimming, cycling.
It is extremely important to notice the development of diabetic foot syndrome in time. Timely measures taken will help avoid serious consequences.
Still have questions about diabetic foot syndrome?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
Complications
The extreme and most dangerous stage of DFS is the development of gangrene of the foot. Diabetic foot is the leading cause of non-traumatic amputation in peacetime. Every year in Russia 70,000 amputations are performed for diabetic gangrene.
Diabetic gangrene often occurs with an associated anaerobic infection. With this outcome, the damaged tissues die, and the blood and healthy tissues become infected. The disease develops very quickly, often leading to death.
Trophic ulcers are another complication, most often found on the sole or big toe. They can also form on the sides of the foot from poorly fitting shoes. If left untreated, they can lead to serious infections. The classification of complications of diabetes includes trophic changes in the skin of the foot.