Bursitis
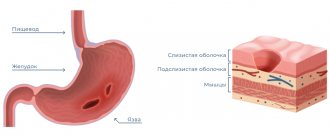
is an inflammatory disease that occurs in the synovial bursa of the joint and is associated with the accumulation of fluid in the joint cavity.
Bursitis can occur in all 180 joints of the human body
, from the smallest to the largest, partially or completely limiting movement in them.
This disease is just a defensive reaction of the body, which is trying to protect the injured lining of the joint capsule from further destruction. Indeed, rest is necessary to cure bursitis, because sometimes (for example, with an injury), it gives the joint time to heal and recover, and with it the inflammation goes away. But acute bursitis can cause irreparable damage to the joint and lead to the formation of adhesions on the synovial cartilage
. And if left untreated, it can cause purulent arthritis of the joint, osteomyelitis, spread of infection throughout the body, or persistent limitation of joint mobility.
Like most diseases, bursitis can be completely cured in the early stages. But how to recognize it in time? How to treat bursitis? We will tell you who is at risk, how to prevent the disease and how to avoid complications.
Bursitis is a disease in which the joints become inflamed.
Causes of bursitis
The leading triggers of bursitis include injury or overload, infection in the joint capsule or the formation of metabolic crystals in it in some chronic diseases.
Inflammation can be caused by, among other things:
- even minor damage to soft tissue in the periarticular area (cut, bruise, abrasion, muscle sprain, ligaments or tendons), especially if it is accompanied by hemorrhage into the joint capsule;
- inflammatory process near the joint - for example, in the subcutaneous tissue (phlegmon), epidermis (carbuncle, furuncle), medullary canal (osteomyelitis);
- generalized or focal chronic infection (for example, tonsillitis, caries, nasopharyngitis, genitourinary, intestinal, respiratory infections, pyogenic processes occurring in any organ;
- deposition of crystals in the joint capsule (for example, uric acid - in gout);
- monotonous static and dynamic physical activity of any intensity (from carrying loads to working with vibrating tools, exhausting housework or prolonged standing);
- physical overload and failure to comply with safety precautions when performing sports exercises;
- unfavorable working conditions (for example, the need to hold their hands above their heads for a long time puts painters at risk for shoulder bursitis);
- overweight;
- chronic diseases associated with metabolic disorders (diabetes mellitus, chronic alcoholism, gout, obesity, adrenoleukodystrophy, AIDS, liver and kidney diseases);
- autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, scleroderma);
- taking certain hormonal medications and age-related changes in hormonal levels;
- acute intoxication;
- increased allergic sensitivity;
- exposure to temperature factors (for example, overheating or hypothermia);
- incorrect posture;
- history of bursitis, as well as other diseases of the musculoskeletal system.
Those at risk for bursitis include:
- athletes (cyclists, parkour athletes, golfers, gymnasts) and people engaged in heavy physical labor;
- persons infected with staphylococci, streptococci, gonococci, pneumococci, patients with tuberculosis or brucellosis, as well as other chronic infections;
- allergy sufferers;
- patients who have had infectious diseases or have weakened immunity for other reasons;
- elderly people.
Classification of bursitis disease
As a disease, bursitis is usually divided into:
- specifics of the course
(acute, subacute, chronic or recurrent); - pathogen
(specific or nonspecific infections, inflammation without an infectious pathogen), as well as origin (primary or secondary bursitis); - type of exudate
(serous, purulent, hemorrhagic) - localization
.
Bursitis with a sudden onset and acute course can be completely cured if therapy is started early. If a visit to the doctor is constantly postponed or his recommendations are not followed, the transition to a chronic form is most likely
- in this case, the disease lasts several months, and subsequently recurs, causing irreparable consequences.
As a primary disease, bursitis occurs with direct damage to the joint capsule or local infection. Secondary - as a consequence of another chronic disease. The type of exudate can be determined only after taking a sample - based on it, treatment will be selected.
Advantages of Dr. Elshansky I.V.
Our clinic, located in the center of Moscow, traditionally deals with bursitis of various types and locations.
Main competitive advantages:
- Doctor with extensive (over 25 years) experience, Ph.D.
- The ability to perform all necessary manipulations immediately, on the day of treatment, incl. ultrasound guided punctures
- If necessary, an ultrasound scan is performed immediately during the appointment and is included in the cost.
- We do not prescribe unnecessary tests and examinations, and if there is still a need for them, we do not require them to be done exclusively in our clinic
- Qualified, polite staff
- No queues - we plan the time and accept appointments strictly by appointment
- Convenient transport accessibility - 5 minutes walk from Turgenevskaya metro station, Chisty Prudy, Sretensky Boulevard
Symptoms of bursitis
Acute bursitis usually begins suddenly and is accompanied by:
- sharp pain that intensifies with movement, as well as pricking or shooting pains at night;
- soreness and hypersensitivity of the skin over the joint;
- limitation of mobility in the joint;
- hyperemia and swelling of the skin over the joint;
- local or general increase in temperature;
- weakening of muscles;
- when palpating the joint, you can detect a non-rigid seal filled with liquid, which resembles a balloon filled with water to the touch;
Most often, symptoms of bursitis appear in the shoulders
,
knee
,
elbow and hip joints
, as well as
joints in the area of the heel tendon
. Symptoms and treatment of bursitis depend on the intensity of the inflammation. If left untreated, the increase in body temperature can reach 40°C due to a purulent process. At this stage, there is a high probability of complications - for example, erysipelas, subcutaneous fat tissue suppuration.
Symptoms of chronic bursitis are that:
- pain becomes moderate, tolerable or absent altogether;
- the infused seal under the skin remains for a long time;
- movements are less constrained or there is no restriction on their amplitude at all.
The recurrent process is characterized by a combination of all the symptoms of bursitis: the chronic course is periodically interspersed with exacerbations of symptoms. If this condition is not treated
,
subsequently fistulas begin to form
,
which create the risk of purulent arthritis
.
Fluid accumulation in the joint cavity is a common symptom of bursitis.
Preventive measures
The best method of treating diseases is their timely prevention. To avoid having to experience the effectiveness of modern treatment methods, it is best to take preventive measures. Let's try to figure out what these include.
Disease Prevention
A number of simple recommendations will help prevent elbow bursitis, compliance with which will ensure the ability to maintain healthy joints and the overall level of quality of life:
- Preventing injuries, ensuring skin protection.
- Providing high-quality first aid for injuries to the skin or joint.
- Timely seeking medical help.
- Maintaining a healthy lifestyle.
- Quitting bad habits (smoking, drinking alcohol, overeating).
- Attending preventive medical examinations.
- Preventive use of a course of chondroprotectors like Artracam.
Diagnosis of bursitis
Some specialists diagnose bursitis only based on a survey and physical examination of the patient. During oral data collection, the doctor clarifies the presence of injuries, diseases, recent infections, overuse, as well as specific symptoms of bursitis and a list of medications taken (some blood thinners can cause bleeding in the joint).
However, to confidently differentiate the disease, bursitis from synovitis and other similar pathologies, the doctor may prescribe standard procedures: x-ray examination
or
ultrasound of the affected joint
. If the clinical picture is blurred (for example, by the chronic course of the disease, taking anti-inflammatory drugs and analgesics, concomitant diseases), additional studies may be needed. Less commonly, computer or magnetic resonance imaging of the diseased joint is prescribed.
To determine the causes of bursitis, you may need to:
- biochemical examination of blood and urine;
- serological tests for the presence of antibodies to infections;
- study of biomaterial using PCR to determine the pathogen;
- puncture (fluid sampling) of the joint capsule to determine the microorganisms involved in the inflammatory process, as well as their sensitivity to antibacterial agents.
The combination of various research methods eliminates inaccurate diagnosis and helps the doctor reliably determine how to treat bursitis.
Why self-medication is dangerous
Self-medication is no less dangerous. A doctor at an appointment can recognize bursitis even by minimal signs. To confirm the diagnosis, he will prescribe an ultrasound, x-ray, MRI and will know exactly where the inflammatory process is located. After this, the doctor prescribes treatment for acute bursitis, which may include:
- non-steroidal anti-inflammatory drugs (NSAIDs) – Ibuprofen, Dexalgin, etc.; these drugs also have an analgesic effect;
- in case of a purulent process, the doctor pierces the bursa, removes the pus and rinses the cavity with antiseptics and administers antibiotics;
- in case of severe inflammation, hormonal drugs are injected into the bag;
- prescribes physiotherapeutic procedures.
If all this is not done and treatment is carried out at home with folk remedies, then the risk of developing complications increases sharply, the treatment of which is problematic even for a specialist.
Acute bursitis rarely develops without chronic joint injury. Joint pain requires immediate medical attention. If this is not done, the consequences may last a lifetime.
Sign up for a free initial appointment
Treatment of bursitis
In most cases, bursitis requires conservative treatment for 2-5 weeks; surgical intervention is indicated only in particularly advanced cases or with the development of purulent bursitis.
In addition to taking medications in accordance with the doctor’s recommendations, the patient is recommended physiotherapeutic procedures to relieve inflammation, as well as complete rest. To relieve stress on the joint, you can use plaster splints or walking aids.
With a mild inflammatory process, treatment of bursitis is carried out at home and includes rest, wearing an elastic bandage, applying compresses with decongestant and anti-inflammatory compounds.
You can use an ice compress before visiting an orthopedist or rheumatologist.
to relieve swelling and tenderness, or
cooling ointments
as a temporary measure to relieve the symptoms of bursitis. For this purpose, ice is applied to the sore joint for 5-15 minutes every 4-6 hours.
Surgical treatment of bursitis
In cases where the seal over the joint is too large and the process of its resorption will take too long, the doctor may decide to perform a minimally invasive operation - puncture
or
drainage
to drain excess fluid. The puncture can be combined with arthroscopic lavage - a procedure in which disinfectant solutions are injected into the joint capsule, and then they are removed back and an intra-articular injection of a steroidal anti-inflammatory drug is performed.
Also, surgical treatment of bursitis is indicated for suppuration in the cavity of the joint capsule, the formation of articular adhesions that interfere with normal mobility in the joint. In case of severe purulent inflammation and the settling of a diseased amount of crystals on the lining of the joint capsule, arthrotomy (opening of the joint cavity) may be necessary. It is performed through a small incision (up to 1 cm) with the removal of dead tissue, metabolites, calcium deposits on tendons and other foreign objects, which allows you to quickly and reliably relieve the patient’s condition even with severe acute and chronic bursitis.
In case of phlegmon, fistulas, and also when conservative treatment of bursitis is ineffective, tissue excision is performed - bursectomy or other types of ectomy.
As a rule, pain goes away immediately after surgery.
,
mobility in the joint is restored after a few days
,
and sutures are removed 10 days
after the intervention.
Physiotherapy in the treatment of bursitis
Physiotherapy in the treatment of bursitis is indicated in cases where medications are not enough to quickly and completely stop the inflammatory response. Physiotherapeutic techniques for the treatment of joint bursitis can normalize the metabolic process in the affected tissues, relieve swelling and pain, and affect the inflamed area at the cellular level. They enhance the effect of medications and help achieve drug-free remission in chronic bursitis. The following procedures are most effective:
- magnetic therapy;
- shock wave therapy;
- balneotherapy;
- cryotherapy;
- medicinal electrophoresis (usually with novocaine);
- UV irradiation;
- paraffin applications, ozokerite;
- kinesiotherapy (only in remission);
- massage (only in remission).
They allow you to restore mobility in the joint and prevent relapses and complications.
Exercise therapy in the treatment of bursitis
Therapeutic exercises for bursitis are indicated purely as a means of rehabilitation and prevention of relapses. It is strictly forbidden to perform any exercises during an exacerbation of the disease.
. The presence or absence of inflammation must be determined by a traumatologist or orthopedist.
The choice of exercises for the treatment of bursitis is determined primarily by the localization of the disease in a particular joint, the presence of complications and the purpose of performing gymnastics. As a rule, standard sets of exercises are used to restore mobility in the joint. Conventionally, the exercises in them can be grouped as follows:
- gentle stretching of muscles and extension of the joint manually;
- flexion-extension of the joint;
- rotation in the joint;
- general strengthening of the muscles of the limb (for example, lifting);
- overcoming additional resistance during flexion-extension.
The load when performing exercises should be increased gradually. If you experience the slightest pain in a joint, you must stop exercising immediately!
Therapeutic gymnastics - a means of rehabilitation after illness
Drug treatment of bursitis
The choice of medication for bursitis depends on the results of a synovial fluid test. If its composition is normal and does not contain dead leukocytes and infectious pathogens, anti-inflammatory therapy with nonsteroidal and steroidal drugs is carried out. If the analysis reveals infectious agents, an individual antimicrobial treatment program is drawn up based on the antibioticogram.
Anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs are used as the main medications for bursitis. When the inflammatory process is mild, NSAIDs are prescribed topically, in other cases - systemically (in the form of tablets or injections) or in combination with each other.
A severe inflammatory process, which is accompanied by severe pain and cannot be controlled with non-steroidal drugs for bursitis, requires the use of hormonal agents - glucocorticoids (GC). They are usually injected directly into the joint capsule after it has been washed; less often - used for intramuscular or intravenous administration.
If the inflammatory process subsides before taking medications for bursitis, doctors predict a successful cure for the disease without restricting mobility in the future
.
Both NSAIDs and GCs have side effects, so you should consult your doctor for an individual prescription before using them. Do not use NSAIDs for erosive and inflammatory lesions of the mucous membranes of the stomach and intestines.
In addition to anti-inflammatory drugs, regular analgesics can be used after visiting a doctor.
The following NSAIDs are used for bursitis: Naproxen
,
Meloxicam
,
Nimesil
,
And also GK: Diprospan
,
Glucocortisone
,
Prednisolone
,
Methylprednisolone
,
Dexamethasone
,
Triamcinolone
.
Antimicrobials and antibiotics
Before conducting a serological test or PCR, the doctor may prescribe broad-spectrum antibiotics. If the patient suffers from the consequences of a specific infection, the doctor chooses a medicine for bursitis that is most effective against this pathogen.
Broad spectrum antibiotics: Doxycycline
,
Tetracycline
,
Rondomycin
,
Ceftriaxone
,
Blicef
,
Ofloxacin
,
Ciprofloxacin
,
Floxal
and others.
Chondroprotectors
As a preventive measure, as well as in case of damage to the synovial bursa, it is recommended to take chondroprotective agents - glucosamine and chondroitin sulfate. They help restore damaged cartilage tissue, strengthen ligaments and tendons, and make the bursa more resistant to stress. This is the only group of drugs that improves the architecture of the joints, promotes the healing of erosive lesions without the formation of adhesions, which impair mobility in the joint affected by bursitis.
It is especially important to take chondroprotectors in case of chronic or recurrent bursitis, as well as in severe cases with purulent complications
.
Long-term use of chondroprotectors improves the quality of synovial fluid, which is a source of nutrients for the entire joint, helps to achieve remission without the use of NSAIDs and GCs and without side effects.
Chondroprotectors are produced in the form of capsules, tablets, injections and ointments. The drug Artracam in a sachet is especially easy to use; it has a pleasant sweetish-lemon taste - it can be diluted in water, and the bioavailability of glucosamine reaches 90-95%. A sachet with a daily dose is convenient to take with you to work.
Other chondroprotectors: Artra
,
Dona
,
Alflutop
,
Chondroitin Complex
,
Movex Active
,
Structum
.
There are several types of drug treatment for bursitis.
Cooling and anti-inflammatory ointments
With a mild course of the disease, external remedies - gels, creams, ointments, balms and compresses - are sometimes enough to cure. In other cases, they are an auxiliary measure that alleviates discomfort in the joint for the patient, reduces pain and swelling. In most cases, drugs for external use provide only a symptomatic effect and do not solve the problem.
.
Ointments for bursitis: Indomethacin
,
Diclofenac
,
Vishnevsky ointment
,
Nayatox
,
Apizartron
,
Ibuprofen
,
Voltaren
,
Ortofen
,
Finalgel
,
Ichthyol
,
Dolobene
,
Capsicam
,
Ungapiven
.
Dimexide are also recommended as an external decongestant.
.
In the presence of hemorrhages and hematomas, it is worth adding Heparin
.