Epithelial coccygeal duct is a congenital defect in the form of a narrow canal in the soft tissues under the skin of the sacrococcygeal region. The passage is located in the fold between the buttocks, and comes out to the surface of the skin with one or more small openings (primary openings). Inside the passage there are sweat and sebaceous glands, hair follicles, and connective tissue fibers. Their waste products exit through the primary openings in the form of secretions, and infection can penetrate into the tissue through these same openings.
In the absence of inflammation, the epithelial coccygeal duct gives virtually no symptoms. Exceptions may include minor discharge from the passage, moisturizing the skin between the buttocks, and itching.
What is the epithelial coccygeal duct?
The epithelial pilonidal duct (ECX, coccyx cyst, coccyx dermoid cyst, coccyx dermoid fistula, pilonidal sinus/coccyx cyst, pilonidal disease, epithelial immersion of the sacrococcygeal region) is a several millimeter wide canal (or cavity) lined with skin.
It refers to inflammatory diseases of the skin and subcutaneous tissue of the intergluteal fold and sacrococcygeal region. This canal is located in the area between the buttocks, above the external opening of the anus (rectum), it goes from the skin deep and ends blindly in the soft tissues. This fistulous tract usually opens on the skin with one or more chiseled holes and, sometimes, contains a tuft of hair. These holes can go unnoticed for a long time, as they often do not have any unpleasant symptoms and only in the event of inflammation they attract attention. Important! If there are painless holes in the intergluteal fold without any additional symptoms, the disease is called asymptomatic ECC (Fig. 1). This form of ECC does not require surgical treatment and requires only careful adherence to basic hygiene rules by the patient himself and periodic examinations by a proctologist.
Figure 1. Asymptomatic course of ECC (the arrow indicates the primary opening without signs of inflammation)
With the development of an inflammatory reaction, which is usually preceded by blockage of the external opening, the epithelial coccygeal tract first manifests itself as a painful compaction on the skin in the area of the intergluteal fold (it is important to know that sometimes, especially in the absence of adequate treatment for a long time, the fistulous tracts can take on bizarre shapes and appear outside the specified area (Fig. 2).
Figure 2. A rare form of EC with the presence of multiple fistulas in the perianal region (arrows indicate multiple secondary fistula openings formed as a result of a long-term chronic form of the disease)
Important! The occurrence of such a form is possible with untimely and/or inadequate surgical treatment.
In the absence of adequate treatment, the pain increases and the compaction turns into a full-fledged abscess (abscess). Then there are usually three options for the development of the disease:
- the abscess continues to grow and forces you to consult a doctor as an emergency;
- the abscess spontaneously drains into the existing fistulous tract on its own, which is manifested by the outflow of pus in the area of the intergluteal fold. At the same time, pain and body temperature gradually decrease and the patient may regard this as a cure and not consult a doctor in the future;
- the skin over the abscess is destroyed by an acute inflammatory process and the abscess spontaneously “breaks” out. After the purulent lesion is emptied, the pain decreases sharply and the body temperature returns to normal.
In the last two cases, significant relief of the condition leads many patients to believe that there is no need for further treatment. However, despite the fact that in most cases the skin wound heals over time, the very cause of the inflammatory process - a purulent cavity with elements of embedded hair - remains in the soft tissues, and the preconditions are created for a new accumulation of purulent discharge and the process is repeated. Important! In any of the variants of the course of the disease, it is necessary to contact a proctologist as early as possible to assess the need for further treatment and exclude more serious diseases in this area.
Symptoms of a coccyx cyst
A small round formation appears in the gluteal fold, 5-10 cm above the anus. Its size gradually increases, and the patient experiences discomfort. Experienced proctologists at the Yusupov Hospital diagnose a coccyx cyst during the examination process, focusing on patient complaints. To confirm the diagnosis, a number of modern instrumental studies are prescribed.
Most often, a coccyx cyst manifests itself in patients with the following symptoms:
- discomfort appears in the gluteal fold, which intensifies with movement;
- swelling occurs in the sacral area, in some cases it is more widespread, involving the perineum;
- the skin in the area above the coccyx becomes hyperemic;
- the embryonic passage opens;
- purulent discharge appears (with a purulent cyst of the coccyx);
- body temperature rises;
- pain occurs when sitting;
- Around the first move, the opening of other, secondary ones may be observed.
Why is ECC formed?
For a long time, the mechanism of the disease remained a mystery to doctors, but in the 50s of the last century an explanation was found for why this disease develops, and it still surprises both young doctors and patients. The intergluteal fold has several features: it is prone to sweating, most of the time it is compressed by underwear and outerwear, and is difficult to reach for independent examination. When walking between the contracted buttocks, a kind of “pumping” effect occurs. Hair caught in the intergluteal fold, under the influence of this effect, penetrates into the thickness of the skin, then into the subcutaneous tissue, where an infected cavity is formed (Fig. 3). This predisposes to the development of a local inflammatory process in the intergluteal fold, which facilitates the possibility of hair penetration into the thickness of the skin.
A)
b)
V)
Figure 3. Mechanism of formation of ECC:
A. Pattern of movement of the buttocks when walking with the formation of a vacuum pump effect
b. Photo of the initial stage of hair penetration into the skin of the intergluteal fold
V. Diagram of the development of the inflammatory process (the arrow indicates the abscess)
What are the main symptoms of the disease? How does ECH manifest?
In approximately half of cases, the disease remains asymptomatic for a long time. The only manifestation may be the presence of one or more holes or dimples in the skin of the intergluteal fold, from which a tuft of hair is sometimes visible.
Important! The absence of other symptoms is often the reason for late detection of the disease, or its discovery as an incidental finding during examinations for other problems.
Microorganisms from the surface of the skin or from the anus area enter the lumen of the skin canal, formed earlier by the introduction of hair, which inevitably leads to the development of chronic, recurrent (repeating) inflammation and the formation of an abscess.
- With inflammation of the ECX, the following symptoms most often occur:
- Pain in the sacrum and coccyx area;
- Redness and thickening of the skin in the area of the intergluteal fold or slightly to the side of it;
- Bloody or purulent discharge from the openings of the epithelial coccygeal duct;
- Increased body temperature;
- The appearance of additional (secondary) holes along or near the intergluteal fold;
- Discharge from additionally formed holes;
- General weakness;
- Inability to carry out normal physical and work activities (Fig. 4).
Figure 4. Abscess of the epithelial coccygeal tract (arrows indicate the primary openings located in the intergluteal fold. The area of the suspected abscess is limited by the orange line)
Basic preventive measures:
- Observe all rules of personal and intimate hygiene
- Rinse the intergluteal fold
- Wear loose, clean, eco-friendly clothing (avoid tight, tight, synthetic clothing)
- Avoid trauma to the coccyx area
- Avoid prolonged sitting
- Epilation and/or depilation in the tailbone area
- Promptly treat and sanitize primary holes, wounds and microtraumas in the coccyx area.
- Immediately contact a surgeon if the first signs of discomfort and inflammation appear
If clinical manifestations or relapse appear, then the only correct preventive measure will be surgical treatment.
Who is at risk for developing ECC?
The disease occurs 4 times more often in men than women. ECC belongs to a group of rare diseases and is detected in only 26 out of 100,000 people. Mostly, young people of working age from 15 to 30 years old are affected. According to statistics, ECC most often occurs in Arabs and Caucasian peoples, less often in African Americans.
Risk factors for the development of ECC are:
- excess hair growth
- overweight
- insufficient attention to hygiene of the coccyx area
- passive lifestyle
- wearing tight and tight clothing (pants, skirts)
What is a relapse of the disease and how to avoid it?
Another form of the disease is relapse (re-development) of the epithelial coccygeal tract, which occurs some time (from 1 year or more) after a previous radical surgical treatment of the epithelial coccygeal tract.
Important! At risk of ECC recurrence are both patients who have previously undergone insufficient surgical intervention, and patients who have developed a disturbance in the healing process of a postoperative wound.
In the event of a relapse of ECC, repeated surgical treatment is indicated, which in turn becomes more complex due to the development of a scar process in the intervention area, the length of hospitalization increases, and the cosmetic effect worsens.
How to diagnose ECX?
The diagnosis of epithelial coccygeal tract is established after comparing the data obtained from the patient and his examination with the results of instrumental examination methods. You will need to tell the specialist in detail about when the first complaints appeared, what changes you noticed in this area before the moment of treatment, remember whether there were any episodes of suppuration and spontaneous opening of the ECX. The doctor will definitely examine the intergluteal fold and the adjacent gluteal region. In some cases, with a widespread process or an atypical course of the disease, a digital examination of the rectum may be necessary. Treat this simple study with understanding, because it is important for us that the diagnosis is made correctly.
Instrumental studies provide great assistance to doctors in establishing a diagnosis and determining the extent of the process, especially with regard to the abscess course of ECC and recurrent forms of the disease.
Instrumental methods include:
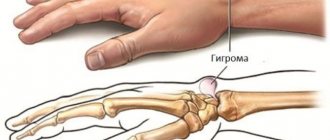
1. Ultrasound of soft tissues of the sacrococcygeal region. This diagnostic method allows you to assess the size, extent of the process, the presence of connections between purulent cavities, and identify deep-lying abscesses, the identification of which by inspection and palpation of this area is impossible. Ultrasound allows the surgeon to determine in advance the scope of surgical intervention and plan a method for closing the skin defect after removal of the ECC (Fig. 5).
Figure 5. Ultrasound picture of the epithelial coccygeal tract in the projection of the intergluteal fold (ultrasonic examination of soft tissues, directly under the skin, in the thickness of the subcutaneous fat, reveals a heterogeneous formation measuring 25x32 mm with smooth, clear contours with inclusions)
2. Fistulography - introducing a contrast agent into the formed tract and performing an X-ray examination. This method allows you to determine the direction of the purulent tracts, their connection with the primary tract and allows the surgeon to also plan the operation in more detail.
In some complex cases, additional examinations may be necessary:
- Anoscopy is an examination of the anal canal using an anoscope, a special optical device for painless examination of the final section of the digestive tract. This study allows you to visually evaluate the mucous membrane of the rectum and anal canal. Anoscopy in most cases is necessary for differential diagnosis of EC with diseases of the anal canal and rectum.
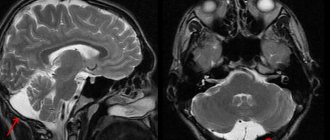
- MRI (magnetic resonance imaging) of the pelvic organs is a study that allows you to obtain a detailed image of the area of interest in various projections, in particular the pelvis and sacral area. This method is more expensive compared to ultrasound, but allows an accurate diagnosis in complex cases of ECX, with relapses of the disease, and the presence of concomitant diseases.
Additional studies will help specialists distinguish complex rectal fistulas from neoplasms of the sacrum and soft tissues of the sacrococcygeal region, disorders of embryonic development, if ultrasound examination is not enough to make a diagnosis (Fig. 6).
Figure 6. MRI image of a complicated epithelial coccygeal tract (MRI in the lateral projection reveals a change in the subcutaneous fat layer at the level of the sacrum and coccyx with the formation of a cavity)
Establishing diagnosis
The coccygeal cyst progresses quite quickly, then the inflammatory process covers an increasingly larger area of soft tissue, and complications develop. Therefore, it is recommended to start treatment as early as possible. When the first symptoms of the disease appear, you should consult a proctologist.
Important. It is not difficult to identify a coccyx cyst; the main thing is to accurately determine its location. After all, often abnormal holes do not coincide with the source of formation.
At an advanced stage, when the formation has already festered and accumulations come out of the canal, it is quite simple to make a diagnosis. However, sometimes a doctor may prescribe an x-ray to distinguish a coccygeal cyst from similar diseases, for example, coccyx osteomyelitis, paraproctitis (formation of pathological canals between the rectum and skin due to suppuration).
In the early stages, the following instrumental diagnostic methods are used to detect a tumor:
- X-ray of the pelvis.
- Computer or magnetic resonance imaging.
After making a diagnosis, the doctor draws up a treatment strategy.
How to distinguish ECC from other diseases?
Some other diseases may have manifestations similar to ECX, which requires differential diagnosis.
Furuncle
A boil is an inflammation of the soft tissue around the hair follicle. First, thickening and redness of the tissue around the hair appears. Then a white rod is formed, around which a zone of hyperemia is preserved. An ECC abscess may be similar to a boil, but a distinctive feature will be the presence of primary openings in the intergluteal fold (Fig. 7).
Figure 7. ECC with a developing abscess (the arrow indicates the primary opening. The area of the forming abscess is limited by the orange line)
Rectal fistula
The external fistula opening is most often located on the skin next to the anus (on the perianal skin). If there is an internal fistula opening, which is located in the anal canal, it can be determined using a digital examination of the rectum or fistulography. With ECS, there is no connection between the tract and the rectum, which is confirmed by probing and or MRI examination, and upon external examination, the primary openings of the coccygeal tract are noticeable.
Presacral teratoma
Presacral teratomas may have a so-called embryonic duct, which opens on the skin near the anus in the form of an epithelialized funnel. Presacral teratomas are located between the posterior wall of the rectum and the anterior surface of the sacrum, which can be determined by digital examination. At the same time, the epithelial coccygeal duct is located under the skin on the posterior surface of the sacrum and coccyx. The final method to accurately make a diagnosis in such cases should be MRI.
Infected wound
A simple infected wound in the area of interest may occur if the patient has had a sacrococcygeal injury, surgery for a rectal fistula, or excision of the epithelial coccygeal duct. In this situation, the presence of primary ECX openings, data on the course of the disease, and the availability of information about any interventions in the specified area are also of fundamental importance.
Treatment of coccyx cyst (preoperative examination, preparation, operations)
Treatment of coccyx cyst is surgical.
To clarify the diagnosis and exclude other pathologies (rectal fistulas, presacral teratoma, osteomyelitis), an examination of the rectum is necessary; in some cases, radiography, colonoscopy or irrigoscopy may be required. Before surgery, thorough depilation of the surgical field is very important and cleansing enemas are required. In case of abscess of a coccyx cyst (festering epithelial coccygeal duct), acute inflammatory phenomena or exacerbation of a chronic process, the first stage is to drain the purulent contents of the cyst (open, drain). The abscess is opened urgently with a small incision under local anesthesia. The cavity is emptied, sanitized with antiseptic solutions and drained. After the drainage of pus, relief occurs. Bandages with water-soluble ointments (levomekol) are applied. The pain goes away, the inflammation subsides, and the postoperative incision wound heals. A period of imaginary well-being begins (full recovery does not occur). A focus of dormant chronic infection remains. Without the second stage - radical surgery (complete excision or removal of the coccyx cyst), as a rule, suppuration is repeated again and again. With a long delay of radical intervention, inflammation can become chronic with the formation of new infiltrates and secondary fistulas.
Primary radical surgery (uncomplicated coccyx cyst) or the second stage of treatment after the subsidence of acute inflammatory phenomena during the period of remission (“cold period”) is carried out as planned. The operation is performed under local infiltration, spinal anesthesia or intravenous anesthesia. Surgical intervention consists of removing (excision) the pathological formation (cyst, canal, tract) along with the internal lining, the contents of the cavity, the surrounding tissues that have changed after repeated inflammatory processes to the fascia. All primary and secondary holes (holes, fistulas) are also excised. To minimize the risk of relapse, all passages and fistulas must be painted with a special dye. After excision of the coccyx cyst, the postoperative wound is usually sutured tightly. Donati sutures are applied to ensure good bleeding control and accurate alignment of the wound edges.
In a number of clinics, the postoperative wound is left open or the edges of the wound are sutured to its bottom for secondary healing (marsupilization). In our opinion, this tactic of postoperative wound management has many disadvantages:
- traumatic
- decrease in the patient's quality of life
- possible secondary infection
- high probability of relapse
- vicious postoperative scars after secondary healing
Is it always necessary to treat ECX?
The determining factor in choosing a treatment method for ECC is the form of the disease. An incidentally detected asymptomatic form of the disease does not require immediate urgent surgical treatment. In order to prevent the development of acute inflammation of the pilonidal cyst in the asymptomatic form of the disease, it is necessary to carry out daily hygiene measures, avoid traumatic effects on the area of the EC and wearing tight and tight clothing, and remove hair (using periodic shaving or hair removal) in the area of the intergluteal groove and buttocks. However, such preventive measures do not guarantee the absence of complications from ECX.
In the initial stages of the formation of an ECC abscess (infiltration stage), when the first symptoms just begin to appear (increasing pain in the area of the sacrum and coccyx, tissue swelling in the area of the intergluteal fold, a slight increase in temperature), it is possible to stop the inflammatory process by using antibiotics and removing the embedded tuft of hair.
Important! Even if the symptoms are not pronounced and develop slowly, it is necessary to consult a specialist as soon as possible to rule out more dangerous diseases and properly plan treatment!
Treatment should only be trusted to an experienced specialist, since it is not always easy to find the line between an abscess (this condition requires mandatory surgical treatment!) and the so-called infiltrate, when surgical treatment is ineffective. Sometimes visual inspection and palpation are not enough to determine the stage of the inflammatory process. Then an ultrasound examination of soft tissues comes to the aid of the specialist, which makes it possible to determine further treatment tactics.
Important! In all more severe cases, with other forms of the disease, surgical treatment is indicated.
If an acute abscess occurs, urgent surgical treatment is indicated, which is aimed primarily at evacuation of pus and rapid relief of the patient's condition.
How to get rid of EKH forever?
The main radical method of treating ECC, that is, a method aimed at completely removing the source of the inflammatory process, is surgical. Depending on the extent of the disease, various types of surgical interventions are performed. There are more than 50 different techniques for treating ECC. Such a large number of possible methods of surgical treatment is due to the fact that currently there is no optimal method that could be called the “gold standard” of treatment for all patients with ECC. In each case, the choice of surgical intervention technique must be individual: several factors must be taken into account - the clinical picture of the disease, the stage of the disease and the extent of the lesion, the possibility of temporary limitation of physical activity in the postoperative period.
Important! After some surgeries, it will be necessary to strictly avoid sitting for 2-3 weeks to allow the wound to heal properly. This must be taken into account when agreeing on the method of surgical treatment with the doctor. The doctor can always suggest several alternative methods.
A specialist who knows and uses in his practice several of the most effective techniques will help you choose the best method.
Provoking factors for the appearance of coccyx cysts
The likelihood of developing a coccyx cyst increases significantly in individuals under the influence of the following factors:
- low physical activity;
- sedentary work;
- frequent diseases, especially infectious ones;
- increased hair growth;
- tendency to form boils;
- small pores, easily clogged with sebum;
- frequent hypothermia of the lower body;
- reduced immunity;
- contact of the buttocks with rough clothing rubbing their skin.
What operation is performed in case of an abscess (acute suppuration) of the EC?
In the event of an acute ECC abscess developing, in most cases, two sequential operations will be required. Treatment of a purulent focus of ECC should be carried out in a specialized coloproctology hospital. Its main goal is to ensure complete evacuation of purulent contents, stop inflammation in the surrounding soft tissues, and prevent further spread of the purulent process.
Important! Even such a simple step as opening an ECC abscess can significantly complicate the second (main) surgical intervention if simple rules are not followed.
The incision should be small and located as close as possible to the midline (intergluteal fold). During the second operation, the scar from the previous incision will need to be removed en bloc with the main volume of ECC tissue. The larger the primary scar, the more tissue will need to be removed during the second operation. At the same time, you should not make too small an incision, since the key to successful recovery is adequate drainage of the purulent-inflammatory focus (Fig. 8).
a)
b)
Figure 8. Stages of surgical treatment of ECX abscess:
a) local anesthesia
b) an incision above the place of greatest fluctuation and evacuation of purulent discharge with the collection of material to determine the microorganism that caused the inflammation.
Correctly performed opening of an abscess leads to the disappearance of pain, temperature and improvement of well-being. However, the final inflammatory processes (changes in the surrounding tissues) after the first stage of surgery (opening and draining the ECC abscess) usually subside within 1-2 weeks.
After successful completion of the first stage of surgical treatment, which will be accompanied by a decrease in the manifestations of acute inflammation and, in fact, is a “symptomatic operation”, it is no less important to carry out the second stage - a radical operation aimed at complete removal of the pilonidal cyst with the affected area of skin and subcutaneous fat. fiber and the subsequent plastic stage to achieve a good cosmetic result.
Important! In case of acute inflammation, two-stage treatment is the most effective and quickly leads to restoration of ability to work. Despite the improvement in the condition after opening and draining the ECC abscess, it is extremely necessary to perform a second radical operation, since each subsequent inflammation will involve an increasing amount of unchanged tissue in the process!
With a small size of the purulent focus and a high level of professionalism of the surgeon, one-stage radical treatment of acute ECC is sometimes possible.
Long-term inflammatory changes lead to persistent pain and long periods of disability, impaired quality of life, complications and relapses after the second stage of surgical treatment, and complicate radical surgery. It is optimal to perform a second (radical) operation 3-4 weeks after opening and draining the ECC abscess.
Classification according to ICD 10
Pilonidal cyst in the international classification of diseases ICD 10 is coded:
- L00-L99 class 12 - Diseases of the skin and subcutaneous tissue.
- L05- Pilonidal cyst.
- L05.0 – Pilonidal cyst with abscess.
- L05.9 - Pilonidal cyst without abscess.
- L00-L08 - Infections of the skin and subcutaneous tissue.
What operations are performed for chronic and recurrent forms of ECC?
Currently, there are a large number of different radical operations to remove ECC, each of which has its own advantages and disadvantages.
All types of surgical interventions can be divided into 2 large groups:
- Minimally invasive techniques.
- Radical surgical treatment with suturing of the wound tightly.
Minimally invasive techniques
Minimally invasive techniques include, for example, sinusectomy and laser destruction of the EC. The advantage of these techniques is that after their implementation there is no significant restriction of physical activity; a return to work is possible on the same day after the surgical intervention. The disadvantage is: the possibility of performing it only with small sizes of ECX (the choice of volume and possibility of execution is determined by the doctor after the ultrasound performed).
a) Sinusectomy
If the patient has only primary passages, as well as in the absence of leaks and additional passages or branches, according to additional examination methods, it is possible to perform a minimally invasive operation - sinusectomy. This operation involves a very economical excision of the epithelial tracts using a scalpel, leaving skin bridges between the primary tracts. This allows you to return to work as quickly as possible, obtaining an excellent cosmetic result (Fig. 9).
a)
b)
Figure 9:
a) type of postoperative wound after sinsuectomy
b) appearance of the postoperative scar 3 weeks after sinusectomy
b) Laser ablation of ECX (diode laser)
The essence of the operation is to process the primary passages of the ECX using a laser. This allows you to destroy the ECC passages and prevent the development of complications of this disease. The operation uses a laser with a specific wavelength in continuous mode. During ECC, the laser beam is delivered using an LED (Fig. 10). The laser power can range from 1.5 to 3 W. The total duration of work ranges from 5 to 25 minutes and depends on the stage of the disease and the length of the coccygeal tract. Due to the ability to concentrate its effect only on the affected tissues, the procedure is minimally invasive and is accompanied by minimal pain. In addition, the laser has a coagulating property, thereby minimizing the possibility of bleeding from the affected vessels.
Figure 10. Laser ablation of ECC tracts
Radical surgical excision with suturing of the wound tightly
This operation, perhaps the most common in Russia, involves a more extensive excision of the epithelial sinus/course with plastic surgery of the defect using local tissues. There are many opinions about how effective and safe this operation is. In the hands of an experienced surgeon, as a rule, the probability of relapse with this type of intervention does not exceed 3-5% and is easily tolerated by patients. The main negative aspect of this technology is the need to limit mobility and eliminate sitting after surgery for a period of several days to several weeks.
The type of surgical intervention is finally determined after examination and receipt of ultrasound results of the soft tissues of the sacrococcygeal region and, if necessary, additional examination methods.
Reviews
In most cases, patients manage to cure a coccyx cyst without problems. However, for this you need to decide on surgery. Those patients who are afraid of surgical intervention only increase their chances of developing complications, because conservative methods will not help cure the pathology.
Oleg, 28 years old: “I suffered from a coccygeal cyst for about 5 years. Only after it burst did I decide to see a doctor. After drainage and dressings, I was scheduled for surgery under local anesthesia. The procedure took about 40 minutes, I did not feel any discomfort. After 3 days I was discharged, at first I was a little bothered by the pain from the wound after the operation, which soon went away. I fully recovered after 3 weeks. For the first 1.5 weeks I tried not to lie on my back or sit on a chair, regularly changed bandages, treated the wound, and went to the doctor. Now I feel great, there have been no relapses, I’m very glad that I decided to have the operation.”
Sergey, 29 years old: “I struggled with the pathology for 2 years: I took medications, made lotions, compresses, ointments, but everything was useless! I decided to undergo surgery, which was performed under local anesthesia. The operation itself was successful, I did not feel any pain. The dressings did not cause pain, and when the stitches were removed, I did not feel any particular discomfort. I recovered within 2.5 weeks. Now everything is fine, the disease is not returning!”
Alexey, 30 years old: “I delayed the operation for a long time, I still couldn’t make up my mind. But when I realized that drugs and folk remedies wouldn’t help, I went to the hospital. A drainage tube was installed in the wound, which remained there for 5 days. During the operation, it turned out that there were already 2 cysts. Naturally, the treatment process was delayed. Therefore, I recommend that if a cyst appears on the tailbone, everyone should not be afraid of surgery. If you wait too long (like me), it will only get worse!”
The main modern modifications of radical treatment of ECX:
Excision of ECX with movement of fasciocutaneous muscle flaps
Our clinic has developed an original technique (patent) involving the creation of fascial-muscular flaps for closing a postoperative wound. The essence of the technique is to move your own soft tissues and create a strong fascial frame (fascia is a strong sheath covering the muscles of our body) in the area of intervention, which reduces the mobility of the wound edges, accelerating healing. It is tension and excessive load on the postoperative wound that is the main factor in unsatisfactory treatment results. This technique allows for the fastest possible recovery of the patient with minimal skin incisions, a low incidence of complications and a good cosmetic result, since the postoperative scar is located in the intergluteal fold and remains almost invisible after surgery (Fig. 11).
A)
b)
V)
Figure 11:
a) primary openings of the ECX, located in the intergluteal fold
b) the type of wound after excision of the EC with subsequent plastic surgery using fasciocutaneous flaps (single interrupted sutures are applied to the wound. The postoperative scar is located in the intergluteal groove, which provides a good cosmetic effect)
c) appearance of the postoperative scar 3 weeks after surgery
Surgery for excision of ECC with Karydakis plastic surgery
In 1976, army surgeon GEKarydakis proposed a surgical technique for radical treatment of the epithelial coccygeal duct. The essence of the operation was that radical excision of all affected tissue occurs from an incision slightly offset from the midline, located next to the intergluteal groove. The operation is accompanied by a small percentage of relapses and postoperative complications. However, its disadvantage is the presence of a postoperative scar outside the gluteal groove, which provides a worse cosmetic defect (Fig. 12).
Figure 12. Scheme of the operation for excision of ECC with Karydakis plasty
Surgery for excision of ECC with Bascomplasty
American surgeon John Bascom proposed two types of surgery for different stages of the disease: in the presence of acute inflammation of the ECX - Bascom I and for radial treatment of the disease - Bascom II. The radical operation proposed by the author is one of the most controversial in the treatment of ECC. The technique involves removing only minor areas of skin (preserving the subcutaneous tissue) containing the primary openings of the ECX. Excision of a large pilonidal cyst, if present, is performed from an incision made away from the median fold.
Figure 13. Scheme of the operation for excision of ECC with Bascomplasty
Marsupilization
Another previously popular method of surgical treatment of ECC is the marsupilization method, which involves excision of the fistula tract en bloc with skin and subcutaneous fat, followed by suturing the skin edges to the bottom of the wound. However, at present this technique is practically not used due to the long rehabilitation period and unsatisfactory cosmetic results (Fig. 14).
Delicate and complex problem
Coccyx cyst (epithelial coccygeal duct) is one of the most delicate and complex health problems.
Those who have dealt with her understand what we are talking about. Coccyx cyst occurs in both men and women. According to statistics, the stronger sex suffers three times more often. The delicacy lies in the localization of the pathological focus. The formation is located in a fairly intimate place (the area of the coccyx, sacrum and intergluteal fold) not far from the anus. Not everyone will easily want to share this with others, even with relatives and loved ones. Not everyone is ready to immediately show the sore spot, discuss their complaints and discomfort, even with doctors. When an epithelial cyst of the coccyx becomes complicated (abscess formation, suppuration, relapse), a person in most cases is deprived of the opportunity to maintain his usual lifestyle and quality of life. Irritating pain, excruciating discomfort, serous or purulent discharge, an unpleasant odor appear, laundry gets dirty, and additional hygiene procedures become necessary. Often it is simply impossible to sit normally. And this is not the whole list of inconveniences.
Many in this situation are forced to give up their usual activities, sports, and even intimate life. All this is depressing. Adding to the delicacy is that a coccyx cyst clinically manifests itself more often in adolescence or puberty. Teenagers are known to be especially sensitive to such problems, although they will try their best not to show it. Wise advice, understanding, help and timely consultation from a surgeon are especially important for them.
The complexity of this pathology lies in the fact that very often there are relapses (repeats) after improper preparation for surgery, an insufficiently radical operation (incomplete removal of cysts, fistulas and leaks), inattentive management in the postoperative period, failure to follow doctor’s recommendations, ignoring basic hygienic procedures and other reasons. Some people have to undergo surgery for coccyx cysts not once, not twice, but multiple times. You won’t believe it, but there are still people who suffer all their lives due to relapses. This reduces the quality of life and is certainly a tragedy. It shouldn't be like this!!!
It is necessary to initially take this disease and the initial operation very seriously. Agree, no one wants to have multiple surgeries. However, repeated surgical intervention should be taken no less seriously, and perhaps more seriously, if the clinical situation has recurred. It is very important to prevent chronicity and continuation of the sluggish process. A coccyx cyst is not a very common and not at all an ordinary problem. The choice of clinic and doctor is extremely important to minimize the risk of relapse. Consultation and surgery with a qualified surgeon who has experience in treating this pathology is necessary.
Skin grafting after radical surgical treatment of ECC
The main problem of wound healing after excision of ECC is the presence of a wide soft tissue defect. The subcutaneous tissue in the sacral area is tightly fixed to the underlying aponeurosis and fascia, therefore, when closing the defect with the remaining soft tissues, tension is created, which is accompanied in the postoperative period by a high risk of divergence of the wound edges and prolonged healing.
The problem of closing the resulting defect with local tissues with plastic skin flaps is especially important in chronic and recurrent forms of the disease.
There are various shapes and types of skin-subcutaneous flaps (Z, VY-shaped, Limberg-flap) for closing the defect that arose after removal of the ECC. The possibility and necessity of using one or another type of plastic surgery is determined by the doctor based on examination data, the characteristics of the operation, the volume of tissue removed, and the patient’s wishes.
Figure 14. Options for closing a postoperative wound defect after excision of the ECC:
a) plastic surgery according to Limberg
b) Z-shaped plastic
How to choose the right clinic and surgeon for treatment in my case?
To summarize the review of surgical treatment methods, it should be said that the choice of the type of operation is undoubtedly the prerogative of the surgeon, but today this decision is made together with the patient. When discussing the plan of surgical intervention (the scope of surgical intervention) specifically in your case, the surgeon should offer you various modern instruments (devices) necessary for the operation, while telling you the advantages and disadvantages of their use. If, in a conversation with you, the surgeon does not try to discuss different approaches to treating your specific ECC, but offers a non-alternative method, then this often indicates that there is no place for other methods in his arsenal.
In such a situation, you have the right to consult another doctor for a “second” opinion. It is necessary to be especially careful when choosing both a surgeon and an institution for surgical treatment in cases where there is a complex or recurrent ECC, when treatment often involves extensive excision of tissue in the sacral area.
Conservative treatment
Many patients who are faced with the disease are interested in the question of whether a cyst can be cured without surgery. The method of therapy depends on the form, type of pathology, and location of the formation. First of all, the doctor must identify the cause of the formation. If its development is caused by a bacterial infection, then it must be removed and cleaned. If the inflammatory process develops after injury or hypothermia, then at the initial stage the patient is prescribed anti-inflammatory drugs. But in any case, the decision on the choice of therapeutic technique is made solely by the doctor.
Medications can help relieve pain and inflammation
Treatment of the cyst with conservative methods will be appropriate in the early stages of its development. The following medications may be used during therapy:
- Antibacterial drugs, for example, Levomycetin, Doxycycline, Kefzol.
- Corticosteroids, for example, hydrocortisone.
- NSAIDs (nonsteroidal anti-inflammatory drugs): Ibuprofen, Aspirin, Diclofenac, Ketoprofen, Piroxicam.
These medications help fight bacteria, relieve inflammation, and relieve pain. However, they will not help stop the development of education and completely cure the pathology.
Important. For coccyx cysts, it is recommended to undergo surgery as early as possible to avoid further spread of the inflammatory process and the development of complications.
If the patient does not have the opportunity to urgently consult a doctor, then a coccygeal cyst can be treated at home using the following folk remedies:
- Pour 1 tbsp. l. calendula 220 ml cold water, put on fire, boil for 3 minutes. Then remove from the stove and leave covered for 30 minutes. Soak gauze or a clean cloth in the broth and apply to the affected area. After 4 hours, remove the compress and apply a new one.
- Soak a napkin with an alcoholic infusion of propolis and apply it to the area of suppuration. Change the compress every 3 hours.
- Mix 1 tbsp. l. tar and 2 tbsp. l. butter. Treat the inflamed area with the mixture before going to bed, cover it on top with cling film, and secure with a bandage. In the morning, wash the skin around the inflammation with warm boiled water.
- Mix toothpaste and pine tree extract, lubricate the sore spot with this product if intense pain occurs. After 3 minutes, the mixture should be rinsed off and gently wiped with a clean, soft towel.
These remedies will help temporarily relieve pain during an acute inflammatory process.
How should you prepare for surgery?
The night before hospitalization for surgical treatment, it is necessary to shave the sacrococcygeal and, if necessary, the gluteal region. It is possible to perform laser (Alexandrite or diode laser) or photoepilation a few days before hospitalization. However, the last two methods are ineffective for removing light hair. Another method of hair removal is electrolysis; it is more painful, but is suitable for all hair types. The effect after the procedures may not be achieved immediately, so it is better to perform them in advance - 14 days before the operation. Shaving, as an alternative to hair removal, will take you less time and money, but at the same time it may damage the skin, which can become a source of infection. No other special preparation is required for the operation; it will be enough to refuse food and liquids 8 hours before the operation.
What to do in the postoperative period?
The period of time required for complete recovery after surgery is usually no more than 3 weeks, but in rare cases it can reach 1 – 3 months. The duration of the period of incapacity rarely exceeds 21 days, and the use of modern surgical technologies makes it possible to transfer the operated patient to outpatient follow-up treatment already 1-2 days after surgery. You need to be prepared for the fact that after surgery, a drain will be installed in the area of the postoperative wound for several days to actively remove discharge from the wound for several days. In the hospital, and then on an outpatient basis, you will undergo dressings to monitor wound healing. The attending physician and medical staff will tell you in detail what work and rest regime should be followed in the immediate postoperative period. In rare cases, antibacterial drugs will be prescribed for a few days. It may also be necessary to monitor wound healing using ultrasound.
Are there ways to prevent relapses/recurrences of the disease?
Despite the radical nature of the operations, there is always a risk of relapse of the disease. To reduce this risk it is recommended:
- compliance with the rules of personal hygiene and features of postoperative wound care, which will be announced by medical personnel;
- shaving the sacrococcygeal area for 3 months after surgery;
- limiting sitting for 2 weeks and intense physical activity for 2 months after surgery.
- timely visits to the attending physician in the early postoperative period
Complications and consequences
If the process is severe, the following complications may develop:
- relapse
- coccyx osteomyelitis (purulent bone lesion)
- fistulous pyoderma (purulent skin lesion)
- fungal infection
- multiple communicating purulent fistulas and pathological tracts with epithelial lining (sacrococcygeal region, perineum, scrotum, inguinal folds, anterior abdominal wall, anus)
Complications require painstaking, lengthy, often multi-stage treatment. Competent prevention, the right choice of clinic and doctor, timely treatment, radical surgery, and compliance with all recommendations will help you avoid such problems.