The color of a healthy person’s stool normally varies from light brown to dark; a change in shade indicates that some pathological process has begun in the human body. The presence of bilirubin and bile pigments is responsible for the color of feces. Sometimes the color of stool changes due to the characteristics of the food consumed; usually this deviation returns to normal in a day or two. In most cases, orange-colored stool indicates problems with the gastrointestinal tract and digestive system.
Norm and pathology
In normal condition, feces are a small sausage, the size of which can vary from 10 to 20 centimeters. The stool should be uniform brown in color and soft in consistency. There should be no blood or pus in the stool, but mucus in small quantities is considered acceptable. The nature of the feces of different people may differ from normal standards, this is due to a person’s food preferences and depends on the amount of food and water consumed per day.
Deviations from the norm are considered to be the presence of impurities such as blood, pus, and foam in the stool. A sharp change in the color of stool and its consistency may indicate the development of a pathological process in the body.
Discolored stool
Hepatitis
51808 August 25
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. The color of stool depends on the amount of bile pigments (products of the breakdown of hemoglobin), coloring substances contained in food and medications, admixtures of fresh or clotted blood, and metabolic products of microorganisms living in the intestines.
In the absence of strongly coloring food pigments, the color of stool is normally light to dark brown.
Stercobilin, a breakdown product of bilirubin, gives stool its brown color. A change in the color of stool from light green to yellowish-gray can occur with various diseases.
If bilirubin does not enter the gastrointestinal tract for any reason, the stool will become discolored. Such feces are called acholic. Discolored stool can have a different consistency, which is determined by the amount of water consumed, plant fiber, intestinal tone and other factors. These factors are taken into account when diagnosing liver diseases.
Possible reasons
Damage to the hepatic and bile ducts
.
If the patency of the hepatic ducts is impaired cholestasis
, which is characterized by acholic feces. Cholestasis can be caused by blockage of the ducts with small stones (cholelithiasis), blood clots, parasites (with opisthorchiasis, fascioliasis, clonorchiasis), and can also be a consequence of congenital anomalies, cicatricial stenosis, and the presence of tumors of the bile ducts. The lumen of the common bile duct may be narrowed due to tumor growth, due to inflammation and cysts of the pancreas, recurrent cholangitis, lymphadenitis due to tuberculosis, sarcoidosis, or be a consequence of surgical treatment and adhesions. In all cases, the flow of bile from the liver is impaired.
Symptoms of cholestasis are: skin itching, jaundice, discoloration of stool and dark urine; severe cases are manifested by a flu-like condition (chills and fever).
Sclerosing cholangitis
is a pathology that is also accompanied by discoloration of stool due to a violation of the outflow of bile. With this disease, sclerosis of the bile ducts occurs (replacement of healthy organ tissue with scar connective fibers) due to inflammatory processes.
Sclerosing cholangitis in most cases is accompanied by inflammatory diseases of the gastrointestinal tract (ulcerative colitis, Crohn's disease).
Patients develop jaundice of the skin, mucous membranes and sclera, itching, weakness and fatigue, weight loss, impaired motor activity due to limited mobility of the limbs (symptoms of osteoporosis).
Functional disorders of the biliary tract
. Functional dysmotility of the biliary tract - biliary dyskinesia - is one of the most common causes of changes in the color of stool. This is due to a narrowing (muscle spasm) of the lumen of the bile ducts and duodenal papilla, which regulates the flow of bile into the intestine.
Spasm can occur due to hormonal disorders, systemic diseases, pain, or after surgical interventions. In this case, the stool discoloration will not be permanent. The stool becomes light only after spastic attacks, and during the period of resumption of motility of the biliary tract, its color returns to normal.
Considering that the brown tint of stool is caused by bile pigments, any process of disruption of their synthesis or entry into the gastrointestinal tract is accompanied by a change in the color of the stool. Discolored feces do not always indicate illness: with excessive consumption of fatty foods
the usual amount of bile is not enough to process all the absorbed fats, and the feces become light in color.
In some infectious diseases
(cholera, salmonellosis, dysentery),
digestive disorders
(inadequate absorption of nutrients, irritable bowel syndrome), increased intestinal motility leads to the rapid movement of feces, which do not have time to change color.
If discolored feces persistently form, diseases of the hepatobiliary system (liver, gallbladder, hepatic and bile ducts, sphincter of Oddi) should be suspected.
Degenerative-inflammatory liver diseases (hepatitis of various etiologies, cirrhosis) affect the synthesis and metabolism of bile pigments and bilirubin, which is often manifested by uncolored feces.
Damage to liver cells (hepatocytes)
. Hepatocytes that produce bile can die under the influence of many factors.
The infectious nature of liver diseases should be considered first.
hepatitis
viruses enter the blood, an acute infectious disease develops, which is manifested by high fever, nausea, vomiting, heaviness and pain in the right hypochondrium, a yellow coloration of the sclera appears (icterus), urine darkens, and feces become discolored.
When infected with hepatitis B and C viruses,
the process often becomes chronic. The incubation period for hepatitis C can be up to six months, and in the acute period of the disease, symptoms resemble a respiratory infection. Chronic viral hepatitis B and C, if left untreated, can lead to cirrhosis and liver cancer. Hepatitis can be accompanied by cytomegalovirus infection, diseases of herpes viral etiology, infectious mononucleosis (caused by the Epstein-Barr virus).
Currently, alcoholic hepatitis
.
Ethyl alcohol products and its metabolites have a direct damaging effect on liver cells.
The chronic course of alcoholic liver disease ends with massive replacement of hepatocytes by connective tissue with complete loss of their functions. In the clinical picture, the main complaints are heaviness and characteristic pain in the right hypochondrium, which can radiate to the arm, shoulder blade, and lumbar region. Yellowness of the skin develops, the sclera develops, feces become discolored, urine darkens, and signs of encephalopathy appear. In the last stages of alcoholic illness, cirrhosis of the liver, liver failure, bleeding from varicose veins of the esophagus, etc. develop.
Among the toxins that have a destructive effect on liver cells
, include plant poisons (some mushrooms, bittersweet and groundsel juice) and industrial chemicals (phosphorus, arsenic, organochlorines, phenols, pesticides). Many drugs (anti-inflammatory, antiviral, antituberculosis, anticonvulsants) change the functional activity of hepatocytes, which affects the color of stool.
Liver cells die due to oxygen starvation caused by circulatory failure and oxygen deficiency in the blood. With hepatic cell failure syndrome, a dysfunction of hepatocytes occurs, which is accompanied by general intoxication of the body.
Diagnostics and examination
For complaints of discolored, acholic stools, diagnosis includes physical and laboratory tests.
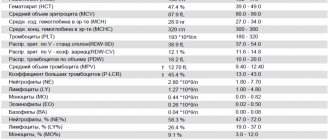
Information about the functioning of the liver and gallbladder is provided by general blood and urine tests; biochemical blood test (aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, bilirubin, glucose, amylase and lipase).
Possible causes of orange colored stool
The causes of orange stool in adults may be due to the following factors:
- Excessive consumption of foods that contain large amounts of carotene. These products include: broccoli, carrots, apricot, pumpkin.
- The use of certain medications can also stain stool, in particular, we are talking about a drug such as Rifampicin.
- Diseases of the genitourinary system - cystitis, as well as lung diseases can also cause orange-colored stool.
- Sometimes the reasons for feces turning orange are diseases such as celiac disease, Gilbert's syndrome, and escherichiosis.
- In addition, cirrhosis of the liver, hepatitis, problems with the pancreas and cholelithiasis are the cause of orange-colored stool in adults. In the presence of such pathologies, the patient may also have other signs, namely: pain in the abdominal cavity, the skin and mucous membranes become covered with a yellow tint. The patient has a high body temperature, nausea, vomiting, the stomach is swollen, and the appetite almost completely disappears.
Orange-colored stool due to problems with the stomach or intestines
As mentioned above, the stool is colored by gastric juice (bile). If the stomach and intestines function without deviations, then bile will color the feces in a “standard” brown shade. If a lack of gastric juice has formed in the intestines, this means that the body does not produce a special bile pigment and the production of enzymes is disrupted. Diseases with similar symptoms: hepatitis, liver cirrhosis. An insufficient amount of bilirubin in the body may be a consequence of the appearance of stones in the liver, cholecystitis, or a malignant or benign tumor.
If the reason for the appearance of orange stool is due to the above reasons, then other signs will also appear:
- pain under the ribs;
- digestive problems;
- unusual, pungent odor from the mouth.
Only a specialist can understand the cause of such symptoms. He should also prescribe you several examinations that will accurately confirm the result. You should not assume that the appearance of orange stool is a completely harmless phenomenon. It's better to play it safe and go to the doctor.
Causes in children
Unlike adults, it is quite common to see orange colored stool in children, and in most cases this is not a deviation from the norm. Orange-colored feces in a baby may be the result of a regular banana eaten the day before. In this case, it does not matter whether the child ate this banana himself or received it from the mother along with breast milk. Older children often eat and drink food products to which dye is added, such as candy, juices and drinks.
Eating low-quality ingredients can cause your baby to have bright orange-colored stool with a liquid consistency, which indicates disorders of the child’s digestive system.
The presence of pus and blood in the stool indicates the development of dysentery or more serious pathologies. In this case, you should immediately consult a doctor.
What else can cause stool to change color to orange?
The following are diseases that rarely cause orange-colored feces, but this can also happen:
| Type of disease | Main symptoms | Treatment |
| Gilbert's syndrome | A disease that is inherited. It is characterized by the fact that bile pigment accumulates in the blood and then directly enters the intestinal lumen. The consequence of this syndrome may be jaundice, and, accordingly, an orange or yellowish coloration of the stool | Eating foods with sufficient fat content. Avoid alcoholic beverages and avoid stressful situations. Phenobarbital is a suitable medication |
| Celiac disease | A disease characterized by physical intolerance to the protein found in wheat, rye and barley. The disease will manifest itself only when the above-described products begin to be included in the diet. After eating them, inflammation of the stomach occurs, which is why the color of the feces changes. | A lifelong gluten-free diet is required. If this does not help, prednisolone is prescribed. If all the above measures are ineffective - hormonal therapy |
Diagnostic measures
Diagnosis of orange-colored stool includes a number of the following measures:
- As with any other disease, to determine the cause of orange-colored stool, it is necessary to conduct a general analysis of stool and urine.
- Advanced stool analysis - coprogram.
- Genetic testing for diseases such as Gilbert's syndrome and celiac disease.
- An ultrasound examination will help to see the condition of the liver and pancreas, as well as establish an accurate diagnosis.
In general, it is not difficult to establish the reason why the stool is orange; the most important thing in this case is to promptly contact a specialist who can accurately diagnose and prescribe appropriate treatment.
Decoding the analysis in adults
Stool analysis helps determine the presence or absence of problems in the gastrointestinal tract. And with a chemical analysis, the presence of salts and protein is determined, acidity, mucus and some other indicators necessary to determine an accurate diagnosis are established.
- Soluble protein. The presence of this substance in the feces indicates that a malfunction has begun in the digestive system, since normally there should be no protein in the feces.
- Starch. This substance, present in feces, indicates a deviation from the norm, since starch must be completely broken down during the digestion of food.
- Muscle fibers. In a completely healthy person, fibers are present in the feces in a modified form, but if they are in an unchanged form, then this indicates a malfunction of the pancreas.
- Leukocytes. In a normal state, a person should not have white blood cells. Their detection and increased number indicate that the patient is developing pathologies of the gastrointestinal tract.
- Connective tissue fibers. This component is the remains of food of animal origin found in feces during defecation. The presence of such fibers indicates that the patient has low acidity, gastritis or pancreatitis.
Treatment
Help before diagnosis
The yellow color of stool, caused by eating habits and observed against the background of normal health, disappears on its own after 2-3 days. In order not to overload the intestines during this period, it is advised to avoid fatty and fried foods and alcohol. If a change in stool color occurs against the background of diarrhea or abdominal pain, you should visit a specialist. To improve your condition, you can drink sorbents. The use of antidiarrheal drugs is undesirable.
Conservative therapy
The yellowish color of stool is caused by various reasons, so the list of therapeutic measures is selected individually. An important stage of treatment is following a special diet, the basis of which is stewed vegetables, lean meat and fish, cereals and soups. In case of chronic pathologies of the pancreas and liver, such a diet must be followed constantly. To treat diseases in which the stool is yellow, the following medications are prescribed:
- Sorbents
. Activated carbon preparations, smecta, are designed to bind and remove toxins from the intestines. Medicines speed up recovery from toxic infections, help cope with diarrhea, and improve digestive functions. - Probiotics
. For dysbiosis, bacterial overgrowth syndrome and side effects of pharmacotherapy, beneficial bacteria are taken that populate the large intestine and promote digestion. For a lasting effect, they are used in courses of at least 10 days. - Enzyme agents
. When the exocrine function of the pancreas is suppressed, drugs containing pancreatic enzymes are used. They eliminate the causes of yellow stools and stimulate the processes of cavity digestion in the small intestine. - Choleretic drugs
. Indicated for hepatobiliary pathology. They improve the chemical composition of bile and ensure its flow into the duodenum, which is required for the breakdown of fats. The color of stool returns to normal within a couple of days after the start of treatment. - Products for rehydration therapy
. All intestinal infections are accompanied by large fluid losses, to replenish which there are oral solutions. They contain the optimal amount of salts and glucose, restore acid-base balance and electrolyte composition.
Decoding the analysis in children
Decoding a coprogram in children is somewhat different from in adults. One of the important indicators is the volume of feces. Thus, an excessively large or small amount of feces indicates that the child is experiencing a disturbance in the functioning of the gastrointestinal tract.
The consistency of the feces is equally important. Pasty stools may indicate colitis, and liquid ones may indicate that intestinal secretion is greatly increased.
The change in the color shade of feces in infants depends on what diet the nursing mother is on. In some cases, stool may change color as evidence that the baby has begun to have intestinal problems, so young mothers during lactation should follow a strict diet prescribed by a doctor.
We're home
On the third to fifth day, the mother’s milk comes in, and by the end of the first week, the baby has fairly stable stools. The literature sometimes says that newborns’ stools are “creamy,” and this confuses mothers who begin to suspect that something is not all right with the baby. In reality, the stool of a healthy baby is liquid and not always homogeneous. The normal color of stool is yellow and its shades. You may notice lumps and a little mucus - it's not scary. Do not be alarmed if the baby’s stool has a greenish tint for up to three months due to the immaturity of the liver enzyme systems and the peculiarities of bilirubin metabolism, this condition has the right to exist and also does not require treatment.
Many mothers sometimes experience anxiety because the baby’s stool “suddenly” becomes watery and the child walks around with profuse gases and a sharp sound. Doctors in this case often suspect lactase deficiency. In reality, things usually work out like this. In the period from 3 weeks to one and a half months, the baby has frequent growth spurts, so at certain moments the baby literally “hangs on the chest” to help the mother produce more milk. Over the course of a day or several, the baby requires the breast more often and for longer than before, and the mother begins to suspect that there is not enough milk. As a result, she often begins to shift the baby from one breast to the other, and the baby receives mainly “foremilk”, which comes from each breast at the beginning of feeding. This milk is rich in carbohydrates and proteins, it makes the baby actively grow, but because of this milk the stool is liquid and gassy (sometimes the “result” looks foamy if the baby is held over a potty or basin when he needs to empty himself, and the mother can observe the consistency chair). In this situation, there is no need to panic - you just don’t need to constantly shift the baby from one breast to the other, for fear that he is starving. Give the baby the opportunity to receive hindmilk, rich in fat, which will not cause flatulence and will linger longer in the intestines.
In this situation (when the baby suddenly begins to clearly suck in more milk), the mother may feel unsure of herself and start drinking lactogenic teas. From this, more carbohydrates again begin to flow into her milk and the baby’s stool becomes more liquid and gassy.
Similar problems due to “foremilk” occur in the case of improper attachment to the breast, as a result of which the baby swallows the air and interrupts feeding, or simply cannot receive “hind” milk. The best way out in this situation is to consult with a breastfeeding specialist to correct the latching technique and stop panicking that the baby “doesn’t have enough milk.”
In a word, don’t worry if your baby has problems with stools of this nature. Of course, his intestinal flora is unstable, it is just beginning to establish itself - this will take at least three to four months. Your task is simply to feed the baby on demand and correctly and not to rush to treat him for imaginary diseases.
When should you see a doctor?
If the orange-colored feces remain for a day or two, and, in addition to the change in the color of the feces, there are no more impurities, then this is not a cause for concern.
If this condition lasts more than two days, then in this case you should consult a doctor. The presence of blood or pus in the stool also requires immediate contact with a specialist.
Treatment of the causes of orange stool
If the stool begins to turn orange, the necessary treatment is prescribed by a gastroenterologist in accordance with what caused the changes.
If, during diagnosis, a large number of red and white blood cells are found in the patient, the doctor prescribes anti-inflammatory drugs, as this is the cause of the development of the inflammatory process in the body.
An infectious disease detected during diagnosis requires immediate hospitalization of the patient. The patient is first given medications that normalize the water-salt balance and intestinal microflora, and only after that the doctor prescribes medications that eliminate the inflammatory process, as well as rid the body of pathogenic bacteria. In addition, the patient is recommended a course of restorative therapy.
If gallstones are found in a patient with orange-colored stool, it is recommended to remove them through surgery.
It is important to note that if the color of stool changes in children or adults, you should not wait for time, but should immediately consult a doctor. Except for those moments when there is an exact certainty that the coloring of the feces was caused by some food product from the diet, in this case there is no need to worry, since the situation will normalize by itself.
Stool during intoxication
With an increased content of bile in the body, poisoning may develop. The main signs of intoxication caused by stagnation of bile:
- Vomit.
- Orange diarrhea.
- Yellowing of the whites of the eyes.
- Bitter taste in the mouth.
- Decreased appetite.
- General state of weakness.
Therapy includes:
- To relieve symptoms of intoxication, patients are prescribed adsorbents (Smecta, Activated carbon).
- To restore normal functioning of the gallbladder, the patient needs to take Sorbitol and Choleritin.
- Drotaverine, No-shpa, Papaverine will help reduce painful spasms.
An accurate diagnosis is made after receiving the results of tests of urine, blood, and feces. If the doctor detects a lack of bile, the patient is recommended to take Allohol, Flacumin.
There are several forms of escherichiosis.
| Type of disease | Main symptoms | Treatment |
| Enterotoxigenic type of Escherichia coli | Normal body temperature, diarrhea with odorless orange stool. Goes away quickly, with virtually no treatment | Most often not required |
| Enteroinvasive type of Escherichia coli | A pulling sensation in the lower abdomen, increased body temperature, regular watery stools, muscle pain (krepature) and a constant feeling of weakness | Contact a specialist and follow his further instructions. Usually the doctor does a hormonal culture, thus determining the strain of the pathogen. Probiotics are prescribed - drugs that normalize intestinal microflora |
| Enterohemmarogic type of Escherichia coli | Sharp spasmodic pain in the lower part of the large intestine, diarrhea with orange feces with blood, normal temperature. This is the most dangerous form of E. coli | A gentle diet - slimy soups, porridge with water, stale white bread. Probiotics and enterosorbents can also be prescribed as medications. |