Joints are parts of the body that undergo an incalculable number of movements every day. In this regard, they are susceptible to numerous destructions and various types of inflammatory processes, which have a common name - arthritis.
Arthritis is a generalized, collective name for various types of inflammation localized in the joints. The current clinical picture suggests that arthritis can be either a separate disease or act as a complication.
Types of Arthritis
Arthritis is a disease that is characteristic of people predominantly of old age, however, the clinical picture also occurs in a category of people at an earlier age, in particular, in children and adolescents.
The varying incidence statistics at different ages are explained by the probable causes of the development of joint arthritis, according to which it is customary to distinguish several types of arthritis:
Rheumatoid
It occurs in conditions of frequent failure of the immune system, and therefore belongs to the category of autoimmune diseases. It manifests itself as chronic inflammation of the connective tissues of the body.
Symptoms include:
- symmetrical joint damage;
- the appearance of “nodules” at the folds.
Among the main factors contributing to the occurrence of the disease are:
- heredity;
- past viral diseases;
- allergic reactions;
- other types of arthritis;
- being under constant stress;
- hormonal imbalances.
Reactive arthritis
One of the heaviest varieties. During the development of regenerative processes, inflammation occurs not only inside the joint, but also in the tissues of the digestive system. In addition, it is worth noting that pelvic inflammation can also occur in reactive arthritis.
There are two subtypes of reactive arthritis:
- postenterocolitic (develops as a complication of intestinal infections caused by pathogens of various kinds, in particular Salmonella, Yersinia, Campylobacter, etc.);
- urogenital (develops after suffering infections such as chlamydia, ureplasmosis, etc.).
The main symptoms may be accompanied by additional:
- inflammation of the urinary tract;
- the appearance of cystitis, urethritis;
- tearfulness;
- conjunctivitis.
Infectious arthritis
Inflammation has a bacterial, viral or fungal etiology. It is diagnosed in patients of all ages: from newborns to the elderly.
Infectious arthritis can be:
- bacterial;
- viral;
- fungal-viral;
- parasitic-viral.
In addition to the classic symptoms, you may experience:
- intoxication;
- chills;
- fever;
- elevated body temperature.
The risk group includes people with rheumatoid arthritis, osteoarthritis, as well as those with addictions, diabetes, obesity, etc.
Gouty arthritis
An inflammatory process that occurs due to the accumulation of uric acid in tissues, which destroys the structure of cartilaginous and periarticular tissues.
There are two types:
- primary – is hereditary in nature and makes itself felt in the presence of unfavorable factors;
- secondary – hyperuricemia (increased levels of uric acid in the blood), resulting from a number of diseases or the use of medications.
Symptoms include:
- swelling and swelling of the joints of the limbs;
- redness of areas of inflammation;
- cramping pain syndrome.
Psoriatic arthritis
Inflammatory processes occurring inside the joint provoke a skin disease such as psoriasis.
The etiology of the disease is unclear. The treatment process is one of the most difficult.
Typical symptoms include:
- asymmetrical increase in the size of small joints of the limbs;
- change in skin color;
- lack of mobility of varying degrees;
- the need to take anesthetics.
Factors that increase the risk of developing the disease:
- frequent occurrence of stressful situations;
- abuse of bad habits;
- infectious diseases.
Osteoarthritis
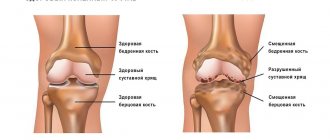
An inflammatory process that affects the cartilage tissue and bones that form the joint. In the process of destruction of cartilage tissue and the body's attempts to restore it, excessive growth of bone tissue occurs, which often leads to direct destruction of the joint.
Symptoms appear slowly, gradually, as the disease develops.
This type of disease often occurs in older people (over 60 years old). Among the factors that increase the risk of disease, it is customary to highlight:
- natural aging of the body;
- excess body weight;
- musculoskeletal injuries;
- hereditary predisposition.
Traumatic (Post-traumatic)
It occurs as a result of previous injuries, not only to the joint itself, but also to injuries/bruises of the periarticular tissues.
The risk group includes people associated with traumatic, physically demanding professional activities, in particular athletes.
Often the disease affects mainly large joints: shoulder, elbow, knee, ankle.
The main symptom is the appearance of crunching in the joints.
The main causes of traumatic arthritis are single and repeated injuries.
Arthrosis
Compared to arthritis, this disease is not an inflammatory joint disease. However, damage to the articular cartilage occurs. The cause may be both involutional changes and injuries or wear of cartilage tissue due to excessive loads. Osteoarthritis can manifest as swelling and pain. Also, in some cases, the disease can lead to changes in other organs and systems. It can lead to both a decrease in range of motion and range of motion. Most often, arthrosis affects the hip joints, knee joints, and spinal joints. Osteoarthritis, an infrequently used term to describe degenerative joint diseases. To understand, it is important to first understand the anatomy of the joint. The ends of the bones that form the joint have a smooth surface called the subchondral bone. Behind this is articular cartilage, which is a strong but elastic connective tissue that protects bones, facilitates movement between surfaces, and also acts as a shock absorber. It is this cartilage that forms the articular surface, and not the bones themselves. The joint has synovial membranes that secrete synovial fluid into the joint space, which lubricates the joint surfaces and acts as a shock absorber. The outer joint capsule provides strength to the joint.
Cartilage is elastic connective tissue. Cartilage cells (chondroblasts) produce and secrete a large number of different substances, such as collagen, into the extracellular matrix. It is this matrix that is responsible for the properties of cartilage, namely its strength and flexibility. Sometimes chondroblasts remain inside the matrix and are called chondrocytes. Cartilage is constantly subject to wear and damage. Cartilage cells constantly replenish the cartilage matrix and thus maintain the integrity of the cartilage.
With age, the ability to regenerate any tissue decreases, but does not stop completely. Even in young people, the body's ability to repair tissue is limited by time. If there is constant and excessive wear and tear on the articular cartilage beyond the time required for repair, then the cartilage will weaken. This is the reason why the disease is more common in older people and more often in those who lead an active lifestyle. There are other factors that complicate regenerative processes, such as inflammatory mediators, which affect normal cartilage regeneration when there is even slight inflammation. Likewise, if there are some medical diseases (such as diabetes) that slow down or stop the activity of cartilage cells, the cartilage gradually wears out. When the cartilage weakens, cartilage ruptures occur, and fragments can float in the joint cavity. Bone tissue is also affected by arthrosis and a condition called osteoarthritis occurs.
Symptoms
Symptoms develop very slowly. In the early stages of cartilage erosion, there may be no symptoms. In addition, arthrosis is a degenerative disease, not an inflammatory condition, and therefore may not manifest itself for a long time. Once symptoms begin, the condition gradually worsens, also over a long period of time. The leading symptom of arthrosis is pain.
The pain is usually isolated to the affected joint. The pain usually worsens during and after movement in the affected joint. In milder cases, pain does not appear during movement, but only some time after exercise. There may also be pain on palpation in the joint area. But pain with arthrosis is usually not accompanied by swelling, as is the case with inflammatory phenomena in the joint (for example, with rheumatoid arthritis).
Joint stiffness is another common symptom. This is most noticeable when waking up in the morning and after a long period of rest. Movement can reduce stiffness, but excessive movement will eventually lead to pain. Joint stiffness tends to get worse over time as the disease progresses. Even when joint stiffness decreases, normal range of motion is not restored. Over time, this leads to a significant decrease in motor activity. The joint may also experience a crunching sound when moving, especially as the disease progresses. Normally, the articular cartilage at the ends of bones rubs against each other, but due to the smooth surface and good lubrication by synovial fluid, this friction does not lead to the appearance of sounds. With arthrosis, the cartilage surface is not so smooth and this leads to the appearance of sounds when moving in the joint (crunching, grinding). Firming – large joints, such as the knees, become firmer to the touch. Bone growths that occur with arthrosis (osteophytes) form over time and can be felt under the skin in the form
Diagnostics
As a rule, diagnosis does not present any particular difficulties and is based on a combination of examination data and instrumental data (radiography, CT, MRI, ultrasound of joints). But given that arthritis also causes changes in cartilage tissue, a careful differential diagnosis of degenerative changes in joints with the consequences of a long-term inflammatory process is necessary. Therefore, laboratory diagnostics are also necessary when diagnosing arthrosis.
Treatment
The disease is more often observed in older people and therefore treatment is most often symptomatic. The key to conservative treatment is to reduce symptoms of pain and improve joint functionality. Drug treatment (for example, NSAIDs) should be prescribed taking into account the concomitant somatic pathology present in older people. A good effect is achieved by intra-articular injection of synovial fluid endoprostheses (Fermatron, Ostenil, etc.), which reduces friction in the joint, improves joint function and reduces pain. Intra-articular administration of long-acting steroids (for example, diprospan) is also possible. Recently, prolotherapy has begun to be used, which consists of introducing substances into tissues that improve the regeneration of connective tissue.
Physiotherapy can quite effectively reduce pain and reduce inflammation.
Exercise therapy. Dosed physical activity allows you to maintain the functionality of the joints, but the loads must be selected carefully, since excess loads lead to increased pain.
Surgery. In case of severe arthrosis of large joints (for example, coxarthrosis or gonarthrosis) and significant dysfunction of the joint and persistent pain, endoprosthetics is recommended.
Arthritis stages
The dynamics of the pathological process suggests the identification of four stages of arthritis:
Stage 1 – the disease practically does not manifest itself, but x-rays of the joints show primary signs of arthritis.
It is characterized by slight stiffness of movement and a feeling of pain when performing various types of loads.
Stage 2 – the progress of inflammation causes the destruction of articular tissues and the formation of erosions on the heads of bones.
The inflamed joint experiences swelling and increased temperature.
Stage 3 – the structure of the joint tissue continues to deteriorate, a visually noticeable deformation of the joints appears, which causes limited mobility and the appearance of pain that accompanies every movement.
There is a partial loss of the functionality of the joint, which is often compensated by tension in the muscle frame.
Stage 4 – the changes that have occurred are irreversible, the inflamed joint loses its ability to move.
If the disease is localized in the knee joints, contractures (tightening, narrowing) are formed at the final stage, and in the hip joints, ankylosis (fusion of the bones of the joint) is formed.
Side by side comparison
Above we described the main causes, symptoms and methods of treating arthritis and arthrosis. In this block we briefly answer the question of the differences between diseases:
| Arthritis | Arthrosis |
| An inflammatory disease that affects the joints and can affect the normal functioning of internal organs. | The disease is degenerative and destructive in nature. It only affects the functioning of the joints. |
| It develops mainly in young and middle-aged people: 25-45 years old. It also happens in children. | It mainly affects older people, as well as people whose activities are directly related to the load on their joints: athletes, musicians, artists. |
| It manifests itself with inflammatory symptoms at the initial stage: pain, swelling, redness and increased temperature in the affected area. | It may not make itself felt for a long time and progress slowly - this complicates the diagnostic process at an early stage. |
Be healthy!
Diagnostics
Have you noticed the presence of several symptoms, but don’t know which doctor treats arthritis? Feel free to seek help from specialists such as a rheumatologist, traumatologist, or therapist (including a chiropractor).
In order to diagnose arthritis of various types, an integrated approach is used, which involves primary and secondary examination of the patient. Modern medicine distinguishes two main methods:
- laboratory (blood and/or immune system testing);
- instrumental (x-ray/ultrasound examination, computed tomography/magnetic resonance imaging, arthroscopy, myelography).
How is rheumatoid arthritis treated?
At the initial consultation, the rheumatologist will prescribe additional examinations - a blood test, x-ray of the joint, ultrasound or MRI. It is impossible to completely cure the disease, so therapy is aimed at relieving unpleasant symptoms and preventing complications.
- Anti-inflammatory drugs relieve inflammation and pain.
- Immunomodulatory - inhibit immune reactions.
With proper treatment, remission lasts a very long time, and sometimes the disease disappears completely, but treatment will take many years. But it is strictly forbidden to massage or warm up joints affected by rheumatoid arthritis. Such manipulations lead to exacerbations.
For rheumatoid arthritis, massage and warming are contraindicated
Treatment of joint arthritis
Only a specialist can determine how to treat arthritis.
The key condition for competent treatment of arthritis of any type is complexity and optimal duration.
Treatment of joint arthritis is prescribed taking into account the diagnostic results, in accordance with current medical standards, in accordance with the scheme developed by a specialist. A number of therapeutic measures are determined by the causes of the disease, its type and characteristics of its course. At the same time, the doctor also takes into account the likelihood of various complications and existing contraindications.
The entire treatment process consists of two stages:
- eliminating the causes of the disease;
- impact on the mechanisms of disease development.
Traditional complex treatment of arthritis involves:
- use of medications of various effects;
- prescription of vitamins;
- use of ointments/gels;
- carrying out physiotherapeutic treatment;
- possibility of surgical intervention;
- organization of therapeutic exercises;
- dieting.
The use of a set of measures ensures effective work aimed at achieving a single goal - curing the patient.
Let's look at the types of treatment in more detail.
Medication
Treatment of joint arthritis with medications is aimed at relieving pain and restoring a normal lifestyle, which includes proper rest, quality work and daily activities without outside help.
To treat arthritis, anti-inflammatory and painkillers are used, as well as chondroprotectors, the key task of which is to restore cartilage tissue.
To eliminate severe inflammation and abscess (formation of a purulent cavity), antibiotics of various spectrums of action can be used.
Physiotherapeutic
Accompanies the phase of reduction of acute inflammatory processes. Using the influence of physical factors makes it possible to significantly accelerate the healing process and achieve stable remission of the disease.
Physiotherapeutic treatment includes:
- laser therapy – promotes activation of local microcirculation and increases local immunity;
- ultra-high frequency therapy (UHF) – promotes the dilation of blood vessels and increases the flow of immune cells to the site of inflammation;
- ultraviolet irradiation – has a bactericidal effect, which increases resistance to viruses and bacteria;
- phonophoresis - involves rubbing hydrocortisone ointment and subsequent exposure to a radiator, which enhances its anti-inflammatory effect and activates blood flow, thereby improving metabolic processes inside the joint;
- Magnetic therapy – normalizes blood circulation and metabolic processes, improving the absorption of medications for arthritis and eliminating inflammation, swelling and pain syndromes, which promotes active recovery.
Diet for arthritis
A balanced diet is the key to successful treatment of any disease. It is for this reason that diet for arthritis is an important condition, the observance of which significantly increases the effectiveness of drug treatment and serves as an excellent prevention of arthritis.
Today, it is customary for experts to highlight a number of general recommendations regarding nutrition for arthritis of the joints:
- Complete cessation of bad habits (smoking/alcohol).
- Balanced, varied diet.
- Reduced calorie content in the menu.
- Increasing the proportion of foods fortified with vitamins (beans, fruits/vegetables, lean meat/fish).
- Compliance with portion sizes, as well as diet (at least 5 times a day).
- Compliance with the drinking regime (1.5-2 liters of water per day).
Proper nutrition for arthritis helps to significantly reduce ongoing inflammatory processes. Following a therapeutic diet for arthritis will improve metabolism and help reduce the amount of uric acid in the body.
Exercise therapy
Therapeutic physical education (PT) is an important component of the complex treatment of arthritis. The systematic use of a set of exercises for arthritis is used to preserve the self-care function and ensure maximum efficiency in restoring joint function during the acute period of the disease.
Among the basic principles of gymnastics for joints, it is worth highlighting:
- tracking blood pressure and pulse levels, pain levels, and the degree of joint swelling;
- smoothness of movements, in conditions of small amplitude of joint movement;
- gradual increase in load;
- regularity of classes;
- MANDATORY consultation with a specialist (coordination of the exercises used).
A well-developed set of therapeutic gymnastics exercises can help achieve stable remission, significantly reduce pain and relieve pathological tension in the muscle frame.
Medicines for arthritis
Treatment of joint arthritis with medications is carried out using drugs of various effects, among which non-steroidal anti-inflammatory drugs (NSAIDs), for example, Artradol, Ibuprofen and Diclofenac, occupy a special place.
If NSAIDs are insufficiently effective, the attending physician may prescribe treatment with hormonal steroids (Prednisolone, Hydrocortisone). It is worth noting that steroid-type drugs can be used both in the form of tablets for arthritis and used as injections and used primarily to relieve inflammation, swelling and pain.
In order to stop the process of cell division, cytostatics (Methotrexate, Immard) can be prescribed, and in parallel with them, antibiotics (Sulfasalazine, Doxycycline, etc.) can be prescribed to destroy pathogenic microorganisms and relieve inflammation.
One of the recommended treatment methods is the use of chondroprotectors, which contain chondrotin and glucosamine, which ensures high-quality restoration of hyaline cartilage (Artracam, Chondra Evalar).
Vitamin therapy involves taking vitamins of groups B (anti-inflammatory and regenerative effect), E (antioxidants) and C (immunity enhancement). Used in parallel with a course of tablets for arthritis.
As additional methods of drug treatment, it is permissible to use local remedies - ointments/gels for arthritis. They may have anti-inflammatory and analgesic effects. Voltaren, Fastum-gel and Capsicam are considered to be the most effective.
To relieve spasms and pain, muscle relaxant drugs are used that normalize muscle tone (Sirdalud, Mydocalm).
It is important to note that taking painkillers for arthritis without consulting a doctor should not exceed 3 days, as this may lead to missing the moment of development of serious complications.
Complications and possible consequences of arthritis
The likelihood of early complications of arthritis in the form of panarthritis (acute purulent arthritis), phlegmon (diffused purulent inflammation) and other processes is possible mainly with an infectious form of the disease.
Late complications usually include:
- contractures;
- pathological dislocations;
- osteomyelitis (purulent-necrotic process of bone or bone marrow);
- generalized sepsis (inflammation).
Lack of proper treatment for progressive arthritis can lead to loss of self-care and free movement - disability.
Classification
Arthritis, depending on the cause and clinical form, is of the following types:
- rheumatoid arthritis associated with malfunctions of the immune system;
- rheumatic, with chronic connective tissue disease with predominant damage to the heart and joints;
- ankylosing spondylitis, or ankylosing spondylitis - inflammation of the joints of the spine;
- infectious, with direct penetration of infectious agents into the joint;
- reactive arthritis - an immune response to a previous infectious disease;
- psoriatic arthritis is a chronic immune-mediated inflammatory disease of the osteoarticular system that develops in patients with psoriasis;
- gouty – occurs due to the deposition of uric acid in the joints;
- inflammation in systemic connective tissue diseases, for example, systemic lupus erythematosus;
- arthritis due to diseases of the gastrointestinal tract, lungs and other organs and systems;
- traumatic, occurring after an injury;
- juvenile idiopathic arthritis in children under sixteen years of age.
Based on the number of joints affected, monoarthritis is distinguished with inflammation of only one, oligoarthritis, if two or three areas are affected, and polyarthritis - a disease of more than three joints.
The process can be acute or chronic. In the first case, it develops rapidly, accompanied by severe pain and inflammation in the tissues. Chronic disease progresses gradually, slowly turning into a serious disease.
Prevention
The best treatment for any type of arthritis is prevention. Preventive measures are primarily necessary for people who are at risk for one of the reasons:
- heredity;
- reduced immunity;
- excess body weight;
- Professional activities involve heavy loads on the joints.
There are two current types of arthritis prevention:
- primary prevention is aimed at preventing the onset and development of the disease, as well as preventing the reasons why it may occur. Involves: timely diagnosis and treatment of various viral and colds;
- quality treatment of chronic infectious diseases;
- the use of measures to strengthen the body's immunity;
- maintaining a healthy lifestyle.
- the use of a course of drug treatment with drugs prescribed by the attending physician;
Timely contact with a professional specialist allows you to promptly identify the disease, determine its degree of development and prescribe the most appropriate treatment.
Self-medication can aggravate inflammatory processes and lead to irreversible consequences, including disability.
Types of arthritic inflammation
This inflammatory disease has two degrees of involvement, according to which it can be systematized: monoarthritis (develops in one joint) and polyarthritis (affects several joints at the same time). According to the rheumatological classification, arthritis is divided into types, some of which can only be determined through tests. Therefore, if you have regular joint pain, do not self-medicate. We recommend contacting the Innovative Medical Center, where experienced specialists, after examination, will give you an accurate diagnosis and prescribe the necessary treatment.
There are these types of arthritis:
- reactive;
- rheumatoid;
- infectious;
- gouty;
- psoriatic;
- osteoarthritis;
- traumatic.
- Knee-joint
- Elbow joint
- Shoulder joint
- Finger joints
- Joints of the hands