Spasm of the gastric muscles when the gastric sphincter is open can cause gas masses to enter the oral cavity, and the taste of the food eaten may be felt. This is due to the release of its undigested particles along with the air. The release of some gastric juice in some cases causes a burning sensation in the esophagus and mouth, as well as a sour taste.
This spasm is called belching. Moreover, the process of regurgitation of food is absolutely normal for recently born children, thus they get rid of excess food and accumulation of gases in the stomach. With the growth of the digestive tract organs, as well as the cessation of breastfeeding, this phenomenon disappears. Although in adulthood, every person periodically experiences belching.
In healthy people, belching is a one-time event and the release of air is not accompanied by unpleasant sensations, since a clean air bubble comes out. A small amount of it is necessary to regulate pressure in the gastrointestinal tract. If too much air accumulates, it comes out without causing us any inconvenience. However, belching can be not only a normal functioning of the body, but also a sign of pathological processes.
Factors causing belching
Belching is a sign of inflammatory processes in the esophagus.
Belching in people who do not suffer from diseases of the gastrointestinal tract, as a rule, is episodic.
The masses released either have a neutral odor, or an unpleasant odor of undigested food is felt. Appears due to:
- active articulation during eating;
- swallowing insufficiently crushed food fragments too quickly;
- eating under stress;
- eating too much;
- Swallowing too much air occurs with food or simply during activity.
In addition, certain types of food can cause active formation of gas bubbles that escape through the esophagus into the oral cavity:
- sparkling mineral water, sweet soda;
- artificially oxygenated drinks;
- milk drinks;
- cold desserts such as ice cream and popsicles;
- dishes with a lot of onions, or excessive consumption of onions raw;
- peas, beans, soybeans and other beans or cabbage dishes also cause belching, although they are more characterized by increased gas formation in the intestines.
Treatment methods
First of all, the doctor is interested in the diet and prescribes an examination to examine in detail the condition of the digestive tract. Modern equipment installed within the walls of our clinic allows gastroscopy to be performed quickly and without pain.
Next, based on the diagnostic results, the gastroenterologist establishes a diagnosis and develops treatment tactics for each patient individually.
Drug therapy involves taking adsorbent, antacid drugs, and anti-inflammatory drugs to combat the inflammatory process of the tissues of the internal organs of the gastrointestinal tract. They create a protective layer on the walls of the stomach, collapse gases, and speed up the process of digesting food. In some cases, the gastroenterologist recommends taking a course of physical therapy to improve intestinal motility.
Treatment of belching is impossible without correcting the diet. So, you need to exclude foods such as cabbage, brown bread, baked goods with yeast, legumes, and carbonated drinks. Along with the main therapy, alkaline mineral water is prescribed to reduce stomach acidity.
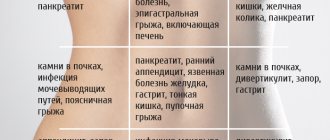
The main diseases that cause belching
First of all, pathological belching is periodic and serves as a symptom of diseases such as:
- inflammatory process in the pancreas;
- inflammation of the gastric mucosa;
- dysfunction of the gallbladder;
- inflammation of the duodenal mucosa;
- stomach ulcer;
- displacement or compression of the esophageal tube;
The appearance of regular belching in combination with an unpleasant rotten smell should be alarming; a lump in the stomach may also be felt. These symptoms are typical for malignant neoplasms.
The process of regurgitation at the end of a meal
Belching may occur after eating.
At the end of a meal, the process of belching can be a physiological norm.
However, in case of disturbances in the functioning of the gastrointestinal tract, belching after eating is also a characteristic symptom; it indicates:
- inflammation of the pancreas in a sluggish and acute form;
- inflammation of the duodenal bulb;
- violation of the patency of the bile ducts;
- inflammation of the intestinal mucosa with a high concentration of acid in the gastric juice;
- inflammatory processes in the esophagus.
Regurgitation that is periodic in nature may indicate disturbances not only in the functioning of the digestive organs, but also some hidden diseases of other systems. Therefore, it is necessary to obtain a conclusion about your health status from your attending physician.
To summarize, we can say that periodic belching occurs due to:
- insufficiently balanced diet;
- irregular eating habits;
- excessively active behavior at the table;
- swallowing large amounts of air;
- dysfunction of the digestive system;
- diseases of other organs not related to the process of digesting food. For example, problems with cardiac activity also contribute to the appearance of belching;
- hiatal hernia.
In addition, there are a number of diseases accompanied by belching phenomena:
- ulcerative lesions in the intestines and stomach;
- insufficient secretion of digestive enzymes;
- reflux of stomach contents into the esophagus;
- disruption of the outflow of bile and the functioning of the pancreas.
Various forms of regurgitation
Belching may have a bitter taste.
According to the form of occurrence, regurgitation can be of a different nature:
- after finishing a meal with a sour taste in the mouth;
- with a hint of bitter taste;
- with the characteristic smell and taste of acetone;
- belching with just air.
Belching is also classified according to the factors causing it:
- sour with a high concentration of acid in the stomach;
- bitter taste, indicating reflux;
- with the smell of acetone or rotten food in patients with diabetes or with stagnation of food residues in the stomach;
- neutral belching without taste or smell - due to poor nutrition, swallowing air, minor problems with the digestive system.
It is necessary to dwell in detail on the origins of the appearance of varieties of belching during pathological processes in the body.
Symptomatic therapy
Episodic erection does not require treatment. To reduce the severity of physiological belching of air, correction of eating habits and diet is sufficient. Frequent, fractional consumption of food (up to 5-6 times a day) with a reduction in the volume of individual portions, and thorough, slow chewing of foods are effective. To reduce gas formation in the stomach, it is necessary to limit or completely eliminate legumes and dairy products, highly carbonated drinks, cruciferous vegetables from the diet, and stop using chewing gum.
Stomach gases are more easily removed into the intestines after short walks, which improve the evacuation function of the stomach after eating. Effective non-drug ways to reduce intra-abdominal pressure are wearing loose clothing without tight belts, limiting the amount of exercise for the abdominal muscles during exercise or training. Sleeping on a high pillow promotes the quiet, imperceptible removal of gases from the gastric cavity.
An increase in the duration of belching for more than an hour, its occurrence for several days in a row, the passage of a large volume of air, the appearance of a sour, bitter or rotten taste, and other dyspeptic disorders are indications for contacting a gastroenterologist. Until an accurate diagnosis is established, herbal decoctions, sedative herbal medicines, agents that improve gastrointestinal motility, and enterosorbents are used to relieve permanent erection.
Sour taste when burping
Belching with a sour taste appears in the following cases:
- reflux of stomach contents into the esophagus;
- gastritis;
- ulcerative lesions;
- oncological diseases.
Diseases of the gastrointestinal tract are always accompanied by belching, and without curing them it is impossible to get rid of this symptom. Patients need to consult a specialist because they may suffer from ulcerative lesions or inflammation of the mucous membrane if:
Regurgitation with a bitter taste
Belching with a bitter taste occurs due to a violation of the outflow of bile masses.
Belching with a pronounced bitter taste indicates:
- disorders of the outflow of bile masses, when bile moves in the opposite direction to the stomach, and not to the intestinal tract. This is due to dysfunction of the pyloric valve and increased pressure in the duodenum;
- damage, neoplasms, displacements, compression of the intestines. In this case, bile is poured into the stomach and enters the oral cavity;
- some medications relax the intestinal muscles and help open the valve between the intestines and the stomach;
- surgical interventions can damage the muscle tissue of the locking mechanism, and bile will constantly leak into the stomach;
- inflammatory processes in the small intestine lead to increased pressure and the release of bile;
- during pregnancy, all abdominal organs are displaced and compressed, which also causes belching;
- in rare cases, a completely healthy person can also belch with bitterness.
Surveys
A gastroenterologist examines patients with complaints of putrefactive erection. Since rotten belching most often indicates the presence of a pathological condition, the diagnostic search is aimed at identifying the root cause of the symptom. The patient undergoes a comprehensive examination to study the morphological and functional features of the digestive and biliary system. The most valuable methods are:
- Sonography
. Ultrasound of the abdominal organs is an accessible non-invasive examination that is prescribed for rapid diagnosis. The method is not accompanied by radiation exposure and makes it possible to detect nonspecific signs of inflammatory diseases and space-occupying formations. According to indications, targeted ultrasound examination of individual organs is performed. - Endoscopy
. Endoscopy is used in the diagnosis of pathology of the upper gastrointestinal tract to identify motility disorders, dysregulation of the pyloric sphincter, and signs of hypoacid conditions. For colonic symptoms, colonoscopy is informative, allowing, if necessary, a biopsy of the affected areas. Video capsule endoscopy is used less frequently. - X-ray methods
. X-ray with oral contrast is used to visualize all parts of the gastrointestinal tract; taking delayed images allows you to assess the speed of passage of contents through the intestines and the coherence of the muscle sphincters. To study the biliary and pancreatic ducts, RPCP and percutaneous cholangiopancreatography are prescribed. - Stool analysis
. Diseases accompanied by rotten erection often cause pathological changes in the feces. The standard coprogram can be supplemented by tests for helminth eggs and an expanded bacteriological study. If neoplasms or ulcerative-destructive processes are suspected, the Gregersen test for occult blood is performed.
Laboratory methods are recommended to clarify the diagnosis; patients may be prescribed liver tests, determination of the levels of pancreatic enzymes in the blood and urine, and measurement of the concentration of gastrin and pepsinogen in the blood. To assess gastric secretion, 24-hour pH measurements are performed.
A patient with complaints of rotten belching undergoes a comprehensive gastroenterological examination
Belching with a characteristic acetone odor
Such belching often occurs in diabetics whose disease is complicated by:
- increased blood sugar levels over a long period of time;
- disorders of nervous activity. In this case, the functioning of the digestive tract is disrupted, muscle arrhythmia occurs, food does not move through the intestines quickly enough, and reflux occurs. In the stomach cavity, food residues can also linger, the fermentation process begins, and a large amount of gases are released;
- dysfunction of carbohydrate metabolism. This dysfunction leads to gastric and intestinal atony, while the mucous membranes are constantly irritated.
Diabetics experience belching and a burning sensation mainly after eating. This may also be accompanied by attacks of nausea. Constant monitoring by an endocrinologist helps alleviate this condition.
This video will tell you about burping and more:
https://www.youtube.com/watch?v=VIvzMoDKgdU
Regurgitation at an early age
In young children, burping is considered normal after drinking milk.
During infancy, regurgitation of breast milk along with some air is a normal physiological process.
A certain amount of air masses enters the stomach during feeding and serves to normalize pressure.
Since the activity of the baby’s digestive tract is not properly regulated, air bubbles can enter the intestines, causing unpleasant pain and flatulence. All this goes away with a belch. Therefore, after feeding, it is recommended to carry the baby in your arms until excess air is released. As you grow older, the need for this disappears.
It is better to rock hyperactive children who cannot calmly suckle the breast before feeding and wait until the baby calms down. You should also interrupt feeding to allow the air to escape. It would not be superfluous to consult a neurologist. Belching in a one-year-old toddler should worry parents. In this case, medical attention is needed.
In young children, the state of the digestive organs directly depends on the stable functioning of the nervous system. Hyperactive children are more vulnerable in this regard. Baby burping can also be caused by:
- active distracting activities during meals;
- watching TV while eating;
- lack of discipline while eating;
- ENT diseases.
School-age children burp for the same reasons as adult patients:
- disruption of the digestive system;
- liver problems;
- violation of the outflow of bile.
Although belching and hiccups are considered normal, they can occur with high frequency or even become constant, annoying and require medical attention. And patients with aerophagia should not undergo exploratory laparotomy. They require other treatment methods.
All about burping
Belching is an audible release of air from the esophagus into the pharynx. The medical term is erection. Almost 7% of the general population complain of excessive or unpleasant belching.
There are two types of it: the so-called gastric and supragastric . The first is the release of swallowed air that enters the esophagus during transient relaxation of the lower esophageal sphincter (TELS). TRNPS is triggered by inflating the proximal stomach and allows air to be expelled from the stomach, thereby acting as a decompression mechanism for the organ and preventing large volumes of gas from passing through the pylorus into the intestine. Thus, TRNPS is sometimes called reflex belching.
Distension of the esophagus caused by refluxed air initiates reflexogenic relaxation of the upper esophageal sphincter (UES), through which air can escape. Gastric belchings occur 25 to 30 times a day and are physiological. They are involuntary and completely controlled by reflexes.
The supragastric form is not a physiological reaction, therefore in all cases it is considered a pathology. Unlike gastric belching, such belching, a common cause of which is an anxiety disorder, is not a reflex and refers to a behavioral reaction. Contraction of the diaphragm creates negative pressure in the chest cavity and esophagus, subsequent relaxation of the IPS leads to an influx of air into the esophagus and is immediately pushed out by voluntary muscle tension.
Often patients seek help for very frequent episodes of belching.
They can occur directly during the examination with a frequency of up to 20 times per minute. Usually, if you are distracted by a conversation, the symptoms stop, then reappear. There are no episodes of belching during sleep.
Etiology
There are several important factors that influence the presence of gas in the gastrointestinal tract. These include the amount of air swallowed and the efficiency with which the gastrointestinal tract moves and expels air or gas. Excessive air entry into the stomach is associated with rapid swallowing of food and drinks, drinking through a straw, chewing gum, sucking hard candy, or wearing unstable dentures. People also take in more air when they are nervous. For some people, excessive burping is a learned behavior or habit.
Air that is swallowed and not expelled by belching passes through the gastrointestinal tract and exits through the anus. In normal people, about 50% of the gas expelled in this way is swallowed air. And this amount can increase significantly in those who ingest it exorbitantly.
Possible causes of gastric belching:
- breathing through the mouth;
- myocardial infarction (rare, but may cause belching with chest pain);
- emotional stress;
- drinking carbonated drinks;
- food intolerance;
- food allergies;
- lactose intolerance (lactase deficiency);
- reduced acidity of gastric juice (achlorhydria);
- diabetes mellitus (diabetic gastroparesis can cause frequent belching);
- occasional belching of offensive intestinal gas is a greater cause than swallowed air: fermentation in the intestines;
- gastroparesis (causes: diabetes type 1 or 2, anorexia nervosa, damage to nerves or muscles caused by surgery or injury, thyroid disease, pancreatitis, scleroderma);
- vagotomy;
- pyloric obstruction;
- peptic ulcer;
- intestinal tumor;
- nervous habit of swallowing air while eating or talking;
- gastrointestinal ulcers;
- gastritis;
- gallbladder diseases;
- pancreatic diseases;
- pregnancy;
- obesity;
- sliding hiatal hernia;
- gastroesophageal reflux disease;
- celiac disease;
- Down syndrome associated with celiac disease.
A number of different medications can cause stomach belching or problems that cause it: drugs for type 2 diabetes (acarbose), laxatives (lactulose and sorbitol), pain relievers (naproxen, ibuprofen, aspirin). Excessive use of painkillers can cause gastritis and, consequently, belching.
Pathogenesis
Normally, air from the stomach enters the intestines. Belching occurs when air enters the esophagus and is pushed out through the mouth. As with gastroesophageal reflux disease (GERD), this process requires the LES to be relaxed to regurgitate up into the esophagus and then audibly through the mouth.
Belching after eating, especially a large meal, can be normal and occur as a result of swallowing air. Relaxation of the LES is facilitated by food, primarily onions, tomatoes, fats, and alcohol.
Chronic belching does not lead to organic disorders. In most cases, swallowed air from the esophagus quickly flows back before reaching the stomach. This becomes a bad habit in some individuals. Magenblase syndrome, an incompletely understood disorder, causes severe bloating and tension in the abdomen from gas in the stomach after eating. These symptoms resolve after belching. Babies and children can swallow large amounts of air without realizing it.
Diagnostics
Belching itself is not cause for concern and does not indicate any serious illness. An examination may be indicated if the symptoms are very unpleasant or there are other associated ones - abdominal pain, vomiting, diarrhea, constipation, weight loss, gastrointestinal bleeding and sometimes heartburn.
Physical examination. It is necessary to make sure that air is regurgitated and belched again. Currently, there are several tests (other than history and physical examination) that are used to further evaluate regurgitation. In such cases, endoscopy may be useful if peptic ulcer disease or GERD is suspected.
Laboratory diagnostics. Low hemoglobin may indicate malabsorption of iron, folate, and vitamin B12. The albumin level provides evidence of hypoalbuminemia, suggesting malabsorption.
If it is necessary to exclude intestinal obstruction, an X-ray examination of the abdomen is performed. Sometimes lactose intolerance should be assessed. Tests are available to screen for celiac disease if other signs suggest the disorder.
Treatment
Patients with intense belching often suffer from decreased quality of life . Therefore, the symptoms must be taken into account and treatment carried out accordingly. However, other than a few anecdotal reports, there is still too little data on the treatment of patients with gastric regurgitation.
It is often recommended to make lifestyle changes, including avoiding fast eating and drinking, chewing gum, drinking carbonated drinks from a bottle, consuming chocolate, onions, hard candy, and alcohol. You should stop smoking.
Patients with GERD may experience a high frequency of gastric belching. However, in this category, supragastric disease was also observed. Patients with GERD swallowed air more often and then had more gastric burps than healthy people (Hemmink GJ et al., 2009). Acid suppressive therapy helps reduce the intensity of this process. This means that the unpleasant sensation of heartburn stimulates patients to take a large and frequent sip of saliva and, along with it, swallow more air. Belching symptoms respond to treatment with the TRNPS inhibitor baclofen (Cossentino MJ et al., 2013). Defoamers, in particular espumizan, do not help with gastric and supragastric belching.
Given that excessive supragastric regurgitation is a behavioral disorder, cognitive behavioral therapy appears to be a reasonable alternative approach (Chitkara DK et al., 2008). Observations support the effects of distraction and stimulation. A small study using baclofen, which reduces the incidence of TRNS, found that the drug reduced the number of supragastric belches (Blondeau K. et al., 2004). Successful treatment of excessive belching has been reported in several cases using hypnosis and biofeedback (Spiegel SB, 1996; Cigrang JA et al., 2006).
Inability to burp
The physiological significance of belching is illustrated by the example of those patients who have an acquired inability to do it. After anti-reflux surgery, a newly placed cuff around the LES prevents reflux by reducing the number of TRIPs and increasing sphincter pressure during relaxation (Bredenoord AJ et al, 2008). As a result, the number of gastric belches is significantly reduced, and in some patients it is not observed at all. Loss of the stomach's ability to ventilate can cause air to accumulate in the stomach and in the intestines, causing bloating and increased flatulence. These symptoms can be very severe and sometimes lead to a second surgery to restore normal anatomy.
Some, to reduce bloating symptoms after antireflux surgery, induce supragastric burping in a futile attempt to expel air. The fact that the patient is said to be able to regurgitate after antireflux surgery cannot be taken as an indication that the ventilatory capacity of the stomach is not impaired. After all, belching can also be caused by the supragastric mechanism. Its incidence has been shown to be lower after partial fundoplication (270 degrees Toupet) than after complete fundoplication (360 degrees Nissen) (Broeders JA et al., 2012).
Very rarely, inability to burp is observed in patients with achalasia. In this case, the neurons that control the motility of the smooth muscles of the esophagus are involved in the degenerative process. This typically results in a lack of peristalsis and an inability of the LES to relax. Air dilatation of the esophagus occurs and patients experience chest pain. Likewise, a high IPS threshold for relaxation can cause chest pain. It has been suggested that regurgitation disorders play a role in some patients with noncardiac chest pain (Gignoux C. et al., 1993).
Read the continuation of the material here.