Intestinal obstruction is a pathological condition leading to disruption of the passage of a bolus of food through the intestines, circulatory disorders, intoxication of the body, and, if the outcome is unfavorable, to necrosis and perforation of sections of the intestinal wall and the death of a person. One of the causes of obstruction is intestinal volvulus - a situation when part of the large or small intestine twists around its own axis or around the axis of the mesentery. Places of torsion become a clamp not only for food mass, but also for nerve fibers, blood and lymphatic vessels.
General information
Intestinal volvulus is the twisting of a loop of any intestine around the axis of the mesentery and its pinching. This condition is classified as strangulating intestinal obstruction . Torsion of the mesentery itself may involve the mesenteric vessels, increasing the risk of intestinal gangrene with subsequent perforation and peritonitis .
If we take into account age, this pathology most often occurs in adulthood and old age. This pathology cannot be excluded in children, especially newborns, which is associated with congenital intestinal pathology and imperfections of the gastrointestinal tract. If we consider localization, then in adults the most common volvulus of the large intestine is the sigmoid colon (in 80% of cases, which is due to the structural features of the mesentery - it has a significant length), the cecum (15% of cases) and the transverse colon (only 3% ), and in children - the small intestine. Inversions can be partial or complete. With complete inversion, the intestinal loop and mesentery are twisted by 2500-3600. In rare but severe cases, there may be double or triple torsion and the formation of knots. This condition is acute and requires urgent intervention.
What it is?
Volvulus is an acute intestinal obstruction that begins to progress due to rotation of the intestine around the mesenteric axis. This can also occur due to twisting of a certain section of the intestine together with the mesentery around the axis (the process is accompanied by severe circulatory disorders).
Most often, this pathology is diagnosed in children under one year of age. This is due to the fact that their peristalsis has not yet fully normalized, so some part of the small intestine may enter the large intestine.
Pathogenesis
Congenital anomalies of intestinal rotation and fixation develop in the first 3 months of pregnancy and fetal development. First, the embryo's primary intestine protrudes from the abdominal cavity, and from the sixth to tenth week the intestine rotates, returning to the abdominal cavity. Anomalies of rotation and fixation of the intestine include the absence of rotation, its incompleteness, reverse rotation and improper attachment of the mesentery. The incidence of rotation anomalies is 1% and is 2 times more common in boys. As it returns to the abdominal cavity, the colon rotates counterclockwise.
The elongating intestine first rotates 90 degrees and continues to rotate up to 270 degrees. At the 10th week, the duodenum is fixed in the left upper quadrant of the abdomen.
At the same time, the colon completes its rotation. In this case, the cecum is located in the lower right quadrant. With various disorders, by the time the child is born, the duodenum, small intestine, and part of the large intestine may remain unrotated. Individual parts or the entire large intestine may remain unfixed, and the cecum may also be in an incorrect position. If an incomplete turn occurs, then the cecum appears in a different place (in the right hypochondrium or in the epigastrium). There are cases when a newborn’s stomach, duodenum and entire colon are located on the left, and the small intestine is on the right. In the area of the duodenum and cecum there are pathological adhesions and volvulus, in which the entire intestine is often involved.
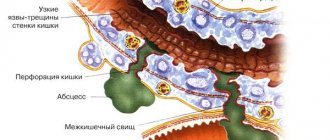
In the case of acquired strangulation intestinal obstruction in adults, there is a disturbance in the inflow of arterial blood and a deterioration in the venous outflow in the mesenteric vessels. When the passage of intestinal contents stops, the intestinal wall is damaged due to overstretching and the release of inflammatory mediators occurs. This leads to a significant increase in the permeability of the vascular wall and the progression of ischemia of the strangulated intestine.
With strangulation, blood flow disorders are more significant and develop very quickly. In the clinic, this manifests itself as profound disturbances in homeostasis . Due to the sweating of fluid, swelling of the intestinal wall develops, and the rapid leakage of blood into the intestinal lumen. An effusion quickly forms in the abdominal cavity - hemorrhagic during strangulation. The volume of fluid exuded during strangulation on the first day can be 5-6 liters. In the clinic, this is manifested by tissue dehydration, blood thickening, dry skin, decreased circulating blood and decreased urine output.
Dehydration of the body leads to an increase in the production of antidiuretic hormone and aldosterone , therefore, potassium is intensively released with vomit. Hypokalemia and intracellular acidosis develop . Developing electrolyte disturbances block the occurrence and propagation of the peristaltic wave - paresis of intestinal loops and their dilation occurs.
Overdistension of the intestine causes severe abdominal pain and reflex vomiting. As ionic disturbances and hypoxia of the intestinal wall increase, peristalsis fades, pain dulls - this is the phenomenon of “deathly silence”. In areas of intestinal ischemia, cell membranes are quickly destroyed, cells die and the level of toxic substances increases, the absorption of which into the bloodstream causes endogenous intoxication. The progression of endotoxemia causes the development of multiple organ failure. Increasing ischemia and intestinal damage cause perforation of the intestinal wall. With strangulation, perforation occurs within the first 6-7 hours from the moment of its occurrence.
Causes of volvulus
If we consider the causes in adults, then in most cases it is various acquired pathologies of the intestines or nearby organs. What causes intestinal volvulus? Let's name the main reasons:
- Constipation.
- Spikes.
- An increase in intra-abdominal pressure (this happens during physical stress), which leads to a sudden movement of intestinal loops.
- Increased peristalsis when taking large amounts of difficult-to-digest food (this often happens after fasting). This happens especially often in the sigmoid colon - with increased peristalsis, the intestine easily twists around its axis.
- Pregnancy . During pregnancy, sigmoid volvulus is the most common cause of intestinal obstruction. This is due to the fact that during pregnancy the uterus displaces the sigmoid colon, and this causes it to twist. In most cases, volvulus occurs in the third trimester.
- Abdominal adhesions.
- Volumetric formations.
- Surgery on the intestines.
As noted above, volvulus most often occurs in the sigmoid colon and it occurs with chronic constipation in bedridden (spinal) patients, with excessive use of laxatives, high fiber content, taking drugs that inhibit intestinal motility, ascites , ovarian tumors, pregnancy. Intestinal volvulus in adults, in particular the sigmoid colon, is typical for older people (over 60 years old) and there is an increase in incidence with age.
The causes of cecal volvulus are associated with congenital anomalies (significantly elongated mesentery), operations on this intestine, mass formations of the abdominal cavity and pelvis, and the formation of adhesions. If we talk about volvulus of the small intestine, the length of the intestinal loops can be different and total volvulus of the small intestine is possible. Symptoms of volvulus in adults will be discussed below.
Causes of volvulus in children
In childhood, volvulus of the large intestine is rare. Acquired bloat is also rare in children. At this age, volvulus of the small intestine, which is associated with:
- with congenital anomalies;
- adhesive processes;
- hernias (meaning internal hernias);
- diverticula.
Prevention
To prevent the disease from overpowering a person, the second person must follow a few simple rules. Basically, you need to beware of what causes volvulus:
- Do not overeat, especially before bedtime, when all body functions are weakened.
- Do not starve, and especially do not break after a long diet, so that there is no heavy load.
- Eat often, but in small portions.
- Increase physical activity - ensures normal intestinal motility.
- Conduct timely treatment of constipation and prevent it in time.
Volvulus is a dangerous disease, so it is extremely important to prevent its development. And if pathology appears, you must immediately contact a medical institution to receive qualified assistance.
Symptoms of volvulus
It is advisable to consider symptoms in different parts of the intestine, since they differ. The higher the level of obstruction , the more often attacks occur. The pain is more intense with strangulation obstruction than with obstructive obstruction. Vomiting with small intestinal obstruction is an early symptom and occurs immediately with an attack of pain.
Vomiting with colonic obstruction develops in the later stages. Retention of stool and gases primarily worries patients with low-grade colonic obstruction. Retention of stool and gases is more typical for colonic obstruction and manifests itself early. In case of small intestinal obstruction - later, since bowel movements continue.
Symptoms of volvulus in adults
If we consider volvulus of the small intestine, then only turning it by 1800 causes blocking of its lumen and compression of the vessels. If a small intestinal volvulus occurs, symptoms in adults develop suddenly and have characteristic signs of high strangulation obstruction - severe pain, vomiting, stool retention. Characterized by cramping pain in the abdomen, aggravated by peristaltic movements. It has different localization: in the umbilical region, epigastric in the right half of the abdomen or in the lower abdomen. The pain is so severe that patients scream in pain, become restless and take a position with their legs brought to their stomach.
Immediately after the pain, vomiting of eaten food develops. Vomiting becomes profuse, and vomit includes stagnant intestinal contents. In later stages, vomiting is fecal in nature. When there is volvulus of the small intestine, there is always retention of gases and stool. In the first hours of the disease, defecation is still present (the remaining contents of the final intestine). The condition of the patients is serious and progressively worsening.
On palpation, the abdomen is painless and is not swollen at first. In thin patients, a conglomerate of intestinal loops can be palpated. The tongue is dry and coated. Percussion of the abdominal cavity can reveal effusion. Peristalsis gradually weakens over time and a “splashing noise” appears. With incomplete inversions, bloating is noted and peristalsis is visible.
Sigmoid volvulus in adults most often develops slowly, and acute onset is extremely rare. Usually these are elderly patients who have had constipation and bloating for a long time with no expressed pain. Due to the slow progression, the patient’s condition remains satisfactory, and no signs of intoxication are observed.
Patients usually combat constipation with osmotic laxatives and enemas. In case of torsion, the pain intensifies and becomes cramping. Their intensity is different. The leading symptom of this pathology is stool and gas retention. The abdomen is distended, asymmetrical due to the protrusion of the displaced sigmoid colon upward and to the right (o). Due to severe swelling of the colon, the diaphragm and internal organs are pushed upward, and this makes breathing and cardiac activity difficult. Vomiting is rare and there is no stool.
Thus, typical signs of sigmoid colon volvulus are asymmetry of the abdomen with protrusion of the intestinal loop and the Tsege-Manteuffel symptom - a small capacity of the lower intestine (no more than 500 ml of water) when giving an enema. When examining through the rectum, dilation of the rectal ampulla and gaping of the anus are revealed. If the symptoms increase quickly, the patient’s condition worsens, there is a sharp pain in the abdomen, it is asymmetrical and tense. The pain is localized in the lower abdomen and sacrum, accompanied by single vomiting. Vomiting mixed with feces occurs only when paralytic obstruction and peritonitis . Intoxication quickly increases, and hemorrhagic effusion .
Cecal volvulus can occur in several ways and the clinical manifestations will differ. First of all, volvulus of the cecum together with the ileum is possible when they rotate around their common mesentery. In this case, a picture of strangulation intestinal obstruction arises, which is characterized by impaired blood supply to the intestine with the development of necrosis. This is the most dangerous form. With strangulation obstruction, the most intense pain is observed.
In the second version of volvulus (around the longitudinal axis of the cecum), obstructive obstruction without compromising the blood supply. The pain is less intense, constant and increases over time. Depending on this, patients either immediately seek medical help (in the first case), or with a delay of up to 7-10 days.
Initially, pain and vomiting appear, most patients have no bowel movements, and gases do not pass away. The pain (either constant or cramping) is localized near the navel and in the right half of the abdomen. An oval-shaped swelling is detected in the upper left quadrant of the abdomen. When listening to the right iliac region, increased peristalsis is heard.
Symptoms of volvulus in children
When volvulus occurs, intestinal obstruction occurs (cessation or disruption of the passage of contents through the intestines), which determines the symptoms of the pathology. In children, volvulus of the large intestine (in particular, the sigmoid colon) is less common than in adults. The main signs are: sudden onset of abdominal pain due to delayed bowel movements and intestinal bloating, which is determined by X-ray examination. Symptoms of colonic obstruction are less pronounced than those of small intestinal obstruction. The child’s anxiety is not pronounced and short-lived, and the general condition does not suffer much. During examination, it is sometimes possible to palpate the swollen intestine, which is located in the left iliac region or in the left hypochondrium.
Symptoms in infants with small intestinal volvulus differ. The child is characterized by severe anxiety, screaming, and restless legs. The child refuses the breast. During an attack, he becomes pale and covered in sweat. The duration of the attack is about 3-5 minutes. After the attack, the child calms down, but after a few minutes the attack of pain repeats. Moreover, each time the “light” interval between attacks is reduced - the pain practically becomes constant and loses its severity, but the baby’s general condition worsens.
Vomiting in the initial stage is associated with the viscerovisceral reflex, and then is a manifestation of intestinal obstruction . At the beginning of the disease, a child may have independent stool, but then stop. The condition progressively worsens, vomiting recurs.
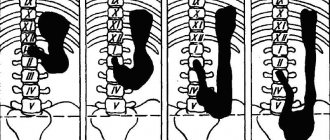
Tests and diagnostics
- Survey radiography . On an x-ray, sigmoid colon volvulus is defined as a sharply enlarged sigmoid colon, the size of which reaches the diaphragm. There are two levels of fluid in the intestine: at the proximal end and at the distal end. A cecal volvulus on a radiograph is visible in the form of a spherically swollen loop with pronounced bridges with a horizontal fluid level. The small intestine is distended, and the final sections of the large intestine are collapsed. In children with any localization of the pathology, a survey examination reveals general signs of obstruction (Kloiber cups and swelling of intestinal loops).
- Irrigography . Examination of the colon using a barium suspension that is injected into the colon. After it is filled, a series of pictures is taken. The sigmoid colon volvulus in the picture has the appearance of a “beak”, above which there is a greatly expanded loop of the sigmoid colon. By the orientation of the “beak” you can determine in which direction the twist occurred (clockwise or counterclockwise). During irrigography during cecal volvulus, barium passes up to ½ of the ascending colon, and above it is absent.
- Oral contrast is the administration of a barium suspension through the mouth followed by an x-ray examination. Used for suspected small bowel obstruction . The site of obstruction to the passage of contrast, enlarged loops of the small intestine and poor filling of the large intestine or its absence are identified.
- CT scan. The study is indicative of volvulus of the small and cecal intestines. With this pathology, the sign of a “storm sign”, expansion of parts of the intestine, thickening of its wall, and swelling of the mesentery are detected.
Procedures and operations
When a volvulus occurs in the small intestine, surgery is performed to straighten the volvulus. In the absence of peritonitis, the affected intestinal loops are excised and an anastomosis between the two ends of the intestine.
The main treatment method for cecal volvulus is also surgery. The intestine is straightened. In case of necrosis, hemicolectomy is performed with anastomosis. Shortening of the mesentery of the cecum is rarely performed recently, since recurrence of volvulus after this occurs with the same frequency as without shortening the mesentery. Weakened patients are offered percutaneous typhlostomy (a fistula in the cecum), but persistent fecal fistulas often occur after this procedure.
Sigmoid volvulus can be corrected by decompressing the loop using sigmoidoscopy . During this procedure, a tube is inserted into the intestine to prevent relapse. It is left in the intestine for 2-3 days, and a week later the operation is performed. Palliative intervention is performed if there are no changes in the intestinal wall. It includes straightening the volvulus and prophylactic shortening of the mesentery by gathering it into an assembly or fixing the sigmoid colon to the abdominal wall. Palliative interventions have a high rate of volvulus recurrence.
In case of necrosis of the intestine, a radical operation is indicated - its resection according to the general rules with an "end to end" or "end to side" anastomosis. If there is a complication in the form of intestinal gangrene, a resection of the non-viable area is performed, but an anastomosis between the ends of the intestine is not applied, but an unnatural anal opening (colostomy) is placed on the skin of the abdominal wall.
Removal of a sigmostoma is the safest option for surgery. During the second stage of the operation (after 3 months), the intestinal fistula is closed. Since it is very difficult to determine the viability of an intestinal loop in children, this tends to favor more active surgical tactics for volvulus of any part of the intestine.
Treatment
A patient is admitted with a questionable diagnosis to the gastroenterological or surgical department of a hospital. After confirmation of volvulus, he must be transferred to surgery. The disease can only be treated surgically.
Preparation for the operation consists of:
- in the decompression procedure - insertion of a probe through the nose, suction of stagnant contents and gases during volvulus of the small intestinal loops, if the pathology is located at the level of the sigmoid colon, sigmoidoscopy or colonoscopy is performed to insert a thin flexible tube and unload the intestines;
- massive intravenous infusion therapy to compensate for the loss of fluid, electrolytes, and relieve intoxication;
- alkalinization of blood with sodium bicarbonate solution;
- maintaining the level of protein and carbohydrates to provide the body with energy and plastic material.
Antibiotics are prescribed to prevent and treat peritonitis. The extent of surgical intervention depends on the patient's condition and the level of volvulus. In the absence of necrosis, the surgeon tries to straighten the twisted loops and secure them to the mesentery. The presence of necrosis requires removal (resection) of the damaged part of the intestine; in the small intestine, segmental resection is often performed with the creation of an anastomosis between the ends or from the small intestine to the large intestine.
A colostomy bag is connected to the intestinal stoma
If peritonitis is detected in the abdominal cavity, then initially you need to get rid of the inflammation of the peritoneum. Therefore, a stoma is placed on the skin of the abdomen, through which feces are discharged. The final reconstructive surgery is performed after 3 months. During this time, the patient’s condition stabilizes, and it is possible to create an interintestinal anastomosis.
Intravenous fluid administration continues to restore electrolyte balance. A significant threat is posed by infection (intestinal abscesses, fistulas, sepsis). Therefore, antibiotic therapy is prescribed.
Volvulus in children
The causes of volvulus at an early age are various anomalies of intestinal rotation and fixation. Malrotation of the intestine is an anomaly of its development, which consists in its inability to occupy a normal place in the abdominal cavity.
Malrotation most often refers to the small intestine and is not that common. In addition, excessive mobility of intestinal loops contributes to volvulus of both the small and large intestines. Anomalies of fixation are most common in young children. Most defects manifest themselves acutely at an early age and require urgent surgical intervention. The other part of the developmental defects has a chronic course and minimal symptoms (recurrent abdominal pain and vomiting).
The most common types of rotation and fixation disorders include hyperfixation of the duodenum and Ladd syndrome (anomaly of rotation of the small intestine and compression of the duodenum of the cecum). These pathologies arise at the second stage of embryonic development and manifest themselves in the first hours of a child’s life as complete or partial intestinal obstruction - regurgitation and vomiting appear in newborns.
Ladd's syndrome with volvulus of the small intestine and compression of the duodenum is manifested by intestinal obstruction. Symptoms of volvulus in an infant appear acutely - vomiting with bile, bloating, bleeding from the rectum, painful palpation of the abdomen, and there may also be an admixture of blood in the vomit. These symptoms in infants increase quickly, as intestinal ischemia worsens and sepsis . With incomplete compression of the duodenum in Ladd syndrome, a chronic course of obstruction is observed. It is manifested by impaired peristalsis, poor digestion of food, bloating, and impaired absorption.
With incomplete rotation syndrome, the early manifestations in infants are regurgitation and vomiting, which appears from the third day of life. Vomiting of stagnant discharge and bile, sometimes streaked with blood. Meconium and scanty transitional stool are released for the first 3-4 days, and then stop. hyperbilirubinemia may occur . This symptom is not typical for distal intestinal obstruction. With the development of complications ( intestinal necrosis ), asymmetry of the abdomen quickly increases, the child develops lethargy, activity and reflexes decrease, and the venous network on the anterior abdominal wall expands.
Symptoms of volvulus in older children are similar:
- stool disorders;
- colic and abdominal pain;
- gas formation;
- temperature increase;
- vomiting blood;
- bloody stools;
- intoxication.
If there is incomplete obstruction of the intestine (partial volvulus or moderate compression of the duodenum), the passage of contents through the intestine is restored, and then a relapse of obstruction occurs again: periodic abdominal pain, vomiting after eating. This chronic form of the course can be observed in older children over a number of years or appear for the first time at this age.
In this case, there is a lag in development, which is associated with impaired digestion and absorption. It has been noted that anomalies of intestinal rotation and fixation, which occur at stage III of embryonic development, have just such inconsistent symptoms and occur at an older age.
Diagnosis of complete obstruction in a newborn in the presence of clinical manifestations consists of performing an X-ray of the abdominal cavity. The diagnosis is confirmed by the absence of filling of the intestines with gas. Malrotation and volvulus are established by the corkscrew-shaped deformation of the duodenum, its vertical position and the location of the entire small intestine on the right, and the colon during irrigography is located on the left.
Treatment of bloat begins with conservative measures:
- Aspiration of gastric contents.
- Anesthesia.
- Intestinal bloating, if there is no disruption of intestinal trophism. Volvulus of the sigmoid colon can be untangled with a colonoscope, and after the release of stool and gases, the intestine returns to its normal position.
- Intensive therapy to maintain homeostasis in the child.
If the intestine does not straighten out, surgery is inevitable. Incomplete intestinal rotation in the presence of a pronounced clinical condition is subject to surgical treatment in the first hours of the child’s life. Children with partial recurrent obstruction also need to be operated on after the diagnosis has been clarified. The main methods of surgical treatment include:
- unwinding of the torsion;
- excision of fixing adhesions and cords;
- stabilization of the mesentery;
- fixation of the cecum in the correct position and in its natural place.
Diet
Diet 0 table
- Efficacy: therapeutic effect after 21 days
- Terms: 3-5 months
- Cost of products: 1200-1300 rubles. in Week
Diet Table No. 1
- Efficacy: therapeutic effect after 3 weeks
- Terms: 2 months or more
- Cost of products: 1500 - 1600 rubles. in Week
Diet Table No. 4
- Efficacy: therapeutic effect after 7-10 days
- Time frame: 21 days
- Cost of products: 1120-1150 rubles. in Week
Diet for partial intestinal obstruction should not contain large meals and overeating - this provokes an exacerbation. Avoid foods that increase gas formation (cabbage, soy products, legumes, whole milk, yeast baked goods). Patients are recommended to eat frequent, small meals. Sooner or later, the patient has to resort to surgical treatment, after which special nutrition is organized.
After the operation, food intake is possible after a few days, and for the first time tube feeding with special nutritional mixtures is organized. After a while, the patient switches to a zero diet - this is a diet designed for patients who have undergone operations on the digestive organs.
This is the most gentle nutrition in the form of sequentially assigned Tables - No. 0A , No. 0B , No. 0B . The basis of these tables is liquid, jelly-like and pureed food, which is consumed in small portions (no more than 200 g per meal) and often. Diets include easily digestible proteins, fats and carbohydrates, the amount of which gradually increases. All are characterized by a decrease in the amount of salt and an increase in fluid intake.
For the first 2-3 days of normal nutrition, the patient can eat mild and low-fat meat broth, liquid jelly, rice water with cream, compote without fruit, rosehip infusion, tea with sugar, fruit jelly, diluted freshly prepared juices. On the third day, add a soft-boiled egg and 50 ml of cream. Over the next 2-4 days, pureed porridge (rice, buckwheat, oatmeal) is introduced. They are boiled in water or broth. The serving volume increases to 350 g. By the end of the first week, puree soups, pureed boiled meat or fish, pureed cottage cheese diluted with cream to the consistency of sour cream, fermented milk drinks, fruit and vegetable purees, baked apples, and, if well tolerated, pureed milk porridges are introduced.
Thus, zero diets gradually load and train the gastrointestinal tract, serving as a transition to nutrition within Table No. 1 . They exclude whole milk (it is present only in dishes), all dishes with a dense consistency and carbonated drinks. Over time, food expands within Table No. 4 .
Nutrition
In the future, products that enhance intestinal perilstatics are excluded or limited from the patient’s menu:
- bran;
- coarse porridge with peel;
- dairy products;
- cold drinks;
- vegetables and fruits with peels, especially raw;
- legumes;
- apricots, prunes;
- nuts;
- all types of greens;
- vegetable oil.
They also exclude some foods that have a negative effect on the entire digestive tract:
- roast;
- canned food;
- spicy;
- smoked;
- fat;
- alcohol;
- soda.
Consequences and complications
Complete intestinal volvulus causes:
- closed intestinal obstruction (intestinal obstruction);
- impaired blood supply to the intestinal wall;
- gangrene;
- perforation of the intestinal wall;
- development of peritonitis ;
- sepsis.
In case of incomplete obstruction:
- there is a risk of developing mesenteric cysts and chylous ascites ;
- the occurrence of intestinal adhesions.
List of sources
- Doroshevsky Yu.V. Surgical treatment of newborns with rotation defects and rotation of the midgut. — Bulletin of Surgery. - 1978. - No. 2. - P. 92–97.
- Volvulus of the sigmoid colon. Errors in the diagnosis and treatment of acute diseases and injuries of the abdomen / Medicines and medicine: a medical reference book.
- Ioskevich, N. N. Practical guide to clinical surgery: Diseases of the digestive tract, abdominal wall and peritoneum / N. N. Ioskevich; edited by P. V. Garelika. Minsk: Vysh. school, 2001. 685 p.
- Smirnov A.N. with co-authors. Incomplete intestinal rotation in older children (clinic, diagnosis, treatment). — V. book: 4th Russian Congress “Modern technologies in pediatrics and pediatric surgery” (congress materials). - M., 2005. - P. 372.
- Totikov V.Z., Medoev V.V. Some issues of surgical treatment of sigmoid colon volvulus. // Vladikavkaz Medical and Biological Bulletin. Vladikavkaz. 2007. Volume 7. Issue 13. p. 320-323.
Doctors' recommendations
Volvulus in humans is a very unpleasant illness that causes a lot of inconvenience and pain. In acute conditions associated with this organ, you should call an ambulance, especially when it comes to children. After the initial examination, the paramedic will decide whether to transport the patient either to an infectious disease specialist or to an appointment with a surgeon.
If the intestinal disease is chronic, observation by a gastroenterologist is required - a doctor who is responsible for diseases of the digestive tract. If the rectum is affected, you should contact a proctologist.