Mirena is an intrauterine device, which is an entire hormonal system used in gynecology not only for contraceptive, but also for therapeutic purposes. Mirena for adenomyosis helps relieve concomitant symptoms, alleviate the patient’s condition, and stop the progression of pathological processes associated with uncontrolled growth of the endometrium.
Installation of the spiral is carried out only according to medical indications, because it has its own contraindications and side effects. The validity period of the drug is up to 5 years. After this period, the spiral is removed and, if necessary, a new one is installed. Before prescribing the Mirena coil to a patient, medical specialists will conduct a comprehensive diagnostic examination, which will help eliminate contraindications and avoid side effects.
In what cases is Mirena prescribed for adenomyosis?
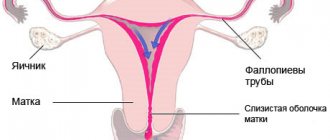
Adenomyosis is a gynecological pathology in which the endometrium grows into the muscular layer of the uterus. The progression of the disease is accompanied by pathological symptoms, disruption of the reproductive system, and the inability to conceive and bear a child. Mirena for uterine adenomyosis helps stop the uncontrolled growth of the endometrium and relieve unpleasant symptoms.
The intrauterine device is installed only according to doctor's indications. The drug is recommended in the following cases:
Progressive internal adenomyosis, manifested by a pronounced clinical picture. A woman is worried about severe pain in the lower abdomen, heavy, prolonged menstrual bleeding, and discomfort during sexual intercourse.
- Uterine leimioma.
- Endometrial hyperplasia.
- Menstrual irregularities.
- Extensive damage by foci of adenomyosis of the myometrium.
- Heavy uterine bleeding, contributing to the development of iron deficiency anemia.
An intrauterine device is installed in women who have already given birth to a child. In exceptional situations, the drug is also used for nulliparous women, but in this case there is a high risk of prolapse of the system from the uterus. Before installation, the doctor sanitizes the vagina and cervix to make sure there are no active inflammatory processes. It is worth noting that after implantation, a woman will not be able to get pregnant for 5 years; this fact is also taken into account by the doctor before prescribing the drug.
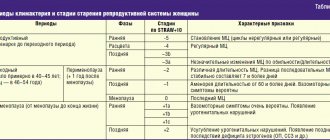
Brief overview of the topic
The Mirena IUD is a small device that helps prevent pregnancy. The appearance of the intrauterine therapeutic system (see photo) resembles the letter “T” placed in a special conductor tube, which has a white core and has an elastomeric hormonal filling. The body of the spiral is equipped with a loop on one side and two arms on the other. Attached to the loop are threads that are used to remove the IUD from the vagina. A trained gynecologist inserts the device into the uterus, after which it can remain there for up to six years.
IUDs like Mirena also help treat “heavy” periods. Mirena begins to work as soon as it is inserted. After a few months, your periods will become shorter in duration and less painful.
Women who are not sexually active but have heavy or painful periods and certain other indications may choose Mirena as an alternative to birth control pills.
Mirena photo
Reviews from doctors about Mirena are unanimous - this device is one of the best options both for preventing unplanned pregnancy and for correcting abnormalities in the menstrual cycle and treating certain pathologies of the uterus.
Pros of Mirena
- It's effective - Mirena is more than 99% effective in preventing pregnancy.
- Ideal for nursing mothers.
- It's convenient - instead of taking birth control pills every day, you don't need to worry about anything - Mirena will do everything for you!
- It helps reduce pain and the amount of blood lost during menstruation.
- The hormonal IUD has fewer side effects than birth control pills. Reviews from women who take oral pills indicate the occasional occurrence of side effects such as weight gain and nausea. Mirena does not contain estrogen (it delivers only progestin to your uterus) and therefore does not have the side effects that the pill can cause.
- This is reversible - if you have a Mirena installed and are thinking about conceiving a child, your IUD can be removed at any time you wish.
IUD Mirena provides reliable contraceptive effect, which experts compare to surgical sterilization. When using the drug, there is a low content of progestogens in the bloodstream. Its obvious advantage, among other things, is the absence of the effect of primary passage through the gastrointestinal tract and the liver, which leads to a better, predominantly direct effect with minimal hormonal load on the body.
Experts also note a certain therapeutic effect of the hormonal intrauterine device "MIRENA" if a woman has idiopathic menorrhagia, uterine fibroids, dysmenorrhea, endometrial hyperplasia, PMS.
Cons of Mirena
- Perforation during insertion;
- Low risk of pelvic inflammatory diseases;
- Possible infection after administration;
- There is a slight risk of the Mirena IUD becoming dislodged during use;
- Intermenstrual bleeding or irregular spotting. It is almost impossible to predict the appearance of these discharges or get rid of them; they usually go away on their own 6-12 months after the introduction of Mirena;
- Drawing pain in the lower abdomen and pelvis;
- Spontaneous expulsion in the first year of wearing the IUD.
Contraindications
- You are pregnant or do not exclude this possibility;
- There are untreated pelvic inflammations;
- Reproductive tract infections detected;
- There is unexplained vaginal bleeding;
- Suspicion of cervical or uterine cancer;
- There is liver disease or tumor;
- Mammary cancer;
- Pathologies of the uterine cavity;
- Allergy to components of Mirena, such as levonorgestrel, silicone, polyethylene, silicon dioxide, barium sulfate or iron oxide.
Installation of Mirena
The active substance is levonorgestrel and this determines the indications for installing Mirena in women 30-40-50 years old. This hormone is metabolized more slowly (compared to progesterone) in the endometrium, due to which it has a more pronounced effect on the inner lining of the uterus. Namely, it helps to slow down the growth of the mucous membrane, suppressing the division of myometrial and endometrial cells. As a result of using Mirena, periods “disappear”. Moreover, this is not caused by inhibition of ovarian function, but by the reaction of the endometrium to the local effect of levonorgestrel. The positive effects of the hormonal system can only be realized if Mirena is administered correctly!
Before starting to use the Mirena IUD, you must undergo a preliminary examination according to the standards provided for the selection of contraceptives containing hormonal components.
According to the instructions, Mirena is installed:
- For women of childbearing age, the intrauterine system is recommended to be inserted into the uterine cavity on days 1-7 of the menstrual cycle;
- after an induced abortion in the first trimester of pregnancy - immediately after the next menstruation;
- after an uncomplicated spontaneous miscarriage - no earlier than 6 weeks;
- when carrying out estrogen replacement therapy, Mirena after 40-50 years can be administered in the last days of menstruation or breakthrough bleeding;
- In women with amenorrhea, a hormonal IUD is placed at any time.
Indications for installation:
- contraception; - idiopathic menorrhagia; — endometrial hyperplasia (treatment and prevention); - endometriosis and some fibroids.
Mirena for endometriosis
Endometriosis is a pathological condition where cells from the inner layer of the uterus, the endometrium, grow outside of it. This gynecological disease is characteristic of women of reproductive age and, in addition to pain and dysfunction of neighboring organs, can lead to infertility.
The Mirena intrauterine device, according to gynecologists, is an effective remedy for eliminating endometriosis in women after 40 years of age for several reasons: • the effect of the drug, confirmed by clinical studies, is manifested by suppression of the growth of pathological lesions, a decrease in their size and gradual resorption; • fewer side effects than other hormonal drugs; • relief of pain, inherently associated with the problem of endometriosis; • there is no need to take daily pills or give injections; • gradual normalization of the menstrual cycle; • there is no need for special contraception.
Endometrial hyperplasia and Mirena
Hyperplasia is a pathological condition and is an excessive growth and thickening of the uterine mucosa. Its signs include heavy and prolonged bleeding during menstruation or uterine bleeding not related to the cycle, lack of ovulation and the inability to implant an embryo into the altered endometrium, which is a consequence of the increased level of estrogen in the body. Gynecologists-endocrinologists recommend using the Mirena intrauterine system for hyperplastic processes due to the reliability of its pharmacological effect on the endometrium. Another advantage is the convenience of daily dosing of the hormone, which does not require additional medical knowledge on the part of the woman and is relatively inexpensive compared to other therapeutic agents.
Mirena - original or fake
Patients who want to buy and install this IUD cheaply often wonder how to avoid running into low-quality, counterfeit goods. It seems that I would like the price to be lower, to be installed cheaper, and for the IUD to be branded, from the manufacturer.
The desire is understandable, but unfortunately, impossible. Of course, if you set the task this way - buy the original Mirena and not give money for a fake. The product is official and certified for use in the Russian Federation and has a number of features, knowing which you can rest assured about your purchase. So how can you tell the difference between an original Mirena and a fake?
A real hormonal IUD has the following characteristics:
- The inscriptions on the box are in Russian
- Instructions for use of the product in Russian
- Sealed packaging with the device itself with explanations in Cyrillic
- Date of manufacture/expiration date indicated
- Prices for Mirena in a pharmacy start from 14,000 rubles, rarely - a little cheaper.
- If the cost of the Mirena spiral you find is lower than these figures, for example, it is offered for sale for 8,000 - 10,000 rubles, you can be sure that this product is not original, i.e. provided for sale on the territory of the Russian Federation, and is sold illegally. What to do in this case - be tempted by low prices and take a risk, or make a choice in favor of reliability and quality - it’s up to you to decide! In our clinic you will receive a certified product from an official supplier.
Photo of what a real, original Mirena should look like for use on the territory of the Russian Federation (picture on the left or, on mobile devices, on top). The differences and differences with the second one are visible to the naked eye.
After Mirena
Common side effects after Mirena installation (in the coming hours) include:
- Pale skin
- Bleeding
- Sweating
- Spasms
- Fast heartbeat
- Dizziness and fainting
If you experience more serious adverse reactions or symptoms that last longer than 30 minutes, you should contact your doctor or any healthcare professional immediately.
Long-term (months after administration) complications from Mirena can be as follows:
- Acne
- Hair loss
- Headache
- Nausea
- Blistering
- Unwanted hair growth
- Decreased sex drive
- Breast tenderness
- Cramps or pain during menstruation
- Nervousness
The main disadvantages that some women complain about after the introduction of the Mirena spiral in their reviews are nausea, dizziness, hormonal changes, cramps in the lower abdomen and some other mild side effects. As a rule, these symptoms practically disappear within the first 3-4 months. The disadvantages of Mirena, if they are unobtrusive and short-lived, cannot serve as an indication for removing the device.
Side effects from its use are not felt by all women. Some simply do not notice the spiral and in their reviews consider Mirena an excellent contraceptive.
Removing Mirena
Mirena should be removed 5 years after its installation. If a woman wishes to use this remedy in the future, then in the absence of contraindications and satisfactory results of the control examination, a new intrauterine system can be introduced.
Mirena should not be used during pregnancy. If a woman conceives while using the product, it is recommended to remove the IUD, since the contraceptive, remaining in place, increases the risk of miscarriage and premature birth. Removing the Mirena or palpating the uterus during a pelvic examination can also cause a miscarriage.
If it is impossible to carefully remove Mirena, you need to consider the advisability of abortion. If a woman wants to continue her pregnancy, she must be informed of the risks and understand the possible consequences.
The principle of operation of the hormonal intrauterine system
The Mirena therapeutic spiral contains the hormone levonorgestrel from the progesterone group. The hormone is enclosed in a special housing and protected by a membrane that regulates its release. Progestogen is released directly into the uterine cavity, affecting the functioning of the reproductive system.
The principle of operation of the hormonal intrauterine system:
- Reduces the sensitivity of receptors to specific hormones such as estrogen and progesterone.
- Makes the uterine mucosa immune to the female sex hormone estradiol.
- Prevents the growth of new pathological tissues.
Thanks to these medicinal properties, the coil for uterine adenomyosis helps to significantly improve the patient’s condition:
- Normalize the amount of menstrual flow, making it moderate.
- Eliminate pain and discomfort.
- Reduce the risk of uterine bleeding.
- Eliminate secondary anemia caused by excessive blood loss
Pharmacokinetics
Absorption.
After administration of the drug Mirena®, levonorgestrel begins to be immediately released into the uterine cavity, as evidenced by measurements of its concentration in the blood plasma. The high local exposure of the drug in the uterine cavity, necessary for the local effect of Mirena® on the endometrium, provides a high concentration gradient in the direction from the endometrium to the myometrium (the concentration of levonorgestrel in the endometrium exceeds its concentration in the myometrium by more than 100 times) and low concentrations of levonorgestrel in plasma blood (the concentration of levonorgestrel in the endometrium exceeds its concentration in the blood plasma by more than 1000 times).
Rate of release of levonorgestrel into the uterine cavity in vivo
initially is approximately 20 mcg/day, and after 5 years it decreases to 10 mcg/day.
Distribution.
Levonorgestrel binds nonspecifically to plasma albumin and specifically to SHBG. About 1–2% of circulating levonorgestrel is present as the free steroid, whereas 42–62% is specifically bound to SHBG. During use of the drug Mirena®, the concentration of SHBG decreases. Accordingly, the fraction associated with SHBG during the period of use of Mirena® decreases, and the free fraction increases. The average apparent Vd of levonorgestrel is about 106 L.
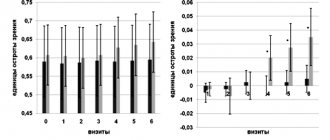
After administration of Mirena®, levonorgestrel is detected in the blood plasma an hour later. Cmax is achieved 2 weeks after administration of Mirena®. Consistent with the decreasing release rate, the median plasma concentration of levonorgestrel in women of reproductive age weighing more than 55 kg decreases from 206 pg/ml (25–75th percentile: 151–264 pg/ml) determined at 6 months to 194 pg/ml (146-266 pg/ml) - after 12 months and up to 131 pg/ml (113-161 pg/ml) - after 60 months.
Body weight and plasma SHBG concentrations have been shown to influence systemic levonorgestrel concentrations, i.e. with low body weight and/or high SHBG concentrations, levonorgestrel concentrations are higher. In women of reproductive age with low body weight (37–55 kg), the median plasma concentration of levonorgestrel is approximately 1.5 times higher.
In postmenopausal women using Mirena® simultaneously with the use of estrogens intravaginally or transdermally, the median concentration of levonorgestrel in the blood plasma decreases from 257 pg/ml (25–75th percentile: 186–326 pg/ml), determined after 12 months, up to 149 pg/ml (122–180 pg/ml) - after 60 months. When using Mirena® simultaneously with oral administration of estrogens, the concentration of levonorgestrel in the blood plasma, determined after 12 months, increases to approximately 478 pg/ml (25–75th percentile: 341–655 pg/ml), which is due to the induction of SHBG synthesis.
Biotransformation.
Levonorgestrel is extensively metabolized.
The main metabolites in blood plasma are unconjugated and conjugated forms of 3α, 5β-tetrahydrolevonorgestrel. Based on the results of in vitro
and
in vivo studies,
the main isoenzyme involved in the metabolism of levonorgestrel is CYP3A4. The isoenzymes CYP2E1, CYP2C19 and CYP2C9 may also be involved in the metabolism of levonorgestrel, but to a lesser extent.
Elimination.
The total plasma clearance of levonorgestrel is approximately 1 ml/min/kg. Unchanged levonorgestrel is excreted only in trace amounts. Metabolites are excreted through the intestines and kidneys with an excretion coefficient of approximately 1.77. T1/2 in the terminal phase, represented mainly by metabolites, is about a day.
Linearity/nonlinearity.
The pharmacokinetics of levonorgestrel depends on the concentration of SHBG, which, in turn, is influenced by estrogens and androgens. When using the drug Mirena®, a decrease in the average concentration of SHBG by approximately 30% was observed, which was accompanied by a decrease in the concentration of levonorgestrel in the blood plasma. This indicates the nonlinearity of levonorgestrel pharmacokinetics over time. Given the predominantly local effect of Mirena®, the effect of changes in systemic concentrations of levonorgestrel on the effectiveness of Mirena® is unlikely.
Benefits of using Mirena
During the conservative treatment of adenomyosis, various hormonal drugs are used, but Mirena has its own advantages:
- Installation is carried out once every 5 years. Unlike hormonal pills, which must be taken strictly according to schedule, after inserting an intrauterine device, a woman does not need to follow any rules or treatment regimens. The IUD remains effective throughout its stay in the body.
- Allows you to achieve a therapeutic effect with a minimal dosage of the hormone. The hormone levonorgestrel, which is part of the drug, enters directly into the uterine cavity, exerting a localized effect.
- Minimal risk of side effects. The drug does not pass through the digestive system, so it does not affect other internal organs.
- No risk of overdose. During the day, a strictly fixed dose of levonorgestrel is released - 20 mcg.
- Reliable contraception. After implantation of an intrauterine device, a woman is reliably protected from unwanted pregnancy.
- Normalization of hormonal levels.
Patients are often prescribed the drug Visanne for uterine adenomyosis. The active ingredient of the product is micronized dienogest - a synthetic hybrid gestagen of the third generation. The drug is available in tablet form and is used for internal and external endometriosis. The doctor must decide which is better - Visanne or Mirena for adenomyosis, taking into account the nature of the disease, the degree of neglect, the presence of indications and contraindications.
What is
The mechanism of action of the hormonal IUD is identical to other types of contraceptives. The drugs included in its composition kill sperm that have penetrated the uterine cavity, and also prevent the attachment of a fertilized egg to the walls of the uterus. The spiral may differ in its shape, material and composition. It is better to entrust the choice of a particular contraceptive to an experienced specialist.
On a note! It is worth noting that this type of intrauterine contraception does not protect a woman from sexually transmitted infections.
Disadvantages of the IUD
Like any other medication, the Mirena therapeutic system has its drawbacks, among which the most significant are:
- Installation and removal is carried out only by a doctor.
- Not suitable for women who are planning pregnancy in the near future.
- Has an abortifacient effect. The IUD does not always suppress ovulation, so conceiving a child is possible. But the pregnancy is terminated not yet in the early stages, since the implantation process is disrupted and a miscarriage occurs.
- Long adaptation period. In the first 3 to 6 months after IUD implantation, you may experience intermenstrual bleeding, which is normal.
- When installing an IUD, the risk of infection entering the uterine body increases.
- It is rare, but it happens that the drug leads to the progression of an aseptic inflammatory process in the reproductive organ.
Features of use during pregnancy and lactation
Any means of contraception cannot be used while carrying a child. If pregnancy occurs while using the Mirena system (this can happen if the IUD is installed incorrectly or falls out), then it must be taken out, as the likelihood of an unplanned abortion or premature birth increases. If the system is removed incorrectly, spontaneous abortion can also occur.
You can use this method of contraception only 1.5 months after the birth of the child. The IUD will not affect the quantity and quality of breast milk in any way.
Scheme for using a hormonal IUD
Before inserting an intrauterine device, simple preparation is required, including the following steps:
- Initial examination by a doctor. During the procedure, the gynecologist assesses the general condition of the patient’s genital tract and excludes contraindications for the use of the drug.
- Testing for sexually transmitted infections. Laboratory procedures such as bacterial culture and survey smear will help identify possible problems. If necessary, tests for viral and intracellular infection are prescribed - PCR, ELISA.
- Ultrasound of the pelvic organs. Ultrasound examination helps to assess the condition of the uterus and appendages, diagnose concomitant pathologies, and determine the degree of progression of adenomyosis.
If there are no contraindications to the insertion of an intrauterine device, the doctor will agree on the date and time of the procedure. The Mirena hormonal system is installed on the 3rd – 7th day of the cycle - at the end of menstruation. During this period, the cervix is dilated, which allows the IUD to be inserted inside without hindrance.
The technology for maintaining the Mirena therapeutic system includes the following stages:
- Control examination and treatment of the genital mucosa with an antiseptic solution.
- Introduction of the mirror.
- Grasp the upper lip of the cervix with special gynecological forceps.
- Checking the patency of the cervical canal and the depth of the uterine cavity with a probe.
- Insertion of a guidewire and an intrauterine device through it.
- Removing the conductor.
After the guide is removed, the IUD remains in the uterus. All manipulations are carried out under ultrasound control, which significantly reduces the risk of side effects. After 5 years the sprial will need to be removed. Premature removal of the system is carried out in the following situations:
- development of unwanted side effects;
- complications arising from the installed IUD;
- pregnancy planning.
Removing the spiral
The removal of hormonal contraceptives is also carried out by a doctor. The device can be removed on any day of your period (provided you have a regular menstrual cycle). To do this, special pliers are used that grab its threads and carefully remove it. If the device was removed due to its expiration date, a new intrauterine contraceptive device can be installed on the same day.
If the IUD is removed outside of menstruation, then 7 days before this procedure you must start using other barrier methods of contraception.
When the Mirena IUD is removed, your doctor should check its integrity to ensure that all components have been successfully removed.
After the IUD is removed, the ability to become pregnant is restored almost immediately. Only in rare cases may this take time (up to six months).
Side effects and contraindications
After installation of the Mirena therapeutic system, side effects rarely develop, but they are still possible. Among the most common complications are the following:
- Individual intolerance to the drug, accompanied by pathological reactions and deterioration in general well-being.
- Frequent headaches, nausea, depressed mood, decreased libido.
- Periodic abdominal pain, bloating.
- Sudden jumps in blood pressure.
- Infections of organs located in the abdominal cavity.
- Failure of the menstrual cycle, manifested by a prolonged absence of menstruation.
Against the background of an implanted intrauterine device, the condition of the skin may worsen. Blackheads, acne, and inflammation appear on the face and body. In extremely rare cases, after the installation of an IUD, cysts form in the myometrium.
The Mirena therapeutic system is not prescribed to patients with suspected pregnancy. In this case, the woman must undergo tests to make sure there is no conception. Also, the IUD is contraindicated for implantation if the following pathologies are diagnosed:
- neoplasms of a malignant nature;
- uterine fibroids larger than 5 cm;
- inflammatory processes in the organs of the genitourinary system;
- congenital or acquired immunodeficiency;
- uterine bleeding of unknown etiology;
- individual intolerance to the active component of the drug.
Who is the IUD not suitable for?
This is a very convenient method of contraception, suitable for almost everyone: women over 40 and young girls. If previously it was believed that the IUD could be placed only after childbirth, today gynecologists recommend it for nulliparous women. Use is also possible after a cesarean section, but only 3 months after the operation.
Due to the constant presence of a foreign body inside the uterus, the cervix is always slightly open, which means it is more accessible to pathogens. In this regard, the use of the spiral is contraindicated in case of inflammation or infectious diseases, including chronic ones.
Gynecologists do not recommend uterine contraception for women with acute and cancerous pathologies of the genitourinary system, as well as with severe heart and vascular defects.
Other contraindications include:
- previous ectopic pregnancy;
- cervical dysplasia;
- anemia and pathologies of hemostasis;
- diseases of the endocrine system, including diabetes;
- deviations in the structure of the uterus.
Complications associated with IUD insertion
During installation of an intrauterine device, there is a risk of developing the following complications:
- Perforation of the uterus. Injury leads to heavy bleeding and a sharp deterioration of the condition. Perforation mainly occurs due to deformation of the reproductive organ or congenital developmental anomalies.
- Expulsion of the system. If the coil falls out, you need to consult a doctor who will replace the drug.
- Endometritis. The main cause is an untreated genital tract infection.
- Ectopic pregnancy.
- Follicular atresia. After implantation of the IUD, the hormonal background changes, so the maturation of the egg is possible, but the follicle does not always mature completely. It increases in size and becomes similar to an ovarian cyst. Often, such a follicle resolves on its own within 2.5 – 3 months. If this does not happen, the patient's treatment plan changes.
Drug interactions
The metabolism of gestagens may be enhanced by the simultaneous use of substances that are enzyme inducers, especially cytochrome P450 isoenzymes involved in the metabolism of drugs, such as anticonvulsants (for example, phenobarbital, phenytoin, carbamazepine) and drugs for the treatment of infections (for example, rifampicin, rifabutin, nevirapine, efavirenz ). The effect of these drugs on the effectiveness of Mirena® is unknown, but it is believed that it is insignificant since Mirena® has mainly local effects.