Hemorrhoids are the most common vascular disease in proctology, in which the cavernous (cavernous) bodies in the terminal part of the rectum expand. Many people do not attach importance to its symptoms, thus leading the process to complications.
According to statistics, every 7 out of 10 people on our planet experience symptoms of hemorrhoids. Lack of timely adequate treatment can lead to serious complications. Among them are bleeding from hemorrhoids, their inflammation, thrombosis and necrosis, anemia, paraproctitis and anal fissure. MedicCity proctologists recommend undergoing regular examinations by a specialist to prevent unpleasant consequences of the disease. In the early stages, hemorrhoids are treated using the most gentle methods possible!
Hemorrhoids in women usually occur during pregnancy and childbirth. Hemorrhoids during pregnancy are quite difficult to treat, since most medications can adversely affect the development of the fetus. Therefore, women are recommended to visit a proctologist at the stage of pregnancy planning.
1 Consultation with a proctologist in MedicCity
2 Consultation with a proctologist in MedicCity
3 Consultation with a proctologist in MedicCity
Hemorrhoids in men are no less common. The disease appears as a result of a sedentary lifestyle, sedentary work (for example, hemorrhoids are an “occupational” disease of drivers), digestive disorders, constipation, alcohol abuse, and smoking. The cause of the disease can also be increased physical activity and hereditary predisposition.
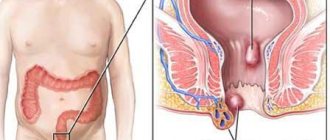
It is customary to distinguish the following types of hemorrhoids: external (external) hemorrhoids and internal hemorrhoids.
This video talks about the main causes of hemorrhoids. Hemorrhoids are a chronic disease that, without timely treatment, progresses and often leads to serious complications.
Brief classification
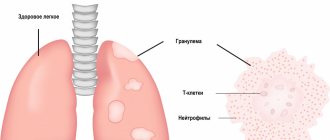
Hemorrhoids are a painful enlargement of the cavernous cavities of the venous plexus of the rectum.
These cavities fill with blood when straining, performing the function of a kind of “pillow” that protects tissues from the traumatic effects of solid feces during the act of defecation. Hemorrhoids are a pressing problem for humanity; about 60% of Earth's citizens experience at least one episode of painful enlargement of hemorrhoids throughout their lives. It must be said that this percentage is much higher in countries that are commonly called civilized.
Anatomically, internal hemorrhoids - hemorrhoidal nodes in the distal (terminal) part of the rectum, and external hemorrhoids , when the nodes are located outside in the anal area.
According to the nature of the course, hemorrhoids can be acute , associated with thrombosis of the hemorrhoidal veins, and chronic , caused by constant overflow of distended veins with blood.
External (external) hemorrhoids
The external manifestation of hemorrhoids is the presence of varicose veins (hemorrhoids), which are located outside the anus. External hemorrhoids appear near the anus.
Enlargement and inflammation of hemorrhoids occurs due to stagnation of blood in the pelvis and in particular in the cavernous bodies of the anal canal.
When a blood clot appears in the external hemorrhoid, swelling develops and the person begins to feel pain. The sufferer may feel hemorrhoids as a large, firm “bump” covered with thin, sensitive skin.
With poor nutrition, a sedentary lifestyle, heavy physical activity and stagnation of venous blood in the rectum, a complication in the form of acute thrombosis (the so-called “hemorrhoidal thrombosis”) may occur.
Blood in external (external) hemorrhoids (hemorrhoidal thrombosis) appears when the skin over the hemorrhoid becomes thinner and the blood clot breaks out in the form of a clot, then scarlet blood may appear.
1 Hemorrhoidectomy in MedicCity
2 Hemorrhoidectomy in MedicCity
3 Hemorrhoidectomy in MedicCity
Symptoms of external hemorrhoids
With this type of disease, the following symptoms of hemorrhoids can be distinguished:
- pineal-shaped protrusion around the anus;
- hemorrhoids, varying in size and location, which are easily palpable by the patient and increase with strain during bowel movements;
- pain and blood during bowel movements;
- unpleasant burning and itching in the anus;
- piercing pain at rest, after stool, when walking, coughing and sneezing (with the development of hemorrhoidal thrombosis);
- severe pain when touching hemorrhoids (hemorrhoids increase in size, swell, turn blue).
Reasons for the development of hemorrhoids in women
Chronic hemorrhoids in women, as a rule, develop after 30 years of age; with age, the risk of developing the disease increases. Women suffer from dilated hemorrhoidal veins four times less often than men. However, the risk increases in the presence of permissive factors: • chronic constipation; • prolonged sitting on the toilet; • obesity; • sedentary work, sedentary lifestyle; • diseases occurring with chronic cough; • diseases of the pelvic organs.
A typical cause of acute hemorrhoids in women is pregnancy or childbirth. In such cases, adequate conservative treatment leads to the disappearance of the problem. However, if therapy was untimely or careless, the disease becomes chronic.
Causes of hemorrhoids
The development of the disease is promoted by many reasons, including hereditary predisposition, excess weight, physical inactivity or bad habits. In addition, hemorrhoids often result from professional activities associated with prolonged exposure to one position (pilots, drivers, office workers, etc.). Various disturbances in the functioning of the intestines, caused by poor nutrition and abuse of spicy, fatty, fried foods, and fast food, are a provoking factor of the disease. In women, the disease most often progresses during pregnancy and childbirth, and in men, the development of the disease can be caused by a passion for strength training and lifting weights.
At the second stage of hemorrhoids, patients often seek medical help, because the disease brings significant discomfort and its symptoms can no longer be ignored.
Symptoms of the acute form of the disease
Symptoms of acute hemorrhoids in young women are most often associated with pregnancy or childbirth. The appearance of an enlarged hemorrhoid constipation characteristic of this period .
Acute dilatation of hemorrhoidal veins manifests itself with sharp pain , which becomes unbearable during bowel movements. In addition, the pain syndrome can intensify while walking, as well as with increased intra-abdominal pressure during straining, coughing, laughing, and hiccups.
Another characteristic sign of the acute form of the disease is bleeding from the dilated veins of the rectum. This symptom manifests itself as fresh blood on the surface of the stool.
Often hemorrhoids in women are combined with anal fissure. In such cases, blood stains on toilet paper and underwear appear even more often after defecation.
Stages of development of chronic pathology
With chronic hemorrhoids, the pain syndrome is much weaker. Often the only signs of chronic pathology are itching around the anus blood appearing on the surface of the stool from time to time .
The stages of development of internal hemorrhoids differ using the most objective symptom - the degree of stretching of the dilated veins: I. The hemorrhoid is constantly located in the intestinal cavity II. The knot falls out when straining and resets itself back III. The patient has to adjust the knot with his hands IV. One or more hemorrhoids are constantly on the outside and cannot be reduced
At any stage, thrombosis of the dilated veins of the rectum , in which case severe pain syndrome characteristic of an acute attack occurs.
With a long course of the disease, the risk of complications increases ( anemia, neurasthenia, anal fissure, etc. ).
Possible complications
Due to the fact that internal hemorrhoids are much more difficult to diagnose than external hemorrhoids, you can skip the period of possible effective treatment. The effectiveness of all procedures aimed at combating the disease depends on the period in which the patient sought help at the hospital. It is very important for both women and men to pay great attention to their health and undergo regular, complete examinations whenever possible. If, nevertheless, the onset of the disease is missed, then this can lead to such troubles as anemia, strangulation of the node and the occurrence of thrombosis. Anemia occurs due to the fact that a person begins to lose blood with each bowel movement, and with each subsequent time more and more. A lack of hemoglobin will result in weakness, rapid fatigue, and a constant desire to lie down and rest. Thrombosis of hemorrhoids is formed due to the fact that blood stagnates in the area of the body responsible for emptying. Severe pain is the main characteristic of this problem. If inflammation is added to this, then you may encounter an even greater problem - damage to the perirectal tissue.
Diagnosis and choice of treatment tactics
Diagnosis of hemorrhoids is carried out by a proctologist using a digital examination. Symptoms such as bleeding, pain, and the sensation of a foreign body in the rectum occur with cancer, as well as with other pathologies of the lower intestine.
Therefore, the general list of examinations may include sigmoidoscopy or colonoscopy, as well as laboratory tests.
At the final stage of diagnosis, treatment tactics are chosen. Acute hemorrhoids are treated conservatively, and in the chronic form of the disease they resort to surgery, giving preference to minimally invasive treatment methods.
The exception is cases when surgery is temporarily contraindicated. For women, this is pregnancy, the postpartum period, as well as situations when it is necessary to stabilize the general condition of the patient. This situation can arise during acute infections or during exacerbation of severe chronic diseases.
Basic methods for diagnosing hemorrhoids
Constipation can cause hemorrhoids
When the first symptoms appear, the best thing a patient can do is to immediately make an appointment with a proctologist. You should not waste time on “traditional medicine” on the advice of friends and acquaintances; modern diagnostic methods will allow you to identify the stage of development of the disease and prescribe appropriate measures. The main diagnostic methods used in proctology:
- Palpation. Digital examination is the simplest and most effective method for determining the stage of development of hemorrhoids and the presence of other proctological diseases.
- Anoscopy is an examination using a rectal speculum.
- Colonoscopy is a method of examining the colon using a colonoscope.
- Sigmoidoscopy is a method of examining the rectum and sigmoid colon using a retromanoscope.
In difficult cases, irrigoscopy may also be prescribed - this is the name for x-ray examination of the lower intestines. It allows you to detect the presence of cancerous tumors and other neoplasms. The doctor may also prescribe a stool test, which will make it possible to identify blood impurities, and a blood test for hemoglobin levels. With constant bleeding, anemia develops, and using a blood test, the doctor will be able to determine the stage of development of the disease.
Many people are afraid to go to the doctor precisely because of unpleasant diagnostic methods or for fear that information about the disease will become known to third parties. However, today medicine has moved forward, and most studies are carried out with minimal discomfort for the patient.
Any medical institution is obliged to keep information about patients confidential, and if you do not trust ordinary doctors, you can use the services of a paid clinic.
Methods for treating hemorrhoids without surgery
Conservative treatment of painfully enlarged hemorrhoids should be carried out comprehensively, affecting all factors contributing to the development of the disease. It is necessary to normalize the stool, because constipation and diarrhea equally seriously injure the inflamed node.
If the cause of hemorrhoids is an attack of diarrhea, every effort is made to cure the disease that caused the stool disorder. Constipation is fought with a diet that includes a large amount of dietary fiber (prunes, dried apricots, oranges, apples). For persistent constipation, mild laxatives (Duphalac) are prescribed.
In order not to irritate the intestines, spices, salt, vinegar, smoked foods, as well as carbonated drinks and alcohol are excluded from the diet.
The pain increases the spasm of the internal sphincter, which contributes to stagnation of blood in the veins. To relieve pain and spasms, use warm baths with potassium permanganate or herbal decoctions.
Painkillers, antispasmodics, blood thinners, and medications that promote tissue regeneration are prescribed as drug therapy. Preference is given to “local” therapy: ointments are used for external nodes, and suppositories for internal nodes.
Attention! The prescription of drugs depends on the location of the hemorrhoid, the stage of development of the disease, the phase of the process, the presence of concomitant diseases and the general condition of the body. Therefore, we recommend not to self-medicate, but to consult a doctor in a timely manner.
Radical treatment of pathology
Minimally invasive methods
Doctors treat chronic hemorrhoids with surgical methods. At the initial stages of the disease, preference is given to minimally invasive techniques, which are carried out on an outpatient basis (without placing the patient in a hospital) and provide for a short rehabilitation period.
An important advantage of low-traumatic operations is a short list of contraindications. The list of methods that are suitable for most patients includes: • sclerotherapy (injection into dilated veins of substances that cause “soldering” of the walls of dilated veins); • infrared coagulation (cauterization of the leg of the node); • ligation of the internal hemorrhoid with latex rings.
Sclerotherapy and infrared coagulation are used at stages I – II of the development of internal hemorrhoids. The effectiveness of these methods at stage I is 85%, and at stage II – about 72%. If the node is ligated with latex rings, the effectiveness exceeds 93%.
Operation hemorrhoidectomy
Hemorrhoidectomy is the removal of enlarged hemorrhoids using surgical methods, that is, using a scalpel.
Such treatment must be carried out in a hospital. The rehabilitation period is much longer and is less well tolerated by patients. Therefore, surgical removal of nodes is carried out only in the last stages of the disease , when minimally invasive techniques are no longer effective.
Hemorrhoidectomy can be combined with disarterization of hemorrhoids under ultrasound control. This method is often used for stage III internal hemorrhoids.
The choice of surgical intervention method depends on the number of enlarged nodes, their location, as well as the presence of complications and concomitant pathologies.
Hemorrhoids: types, stages, treatment
Shlosser Kirill Vladimirovich
Surgeon, Proctologist
April 30, 2021
Hemorrhoids are a pathological expansion of cavernous (that is, cavernous or spongy in structure) vascular plexuses located in the anus, with the formation of external and/or internal nodes.
Causes of hemorrhoids
- A lifestyle associated with prolonged static loads: hemorrhoids are an “occupational” disease of drivers, office workers, security guards, etc.
- Excessive physical activity, heavy lifting, sudden tension.
- Excessive consumption of alcohol, spicy and pickled foods.
- Constipation, straining with difficulty defecating (defecation).
- Pregnancy and childbirth.
- Heredity.
Symptoms of hemorrhoids
- Discomfort or pain in the anus.
- Sensation of a foreign body in the anal canal.
- Discharge of blood during bowel movements, blood in the stool.
- Nodes in the anal area.
Classification of the disease
Acute hemorrhoids are thrombosis of hemorrhoids. The external manifestation is a dense, painful external or internal bluish-colored node filled with a blood clot.
Acute hemorrhoids are divided into three degrees of severity:
I degree – Thrombosis of external or internal hemorrhoids without an inflammatory process.
II degree – Thrombosis, complicated by inflammation of hemorrhoids.
III degree – Thrombosis of hemorrhoids, complicated by inflammation of the subcutaneous tissue in the perianal area.
Therapeutic tactics involve both complex conservative treatment and surgical treatment.
The indication for surgical treatment is acute thrombosis of the hemorrhoid. In the early stages of the disease, optimally up to 72 hours, thrombectomy is indicated - removal of thrombotic masses. Performed on an outpatient basis. The operation leads to a significant reduction in treatment time.
In later stages, either removal of the thrombosed node or conservative treatment followed by planned surgery is possible. Hospitalization is indicated for stage III of the disease, when the inflammatory process spreads to the surrounding tissues of the perianal region and anal canal.
Stages of disease development
Chronic hemorrhoids are divided into four stages.
Characteristic symptoms:
Stage I – Periodic bleeding from the rectum without prolapse of hemorrhoids. The method of treatment is conservative therapy.
Stage II - Hemorrhoids fall out during defecation, but are reduced on their own. There may or may not be bleeding. It is also possible for nodes to fall out during intense physical activity.
The second stage combines conservative treatment and minimally invasive proctological manipulations, which are carried out by Medical specialists in an outpatient setting.
Stage III – Manual assistance is required to reduce the nodes into the anal canal. Bleeding becomes more profuse, and periodic inflammation of the hemorrhoids is observed.
Treatment is surgical. The operations are performed by proctological surgeons at the Medical Outpatient Surgery Center.
IV – Hemorrhoids are constantly in a prolapsed state. This is the most difficult stage. Prolapse occurs even with the slightest stress: change in body position, coughing, release of gas from the intestines. The walls of the node are constantly injured and inflamed.
Only surgical treatment is indicated.
Treatment of hemorrhoids
Methods for diagnosing proctological diseases
- During an external examination, the doctor pays attention to the shape of the anus, its gaping, scar changes or deformations, fistulous openings, the condition of the skin and mucous membrane of the anal canal when straightening the folds. It determines the severity of external hemorrhoids, the stage of the disease, the degree of bleeding and prolapse of the nodes, the possibility of their independent reduction into the anal canal, and evaluates the anal reflex.
- Digital examination helps determine the tone of the sphincter, the presence of neoplasms, mucosal defects and the degree of their pain.
- Anoscopy is performed using a special disposable anoscope device, which allows you to examine the inner surface of the rectum and anal canal up to 10 cm. The procedure is painless, preparation is not required. Using anoscopy, a proctologist can assess the condition of internal hemorrhoids, the presence of inflammatory changes in the mucosa, detect anal canal polyps, mucosal defects, blood clots and possible sources of bleeding.
- Sigmoidoscopy is an examination of the rectum and distal sigmoid colon up to 25 cm using a special endoscopic device that allows you to assess the condition of these sections from the internal lumen of the intestine.
Thanks to a complex of diagnostic tests, a specialist can identify not only hemorrhoids, but also concomitant diseases.
Conservative treatment of hemorrhoids
The therapy is based on a specialized diet aimed at normalizing stool. The patient's diet should include foods rich in plant fiber and plenty of liquid. The doctor also prescribes medications that stimulate bowel movements.
To relieve inflammation, ointments, creams and suppositories with an anti-inflammatory combined effect are used. Therapy is supplemented by taking phlebotonics - drugs that increase the tone of the vascular wall.
In case of severe bleeding, local and general hemostatic (hemostatic) agents are prescribed.
For the conservative treatment of hemorrhoidal thrombosis, combined local agents with analgesic, anti-inflammatory, absorbable, and decongestant effects are used.
Minimally invasive methods of surgical treatment of hemorrhoids
- Sclerosation of hemorrhoids
Indications for surgery are chronic hemorrhoids of stages I–II, accompanied by bleeding.
A special substance – sclerosant – is injected into the lumen of the hemorrhoid using the thinnest injection needles. This drug glues the walls of the vessels inside the node, preventing further progression of the pathology. The operation is performed in an outpatient clinic.
Contraindications:
– Thrombosis of hemorrhoids
– Paraproctitis
– Anal fissure
- Ligation of internal hemorrhoids
Indicated for chronic hemorrhoids of degrees II and III, if the nodes are located separately from each other and have clearly defined boundaries.
The operation is performed in an outpatient setting. A latex ring (ligature) is placed on the base of the internal node, the nutrition of the node is disrupted and it is rejected along with the ligature after 7-10 days. Ligation of several nodes at once can cause pain, low blood pressure and bradycardia in the patient, so the procedure is usually performed at 2-3 week intervals.
Surgical treatment methods performed at the Medical Center
- Laser vaporization of hemorrhoids
It is performed for chronic hemorrhoids of stages II and III. Also suitable for the treatment of small external hemorrhoids. The operation is performed using a Milon-Lakhta surgical laser, which destroys (evaporates) fluid-rich hemorrhoidal tissue, while preserving the mucous membrane. The light guide is inserted into the lumen of the internal hemorrhoid through a small 1-2 mm puncture of the anoderm. The manipulations are performed under general anesthesia in the Outpatient Surgery Center of our clinic.
Advantages of the technique:
– Reduced operation time.
– Significant reduction in pain intensity in the postoperative period compared to classic hemorrhoidectomy.
– Significant reduction in the healing time of surgical wounds and punctures.
– More comfortable course of the postoperative period and rapid recovery of work capacity.
Contraindications:
– Stage IV hemorrhoids
– Purulent and oncological diseases of the rectum
- The Milligan-Morgan hemorrhoidectomy operation is indicated for stages III–IV of chronic hemorrhoids
There are two main types of hemorrhoidectomy: open and closed.
Open surgery is performed under general anesthesia in the operating room. The doctor alternately stitches and ties the vascular legs of the nodes and then removes the external and internal hemorrhoids. Postoperative wounds are not sutured. Next, the surgical site is injected with a local anesthetic, and an absorbable tampon with an anesthetic is placed in the anal canal.
A closed operation is performed in the same way as an open operation, but after removing the nodes, the wounds of the anal canal are sutured with absorbable suture material.
Also, a similar operation is performed using a high-frequency ligation device LigaSure. It is considered open. LigaSure allows the operation to be performed almost bloodlessly, since the device automatically coagulates (seals) large vascular formations that make up the hemorrhoid. The nodes are excised down to the vascular pedicle, and after “welding” the pedicle, they are finally removed.
Advantages of the technique:
– The operation goes faster.
– Reduced blood loss during surgery.
– The risk of bleeding in the postoperative period is reduced.
– Recovery after surgery is faster.
Postoperative treatment of hemorrhoids takes place in an outpatient clinic. The proctologist observes, makes dressings, gives nutritional recommendations and prescribes medications for the recovery period.
Experienced medical proctologists will be happy to help you solve your problems.
Treatment during pregnancy and after childbirth
Treatment of hemorrhoids in pregnant women and in the early postpartum period does not involve surgical intervention. The fact is that the reasons for the dilation of the veins of the rectum during this period are physiological in nature: • changes in hormonal levels; • increased intra-abdominal pressure; • increase in circulating blood volume; • straining during childbirth.
After childbirth, hormonal levels gradually normalize, which leads to the disappearance of the tendency to constipation. The volume of circulating blood decreases, intra-abdominal pressure decreases, the body's defenses are restored and all conditions for recovery are created.
Therefore, in most cases, a painful node that occurs during pregnancy or after childbirth disappears on its own under the influence of standard methods of conservative treatment.
Attention! When conservatively treating hemorrhoids in pregnant women, as well as in women during lactation, care should be taken. Some active ingredients of topically applied drugs still enter the bloodstream and can harm the child. Therefore, treatment must be done under the supervision of a physician.
Is it necessary to treat stage 1 hemorrhoids?
To treat or not to treat hemorrhoids at stage 1 depends on the symptoms. If there is severe discomfort, itching, and blood appears during bowel movements, then it is necessary to treat. As a rule, treatment begins with the regulation of nutrition. To avoid constipation, you need to follow a diet: eat more fiber (fruits, vegetables, legumes, cereals) and maintain water balance; it is recommended to drink at least 2 liters of clean water per day. Next, conservative treatment of hemorrhoids may be prescribed - topical medications, physiotherapy. If conservative treatment has no effect, minimally invasive non-surgical methods are used.
If you were diagnosed with stage 1 hemorrhoids during a routine examination, or the symptoms are so minor that they do not cause discomfort, there is no bleeding, and you feel well, then there is no need for treatment. After all, as we wrote above, the treatment of stage 1 hemorrhoids is symptomatic. It is necessary to adjust the diet so as not to provoke constipation, and maintain physical activity.
The main problem is that, having discovered such symptoms as blood, pain, discomfort in the rectum, people themselves diagnose themselves with hemorrhoids and begin to self-medicate. This is absolutely not worth doing! Besides hemorrhoids, there are many other diseases with similar symptoms. Because of the fear of visiting a proctologist, you can even reach the fourth stage of hemorrhoids, not to mention more serious diseases. Only a doctor at an appointment can make a correct diagnosis. Believe me, in fact, a proctological examination in modern clinics is absolutely not a problem that you need to worry about. In medical diagnostics, diagnostics are carried out absolutely painlessly, using local anesthesia, in the most comfortable conditions for the patient. As for the treatment itself, several painless procedures may be required.
Take care of yourself, do not advance the disease, because treating hemorrhoids in the early stages is always easier and faster.
Reviews from patients about the operation
We analyzed patient reviews about the rehabilitation period after hemorrhoid removal. The analysis showed that the severity of pain, difficulty with defecation and bleeding after surgery depends on the size and number of nodes removed.
Patients who have consulted a doctor with a single small node speak of surgical intervention as a completely tolerable procedure, with a short rehabilitation period.
When it comes to several large nodes, treatment will be lengthy. If the doctor recommends a minimally invasive method, you will have to remove one node per week, so the healing process will take several weeks. A surgical operation will remove all pathological elements at once, but in this case the rehabilitation period may also take several weeks.
Therefore, we recommend that you consult a doctor in a timely manner in order to intervene at an early stage of the disease. Additional information about preparing for surgery and rules of behavior during the rehabilitation period can be read in the article “Treatment of hemorrhoids in men.”
Further development of the disease
The question is often asked: what will happen if hemorrhoids are not treated? If the first signs are not clearly expressed, a person prefers to ignore them rather than go to the doctor with an unpleasant problem. However, delay can lead to complications and very unpleasant signs that can make life unbearable. Among them:
- Progressive inflammation with the formation of edema. It is difficult for the patient to sit; hemorrhoids constantly remind of themselves. Swelling may be accompanied by mucus secretion, accompanied by constant itching and burning.
- Sharp cutting pain during defecation. They talk about the appearance of anal fissures or the beginning of thrombosis. Such pain is one of the most obvious signs of hemorrhoids; when they appear, delay in treatment becomes truly dangerous.
- Nodes falling out. If damaged hemorrhoids are located near the sphincter, they may appear outward during bowel movements, and the patient has to manually reset them. Prolapse of nodes is a common symptom of hemorrhoids during pregnancy.
- Frequent constipation. Growing hemorrhoids do not allow innervation of the sphincter, so there is no urge to defecate. This further aggravates the problem, as there are even greater difficulties with bowel movements and digestion.
The further course of the disease is determined by the actions of the patient. If you start the treatment prescribed by your doctor, you can stop the development of the process and eliminate most of the unpleasant symptoms. If you postpone the problem “for later,” severe rectal bleeding, the formation of cancerous tumors and other serious complications are possible.
An additional factor that aggravates the course of the disease is treatment with numerous “folk remedies”. At best, they simply do not help, and the time for real treatment is delayed. Otherwise, they can lead to additional damage to the sphincter and rectum, which will only aggravate the patient’s condition and accelerate the development of complications.
Relapse Prevention
If you have already had hemorrhoids removed, there is an increased risk of the disease returning. To protect yourself from relapse, you should follow the recommendations of doctors: 1. Watch your stool (it is advisable to achieve daily morning bowel movements). 2. Be careful with “weight loss” diets (see point 1). 3. If you have a sedentary job, do gymnastics regularly. 4. Treat diseases of the gastrointestinal tract and pelvic organs (gastroenterology, urology, gynecology) in a timely manner. 5. Avoid physical and nervous overload.
Nature has prepared a woman for childbirth, so the venous vessels of the rectum in women are more resistant to stress than in men. If you follow the rules, the disease will not return.
Is it possible to cure chronic hemorrhoids with folk remedies?
Unfortunately, chronic hemorrhoids cannot be cured using conservative methods. “Folk” methods give a short-term effect. Similar results will be obtained with “home” drug treatment.
The unpleasant symptoms of the disease may disappear for a while, but the disease will develop unnoticed by you. In the future, the following complications may develop: • anal fissure; • anemia; • nervous exhaustion; • infectious processes (proctitis, paraproctitis, etc.).
It should also be noted that under the mask of hemorrhoids a deadly disease such as rectal cancer . Therefore, if alarming symptoms appear, you should urgently consult a doctor to find out an accurate diagnosis and begin adequate treatment.
Don’t waste time on self-medication, come to an appointment with a proctologist!