Liver hemangioma - what is it?
This disease is a benign vascular tumor that does not tend to degenerate into a malignant tumor. The disease is detected in 2–7% of people. Women suffer from it 6 times more often than men. This is explained by the fact that female sex hormones affect the growth of tumor capillaries.
Most hemangioma is detected in people 30–50 years old. There is no genetic predisposition to tumor formation. It is believed that certain drugs, such as estrogens and steroids, can provoke the development of neoplasms.
Visually, the tumor resembles a porous sponge soaked in blood. It does not have a capsule, it is often localized in close proximity to large veins and develops slowly.
The neoplasm does not make itself felt until it reaches a size of more than 5 centimeters. That is why it is more often discovered by chance during an ultrasound or CT scan of the liver. Hemangioma does not affect liver function or disrupt biochemical parameters.
Large tumors manifest themselves symptomatically in a nonspecific manner. The main manifestations are a feeling of heaviness in the right side that does not go away, or pain.
What is liver hemangioma
A hemangioma (also known as an angioma) of the liver is a benign tumor that consists of clusters of small vascular cavities filled with blood.
5% of the adult population have this diagnosis. These neoplasms are more common in adults than in children: the typical age of patients is 30 - 50 years. Liver hemangiomas are more common in women than in men.
Most liver hemangiomas do not cause symptoms, although larger lesions that press on the tissue may cause poor appetite, nausea, and vomiting.
As a rule, the patient develops only one hemangioma, but in some cases there may be several. Hemangiomas do not develop into cancer or spread to other parts of the body.
Classification
In world medical practice, there are several varieties of this tumor:
- cavernous hemangioma of the liver, which is several free cavities connected into a single one;
- capillary hemangioma of the liver forms a large number of small cavities, each of which houses a blood or venous vessel.
Along with the most common ones, venous, cluster-shaped hemangioma, and hemangioendothelioma can also occur.
Symptoms of liver hemangioma in adults
Most liver hemangiomas do not cause any unpleasant symptoms; they are discovered when the patient is examined for another disease.
Small (a few millimeters to 2 cm in diameter) and medium-sized (2 to 5 cm) are not treated, but should be monitored regularly. Such monitoring is necessary because about 10% of hemangiomas increase in size over time for unknown reasons.
Giant liver hemangiomas (more than 10 cm) usually have symptoms and complications that require treatment. Symptoms most often include pain in the upper abdomen as the large mass presses on the surrounding tissue and liver capsule. Other symptoms include:
- poor appetite;
- nausea;
- vomiting;
- quick feeling of fullness while eating;
- feeling of bloating after eating.
Liver hemangioma may bleed or form blood clots that trap fluid. Then abdominal pain appears.
Complications
Despite the fact that hemangioma does not turn into cancer, its complications are very serious. The most common of them:
- A rupture occurs and internal bleeding begins;
- Thrombosis develops and the tumor thickens;
- When the tumor size is significant, compression of nearby organs and blood vessels occurs.
The development of the tumor is largely influenced by the content of estrogen in the blood, so it is necessary to monitor its development during pregnancy or during the use of hormonal contraception.
Diagnostics
There are a number of tests that help distinguish liver hemangioma from other types of tumors:
- contrast-enhanced ultrasound - high-frequency sound waves pass through body tissue, and echoes are recorded and converted into video or photographs;
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- angiography - a contrast agent is injected into the vessels to look at them under X-ray irradiation;
- scintigraphy is a nuclear scan that uses the radioactive isotope technetium-99m to form an image of the hemangioma.
Nutrition
Nutrition for liver hemangioma plays a significant role in getting rid of it. The patient is required to be prescribed a diet so as not to provoke a worsening of the situation (sharp proliferation of atypical cells).
A diet for liver hemangioma in adults and children involves excluding from the diet such foods as:
- carbonated drinks;
- alcohol and low-alcohol drinks;
- any chocolate;
- egg yolks;
- hot spices;
- pears, melons;
- fresh bread.
You should limit your consumption of fatty, fried, smoked, and salty foods.
Instead, you need to focus on:
- low-fat fish;
- liver;
- dairy products;
- viscous porridge;
- vegetables;
- not sour fruits.
Vitamin B12 may be additionally prescribed.
Modern methods of treatment
Some hemangiomas are diagnosed at birth or in early childhood (up to 5 - 10% of one-year-old children).
Hemangioma usually shrinks over time and in some cases may disappear. If it is small, stable and not causing any symptoms, it can be monitored with imaging studies every 6 to 12 months. There are no medications to treat liver hemangioma. Surgery may be necessary to remove the tumor if it is growing quickly or causing significant discomfort or pain. A technique called vascular embolization, in which the blood vessels supplying the hemangioma are closed, can slow or reverse its growth.
How is an MRI done?
Diagnostics are carried out in closed-type tomographs. Before the examination begins, the doctor will tell you about some of the features of MRI. This is especially true if the patient is to undergo the study for the first time.
- The patient must lie still during the examination. The slightest movements can reduce the information content of the procedure.
- Closed CT scanners make a loud noise, which can be frightening for some patients. If you are one of them, take earplugs with you.
- There is lighting and ventilation inside the tomograph. Also, the patient will be able to contact a specialist at any time using a speakerphone.
- If you feel unwell, you can use the panic button and pause the examination process.
Popular questions and answers
We asked X-ray endovascular surgeon Alexander Shiryaev to answer questions about liver hemangioma.
What complications can occur with liver hemangioma?
Liver hemangioma can lead to tissue rupture, internal bleeding, and hemorrhagic shock. There is a possibility that due to the large size of the formation, nearby organs, vessels and nerves may be compressed.
When is surgery needed for liver hemangioma?
The choice of treatment tactics for hemangioma largely depends on its size and shape.
Tumors measuring 4 - 6 cm (in volume) do not require surgical action. In this case, the patient’s condition is simply monitored; after 3 months from the moment of detection, ultrasound control is performed, and then it is repeated every 6 to 12 months. In a more complex situation, the specialist will select hormonal therapy, radiation therapy or surgery.
Reasons for appearance
Signs of liver hemangioma can be felt by absolutely everyone, regardless of age or gender. However, it is noted that in women it can grow more intensely due to increased levels of the hormone estrogen.
Despite the huge amount of research conducted on this formation, the exact cause of its appearance has not yet been identified. Medical scientists believe that the prerequisites are formed during the intrauterine period of fetal development.
There is an opinion that the proliferation of cells that subsequently form liver hemangioma is activated as a result of hemorrhages suffered by the body, as well as a tendency to enlarge capillary and venous vessels and thrombosis.
Why does hemangioma appear?
There is an opinion that hemangioma occurs in a small child as an anomaly of the vascular venous bundle as a result of a violation of the formation of blood vessels in the embryonic state. There are supporters:
- inflammatory theory (author R. Virchow);
- connections with vasodilation after necrosis (author Ziegler);
- cavernous ectasia or cavity formation (by Schmieden).
The theory of impaired embryogenesis of the vascular system is the most popular. There is a delay in temporary vascular channels. Oncology specialists recognize all the signs of a tumor process in liver hemangioma.
It has been established that the pathology is formed in utero during the first trimester of the mother's pregnancy. This is the period of formation of large vessels and blood networks in the fetus. The impact of unfavorable factors on a woman’s body leads to neoplasm. The specific causes of liver hemangioma are not yet clear.
Factors that cause disruption of the correct process of formation of blood vessels in the liver include:
- bad habits of the expectant mother (smoking, drinking alcohol and drugs);
- forced treatment during pregnancy with potent drugs (estrogens, steroids, Clomiphene, human chorionic gonadotropin);
- exposure to radioactive radiation;
- concomitant damage to the liver tissue with other defects and developmental anomalies;
- hereditary predisposition; cases of family origin among close relatives have been reported.
Multiple neoplasms are more dangerous and difficult to treat
Results of MRI, ultrasound and computed tomography
In this case, consultation with a gastroenterologist without preliminary diagnosis is of little use, since in most cases hemangioma has no visible signs and can only be detected during various types of diagnostic measures. Examinations that allow you to see a hemangioma and determine its diameter are:
- ultrasonography. Liver hemangioma on ultrasound is often noticeable in the liver parenchyma in the form of a round formation with heterogeneous contents and clear contours;
- MSCT of the abdominal cavity;
- hepatoscintigraphy is a method that allows you to examine soft tissues for malignancy. A biopsy for this diagnosis is prohibited, since damage to the tumor can cause massive internal bleeding, since the tumor itself consists of blood vessels;
- MRI and CT scan of the liver and biliary tract. These studies allow us to see the tumor more accurately from different angles. Before these examinations, the patient must be injected into a vein with a special drug - contrast, since liver hemangioma on CT with contrast is outlined more clearly, and the chance of confusing it with another neoplasm is significantly reduced.
Doctors at the Yusupov Clinic are constantly improving their skills, which allows them to stay up to date with the latest methods for studying liver diseases. Our doctors are competent and attentive to drawing up a treatment plan for each patient, because only an individual approach to recovery gives the expected results.
MRI with contrast
A contrast agent is usually necessary when diagnosing liver hematoma, since some important characteristics of a hemangioma are revealed precisely by the administration of contrast.
This makes it possible to examine in detail both the liver itself and the features of the pathology. Before starting the procedure, the doctor injects a drug with a contrast agent into the patient’s vein. This manipulation significantly increases the diagnostic information content.
Contrast is safe for the body; the drug does not accumulate in tissues. Literally within a day the drug is completely eliminated from the body. In order for the substance to leave the body as quickly as possible, it is recommended to drink more water. Contrast studies can only be performed if there are no contraindications.
Introduction
The prevalence of liver hemangiomas in the population, according to autopsy studies, reaches 7.3% [19]. These tumors are the most common benign liver tumors. The availability of modern non-invasive radiation diagnostic methods has led to the fact that hemangiomas are often detected by chance. Imaging methods such as CT and MRI can help clarify the diagnosis, but sometimes this is not possible. A persistent suspicion of a malignant tumor may be the basis for surgical intervention. Clinical symptoms, which usually appear when the tumor reaches gigantic proportions, serve as another indication for surgery. The severity of symptoms does not always correspond to the volume of formation. Some researchers do not focus on absolute size when determining indications for surgical treatment and consider tumor growth to be a more important factor.
With stable tumor sizes and the absence of symptoms, monitoring patients is safe even with gigantic hemangiomas, since most tumors do not grow, and the risk of complications does not exceed the risk of surgery [18, 28, 30]. This opinion is based on studies of fairly large groups of patients, but the small number of such studies and short follow-up periods make this position debatable. Another subject for discussion is the choice of the extent of intervention (resection or enucleation). There are few comparative studies on this topic.
Uncertainty regarding the behavior of hemangiomas over time, their ability to grow and develop complications, and the lack of a clear position regarding the tactics of managing patients with giant asymptomatic tumors prompted us to analyze our own experience.
Material and methods
The study included patients with liver hemangiomas who were operated on or consulted in the Department of Surgery of the Liver, Biliary Tracts and Pancreas of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky from 1987 to 2011. In the group of operated patients, the diagnosis was confirmed by histological examination of the removed specimen. In the group of observed patients, the diagnosis was established based on data from at least one of the research methods (ultrasound, CT, MRI, angiography) or biopsy. Demographic and clinical data, results of laboratory and instrumental research methods, intraoperative and immediate postoperative indicators were extracted from medical histories and outpatient records. Long-term results of treatment and follow-up were studied through outpatient examination of patients or questionnaires (by mail, by telephone). In the questionnaires, patients were asked to assess their condition and provide data from recent studies performed at their place of residence or at the Republican Scientific Center for Surgery.
Quantitative data are presented as median (lower - upper quartiles, range) - Me (Q1-Q2; min.-max.). Quantitative characteristics were compared using the Mann-Whitney test, qualitative characteristics - using the χ2 test or Fisher's exact test (with the number of observations in the group <5). Differences between groups were considered statistically significant at p<0.05.
results
During the noted time period, 178 patients with liver hemangiomas came to our department. The average age of patients at the time of treatment was 48±10.2 years (from 24 to 76 years). Women predominated - 79.2% (141 out of 178). The female to male ratio was 3.8:1. 54.5% (97 of 178) of patients had complaints, the main of which were pain (70.1%; 68 of 97) or a feeling of heaviness (23.7%; 23 of 97) in the right hypochondrium and epigastric region, nausea ( 8.2%; 8 of 97) and early satiety (5.2%; 5 of 97) during meals. Unexplained fever (5.2%; 5 of 97), general weakness (2%; 2 of 97), and shortness of breath (2%; 2 of 97) were rarely observed. The median duration of complaints before contacting the Republican Scientific Center for Surgery was 14 months (5-36; from 0.5 to 240 months). Patients with symptoms did not differ from patients without symptoms in the size of the largest tumor: 71 mm (47-100; from 9 to 350 mm) and 70 mm (42-93; from 6 to 180 mm), respectively (p = 0.3) . The incidence of symptoms also did not depend on the location of the tumor (right or left lobe): 51.8% (59 of 114) and 62.3% (33 of 53), respectively (p=0.2).
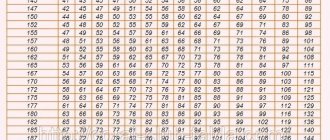
The main demographic and clinical indicators are presented in table. 1.
Single hemangiomas were observed in 50% (89 of 178) of patients, from 2 to 3 tumors - in 41.6% (74 of 178), 3 or more - in 8.4% (15 of 174) of patients. A total of 322 liver hemangiomas (from 1 to 9), the size of which was 36.5 mm (19-76; from 4 to 350 mm), were found in 178 patients. In almost half of the cases (48.1%; 155 out of 322), the tumor size was ≥4 cm, in 14.9% (48 out of 322) it was equal to or greater than 10 cm. The median of the largest tumor in a patient was 71 mm (46-100; from 6 to 350 mm).
Changes in the main biochemical blood parameters were observed in 31.5% (56 of 178) of patients. The most common abnormalities were an increase in the level of transaminases, bilirubin and a decrease in the prothrombin index (Table 2).
Diagnostics
For diagnosis, ultrasound of the abdominal cavity was most often used, which was performed in 84.8% (151 out of 178) of cases. The conclusion about the presence of hemangiomas was made in 49% (74 out of 151) of them. The most characteristic signs of hemangiomas were clear and uneven contours, increased echogenicity, heterogeneity of structure, avascularity and the effect of dorsal enhancement. Abdominal CT was used in 68.5% (122 of 178) of patients. This method allowed us to establish the correct diagnosis in 83.6% (102 out of 122) of them. Properties such as clear and uneven contours, reduced density, an area of reduced density in the center, as well as the characteristic globular accumulation of contrast agent from the peripheral parts with gradual spread to the center of the formation, allowed us to conclude about the presence of a hemangioma. A small number of patients (17) underwent abdominal MRI. In 94.1% (16 out of 17) of cases, liver formations were characterized as hemangiomas. Typical features were smooth and clear contours, decreased intensity on T1-weighted images, increased intensity on T2-weighted images, and a characteristic accumulation of contrast material from the periphery to the center of the tumor with intravenous contrast. Angiography was used only in 22 cases. Almost all studies (91%; 20 out of 22) were carried out before 2003. In 14 (63.6%) cases, this method made it possible to establish a correct diagnosis, in 7 (31.8%) cases the nature of the formations remained unknown. Angiography data did not allow detection of liver masses in one patient, however, ultrasound and CT revealed a hemangioma of the left lateral sector with a diameter of 50 mm. Characteristic signs of hemangiomas during angiography were reduced tumor vascularization in the early phases of the study and the appearance of “lakes” (“puddles”) of contrast agent in the peripheral parts in the parenchymal phase of the study. When there was doubt about the diagnosis, in 8 cases we resorted to puncture biopsies, the informative value of which was 50% (4 out of 8). In 2 patients, intra-abdominal bleeding occurred after a puncture biopsy, which required laparotomy and bleeding control.
Surgical treatment group
Surgical treatment was performed in 50 (28%) of 178 patients. Most patients had surgery after 2000 (72%; 36 of 50). The largest tumor size in this group was 100 mm (80–140; 20–350 mm). The most common indication for surgery was the presence of symptoms (42%; 21 of 50), among which a feeling of discomfort or heaviness in the right hypochondrium (66.7%; 14 of 21) and pain (42.9%; 9 of 21) predominated. Unexplained fever (23.8%; 5 of 21), shortness of breath (9.5%; 2 of 21), and epigastric fullness after eating (4.8%; 1 of 21) were less common. Uncertainty of diagnosis, i.e. suspicion of a malignant tumor was an indication for surgery in 24% (12 out of 50) of patients. The third most common indication for surgery was hemangioma growth, which was observed in 8 (16%) of 50 patients. The tumor diameter at the time of detection was 51.5 mm (40-80; 30 to 100 mm). During the observation period (from 12 to 123 months), the hemangiomas increased to 115 mm (87-170; from 45 to 280 mm). At the same time, the growth rate was 13.3 mm (4.4-35; from 1.4 to 50 mm) per year. In 5 (10%) of 50 cases, chronic calculous cholecystitis was the main indication for surgery, and hemangiomas were removed simultaneously. 3 (6%) of 50 patients had no complaints. The decision to remove hemangiomas was made due to the large size of the formations (75, 100 and 120 mm). In one patient, the reason for surgical intervention was intra-abdominal bleeding that occurred after a diagnostic puncture.
Surgical treatment was performed by liver resection or enucleation of hemangioma. The decision to choose one method or another was made during surgery, focusing on the location of the tumor. When the tumor is located in the anterior segments, preference was given to enucleation. Liver resection was performed when the tumor occupied almost the entire lobe or was located in the posterior segments.
Liver resection was performed in 38 (76%) of 50 patients: bisegmentectomy (II-III) - 13, right hemihepatectomy - 8, extended right hemihepatectomy - 6, left hemihepatectomy - 1, atypical resection of 1-2 segments - 10. In 12 (24 %) of 50 cases performed enucleation of liver hemangioma. There were no statistically significant differences in tumor localization, tumor size, operation duration, and use of the Pringle maneuver between enucleations and liver resections (Table 3).
Tumor enucleations were accompanied by less blood loss: 300 ml (200-400; from 70 to 600 ml) versus 550 ml (300-1800; from 100 to 5000 ml) with liver resection (p = 0.008). The rate of complications after liver resections was higher than after tumor enucleation (26.3 and 16.7%, respectively), but the differences were not statistically significant (p=0.7). The number of hospital days after liver resection was greater: 14.5 (10-20; from 7 to 72) versus 8.5 (8-12.5; from 7 to 23) after tumor enucleation (p=0.016). One patient died after liver resection (the operation was performed in 1990). There were no deaths after enucleation. Overall mortality after surgery was 2% (1 in 50). The diagnosis (cavernous hemangioma) was confirmed by morphological examination in all cases. In the presence of multiple hemangiomas located in different segments of the liver, only the largest of them were removed. Tumors (from 1 to 5) were left in 40% (20 out of 50) of patients. The diameter of the remaining hemangiomas averaged 15 mm (10-21; from 5 to 63 mm).
Observation group
The observation group included 128 (72%) of 178 patients. 46.9% (60 out of 128) of them had symptoms at presentation that were mainly dyspeptic in nature (pain, heaviness in the right hypochondrium and epigastric region, nausea, bitterness in the mouth). Pain was the main complaint (78.3%; 47 of 60) and was described by patients as aching, dull or paroxysmal. Often the pain appeared after eating. When analyzing concomitant diseases, in 51.7% (31 out of 60) of patients with symptoms, diseases were identified that could be the cause of the complaints: cholelithiasis (38.7%; 12 out of 31), gastroduodenitis (38.7%; 12 out of 31), chronic colitis (25.8%; 8 of 31), peptic ulcer of the stomach and duodenum (19.4%; 6 of 31), chronic pancreatitis (6.5%; 2 of 31), gastroesophageal reflux disease ( 6.5%; 2 out of 31). In the absence of symptoms, such concomitant diseases were detected less frequently: 10% (7 of 68) and 51.7% (31 of 60), respectively (p<0.001). The diameter of the largest tumor in the group of observed patients was 60 mm (40-85; from 6 to 184 mm).
A comparison of the groups of operated and observed patients revealed differences in the following indicators: the presence of symptoms, the size and location of tumors. In the group of operated patients, there were more women and patients with symptoms, the tumors were larger, and patients with left-sided tumor localization were more common (see Table 1).
Long-term results
Long-term results were observed in 50% (89 out of 178) of patients. The follow-up period was 55 months (26-104; from 3 to 252 months). In the operated group, 70% (35 out of 50) of patients were followed for 52 months (22-90; from 3 to 252 months). In 88.5% (23 out of 26) of those operated on, the symptoms that were present before surgery disappeared. In 3 (11.5%) of 26 observations, symptoms (discomfort, heaviness in the right hypochondrium after eating) persisted. Complaints appeared in 1 (11.1%) of 9 patients who initially had no symptoms. No recurrence was observed in any observation after tumor removal. In 8 of 16 patients with small hemangiomas left behind, the size of the tumors did not change, in 4 (25%) cases tumor growth was noted (by 6-33 mm over 26-125 months), in another 4 (25%) cases the tumors disappeared (no longer determined by ultrasound).
In the observation group, 42.2% (54 of 128) of patients were followed for 56.5 months (29-156; from 12 to 232 months). In 84% (21 out of 25) of patients who had symptoms, the complaints noted at the time of diagnosis of hemangiomas disappeared. The majority of patients without symptoms (89.7%; 26 out of 29) did not note negative changes in their health. Only 3 (10.3%) patients developed periodic pain in the upper abdomen. The size of hemangiomas remained the same in 85.2% (46 of 54) patients, increased by 13-38 mm during 46-227 months in 11.1% (6 of 54) patients, decreased by 17 and 26 mm during 98 and 76 months in 3.7% (2 of 54) patients. One of the patients, whose tumor grew (by 38 mm) and had complaints, had the hemangioma removed in another medical institution.
Discussion
Liver hemangiomas are more often detected in women aged 30-50 years [10, 34]. This coincides with our data: the number of women exceeded the number of men by almost 4 times. It is believed that most tumors do not manifest clinically. Complaints were present in 54.5% of patients who contacted us. Such a large figure, naturally, does not reflect the true prevalence in the population of individuals with symptoms, since it characterizes a sample sent to the surgical department. Clinical manifestations were mainly due to the volume and pressure of the tumor on surrounding organs: pain (70.1%) and a feeling of heaviness (23.7%) in the upper abdomen. These are the most common symptoms according to other researchers [2, 3, 12]. Signs of impaired gastric emptying were observed in 13 (7.3%) people. The literature describes rare observations of unexplained fever, as well as phenomena resembling a systemic inflammatory process (fever, weight loss, anemia, thrombocytosis, increased fibrinogen and ESR levels against the background of normal leukocyte levels), in patients with giant liver hemangiomas [22, 27, 29]. We observed 5 patients with periodic increases in body temperature, all of them had large tumors (from 87 to 350 mm in diameter). There were no dangerous complications such as tumor rupture with bleeding or Kasabach-Merritt syndrome in our series.
It is logical to assume that tumor size and location influence the incidence of symptoms. It is noted that with a tumor diameter of 4 cm, complaints appear in 40% of patients; with a diameter of 10 cm, this number increases to 90% [16]. It has also been shown that in patients with symptoms, the tumor diameter in the left lobe is smaller than in the right (10.5 and 17.0 cm, respectively; p = 0.07) [15]. We were unable to identify a relationship between the frequency of symptoms and the size and location of hemangiomas. This may be due to the fact that the clinical picture observed in patients with small hemangiomas may be due not to the tumor itself, but to concomitant diseases. Thus, during a detailed examination of 87 patients with hemangiomas, 54% of them were found to have other diseases of the abdominal cavity, which were the cause of the complaints [13]. At the same time, giant tumors located intraparenchymatically in the right lobe of the liver may not affect the patient’s well-being in any way. Thus, it is necessary to carefully interpret the clinical picture when identifying a hemangioma, especially if the tumor is small.
Diagnosis of liver hemangiomas in most cases does not present any particular difficulties, since the tumor has a number of characteristic signs on the basis of which a diagnosis can be confidently made. Among the diagnostic methods, ultrasound is the most accessible and cheapest (we used it in 84.8% of patients), but the sensitivity of the method (49%) leaves much to be desired. It is known that the use of echo contrast agents can increase the information content of the method [36], but there is no personal experience in their use. The sensitivity of abdominal CT in detecting liver hemangiomas was 83.6%. The characteristic gradual accumulation of contrast agent by the tumor (from the periphery to the center) is pathognomonic for hemangioma, so the importance of intravenous contrast should be noted. MRI of the abdominal cavity has the highest sensitivity (more than 90%) and specificity (90-100%) among non-invasive research methods [13, 24, 31, 32]. Our data indicate the same thing: in 94.1% of patients, the method allowed us to make a correct diagnosis. The availability and high information content of CT and MRI have given us the opportunity to almost completely abandon angiography and puncture biopsy. The diagnostic capabilities of the latter need to be given special attention. There are large series of observations in which percutaneous biopsy of hemangiomas under ultrasound or CT guidance was not accompanied by complications [17, 35]. Our experience in this matter is more modest (n=8) and less successful. Intra-abdominal bleeding requiring laparotomy for hemostasis occurred in 25% of patients. Due to the risk of hemorrhagic complications, we consider it justified to resort to puncture biopsy only after using all non-invasive research methods (ultrasound, CT, MRI), if doubts remain about the diagnosis. The use of all available diagnostic methods still did not allow us to establish the nature of the formation in 6.7% (12 out of 178) of patients.
The number of patients who underwent surgical treatment in the presented work was 28% (50 out of 178). When compared with studies by other authors, this is an average figure (Table 4).
It probably could have been less, since we have been actively entering information about observed patients into the database since 2000, and many of those who were consulted in the 90s were not included in it. It is also necessary to take into account the heterogeneity of the compared groups in different studies (differences in tumor size and frequency of symptoms in patients). Once again, it should be emphasized that this information is based on an analysis of data on patients who were sent to surgical departments, and in no way reflects the treatment needs for the entire population of patients with hemangiomas.
Severe symptoms, doubts about the benign nature of the tumor, and tumor growth were the main indications for surgery in 42, 24, and 16% of patients in the surgical treatment group, respectively. This approach is also supported by other researchers who also believe that the size of the formation in itself should not be an indication for treatment, since the risk of complications even with gigantic hemangioma sizes is minimal [15, 18, 26, 30]. Nevertheless, we believe that the indications for removal of a giant asymptomatic tumor can be adjusted taking into account its location, age and physical activity of the patient. For example, if the tumor is peripherally localized in a young man, we consider surgical treatment to be appropriate. As for the term “giant hemangioma,” there is no generally accepted definition in the literature. Several threshold values have been proposed: >4 cm [5, 7, 8], >6 cm [9], >10 cm [20], >12 cm [11]. We consider hemangiomas ≥10 cm to be giant.
The only effective treatment for hemangiomas is their removal, which is achieved by liver resection or tumor enucleation. Enucleation is possible due to the presence of compacted liver tissue, which forms a clear boundary between the tumor and normal parenchyma [1, 4, 6]. The advantage of enucleation is the maximum preservation of healthy liver tissue. In addition, enucleation is accompanied by lower rates of intraoperative blood loss, the incidence of postoperative complications and bile leaks [21, 23]. Despite the small number of observations, we were able to identify statistically significant differences between enucleations and resections in terms of the volume of blood loss (300 ml versus 550 ml; p=0.008), as well as a trend towards a decrease in the incidence of postoperative complications (16.7 and 26.3; p= 0.7) and duration of surgery (190 and 265 minutes; p=0.09).
When choosing one or another method of surgical treatment, we were guided by the size and location of the tumor, performing enucleation of hemangiomas located on the periphery, usually in the anterior segments. However, if the tumor is centrally located, enucleation is also possible, although technically more difficult [14]. In our series, the proportion of patients who underwent tumor enucleation was 24%. The experience of other researchers indicates that the number of enucleations can be much higher - 30-85% (Table 5).
Surgical treatment has demonstrated high effectiveness. Symptoms disappeared in 88.5% of patients, but in 11.5% of cases complaints persisted. This is probably due to the fact that the clinical picture was due to another undiagnosed cause. The persistence of symptoms after surgery was also described by other researchers in 15-30% of patients [13, 33]. In specialized departments, the incidence of complications after removal of hemangiomas is 10-27%, and there is no mortality in most of them (see Table 5).
We were able to track long-term results in less than half of the patients (42.2%), but the follow-up period was quite long - 56.5 months (from 12 to 232 months). In 84% of cases, the symptoms that were present at the time of detection of hemangiomas disappeared. The majority of patients who had no symptoms (89.7%) did not note a worsening of their condition. A slight increase in tumor size (by 13-38 mm) occurred in only 11.1% of patients over a period of 46-227 months and did not lead to a noticeable deterioration in their well-being, with the exception of a single observation. One woman did have her hemangiomas removed in another medical institution: as the tumor grew, she developed symptoms. Thus, the stable size of most hemangiomas, the absence of complications, the rare appearance of new complaints and the disappearance of most old symptoms allow us to conclude that it is safe to monitor patients with this disease even with gigantic sizes of formations. Other researchers are also inclined to this conclusion [25, 30, 33]. There is an opinion that there is no need for regular monitoring of patients with liver hemangiomas [25]. Our position is that annual monitoring of the size of hemangiomas using ultrasound is necessary, since tumors are rarely capable of enlarging.
Thus, modern non-invasive diagnostic methods make it possible to make a correct diagnosis in most cases. Invasive diagnostic procedures (puncture biopsy, angiography) should be avoided whenever possible, as they are associated with serious complications. If clinical manifestations are present, the patient should be carefully examined, since the cause of the symptoms may be concomitant diseases of the abdominal organs. Severe symptoms, uncertainty in diagnosis and growth of hemangioma are the main indications for its removal. The gigantic size of the tumor is not an indication for surgery in itself. We believe that in the presence of a giant (≥10 cm) asymptomatic hemangioma, it is necessary to take into account such factors as the location of the tumor, the age and physical activity of the patient, the presence of concomitant diseases and, of course, the experience of the doctors in the surgical department. Taking into account the benign nature of the formation, it can be argued that postoperative mortality in liver hemangiomas is unacceptable. This places great responsibility on the surgeon when selecting patients for surgery, forcing him to carefully weigh the risks, as well as concentrate patients in specialized departments with extensive experience in the surgical treatment of liver hemangiomas.