| Way | Detailed description |
| Surgical method or extracapsular removal | The classic method of tonsil removal, which until recently was used throughout the world. The doctor uses a scalpel and wire thread. The tonsils are excised entirely, leaving difficult-to-heal wounds. Very long rehabilitation. Currently, the method is used in rare cases, for example, when there are contraindications for other methods or there is simply no necessary equipment. |
| IR laser or thermal welding | The tonsils are still excised, but this time with a powerful infrared laser (IR laser). The bottom line is that the laser hits the target and does not heat neighboring tissues. At the site of dissection, immediate tissue adhesion occurs, which entails minor blood loss and more comfortable rehabilitation. |
| Electrocoagulation | The electrical method is used quite rarely, as unpleasant consequences are possible. The excision takes place under the influence of high-frequency current, while the blood vessels are instantly sealed, and blood loss is minimal. However, electrocoagulation produces extremely high temperatures, and adjacent tissue may suffer thermal burns. |
| Carbon dioxide laser | An original method in which the tonsils simply evaporate (evaporate) under the influence of a laser. The tonsils can be reduced or removed completely. With this method, blood loss is insignificant, and recovery is comfortable. |
| Ultrasonic removal | A laser is used again, which many doctors call an ultrasonic scalpel. In this case, the tonsils are exposed to high-frequency ultrasound (over 26 kHz), which is like a sharp scalpel. Damaged vessels are sealed (coagulated). Recovery after the procedure is quite fast. |
| Cryodestruction | The tonsils are not excised using this method. Liquid nitrogen is used, which completely freezes the lymphoid tissue. The procedure itself is painless, but the rejection of frozen tissue occurs over time and is quite unpleasant. There is a possibility of repeating the procedure. |
| Microdebrider | Not the most humane type of procedure. Excision occurs with a special device (microdebrider), on the head of which sharp blades are placed. Rotating at great speed, they cut off the tonsil. Partial excision is possible. The recovery is quite long. |
Safe and least traumatic methods are thermal welding, coblation and electrocoagulation. This is due to the almost complete absence of blood during the operation and subsequent problem-free healing. However, laser-based methods are not used if the child is under 10 years old. It is extremely difficult for a child of this age to sit still, which can cause serious burns to the healthy tissues of the pharynx.
Any method of tonsillectomy is not complicated; doctors have long honed such skills and techniques. The procedure itself usually takes no more than one and a half hours. The pain is treated with local anesthesia, and in extremely rare cases with general anesthesia.
The most difficult moment of the entire operation is associated with the child himself. Complete immobility is required; for this, parents can be invited to the procedure. You need to try to calm the baby down and explain that there is nothing wrong with this - the procedure is completely painless.
A correctly performed procedure does not negatively affect the child’s health. Problems can arise if healthy tonsils are removed, as they are an important part of the body's defenses. But if the tonsils themselves are a source of infection, it is hardly worth refusing the operation. If tonsillectomy does occur, during the recovery period after surgery, Imudon® helps protect against infections2.
Imudon® is the only* local immunostimulant in the form of lozenges. A detailed regimen of use is presented in the instructions for the drug.
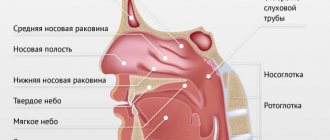
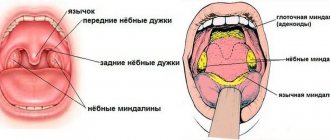
Palatine tonsils
Palatine tonsils are small structures that actually look like almond grains and are located between the arches of the palate. In common parlance they are sometimes called “tonsils.” They consist of lymphoid tissue enclosed in a connective tissue capsule. The tonsils have lacunae - slits that greatly increase the surface of the palatine tonsil. They are part of a lymphatic “ring” surrounding the pharynx. Their role is to capture “samples” of microbes entering the body with air, water and food, and report information about them to other immune organs, which produce antibodies - proteins that destroy microbes. The first “acquaintance” with the microbe occurs in the tonsils, which allows the body to fight it. This function of the tonsils is especially important in the first years of life. With age, it becomes less significant, since the same work is performed by lymphoid tissue located in the thickness of the mucous membrane throughout the respiratory tract.
The anatomical features of the tonsils and their constant contact with infection in the oral cavity create the conditions for the development of inflammation of the tonsils - tonsillitis. This inflammation can be acute or chronic.
Possible consequences of surgery for children
The likelihood of adverse events after removal of the tonsils is minimal, especially if the operation was performed in a specialized clinic. In rare cases, complications after tonsillectomy include:
- discomfort when swallowing;
- minor bleeding;
- damage to surrounding tissues during thermal excision methods;
- pain in the first time after surgery.
For the most part, all these phenomena go away on their own as the tissue heals. If the wounds have healed and the discomfort and pain have not disappeared, additional diagnostics are carried out.
The most dangerous complication is bleeding.
- In case of minor bleeding from small vessels, it is enough to treat the surface with antiseptics.
- In more serious cases, the vessel that is the source of bleeding is identified, a clamp is applied, and the bleeding tissue is sutured.
- In case of massive bleeding, tamponade is used: a gauze swab is inserted into the oral cavity and pressed against the palate under strong pressure. After 3-5 seconds, the tissue is removed to see the source of the bleeding, and then it is eliminated using a clamp and stitching. The patient is additionally administered drugs that accelerate blood clotting.
To prevent infection, a course of antibiotic therapy is prescribed before and after surgery.
Acute tonsillitis
Acute tonsillitis - tonsillitis - is most often caused by streptococci. It must be remembered that they are transmitted to others by coughing and sneezing, so a patient with a sore throat needs to be isolated - placed in a separate ventilated room, with separate dishes allocated for him.
Sore throat is an infectious disease accompanied by high fever, general weakness, aching muscles, joints, etc., with local manifestations on the palatine tonsils in the form of swelling, redness, ulcers or plaque. This pus is an accumulation of dead cells that fight the causative agent of sore throat. Often, with a sore throat, an ichorous (putrid) unpleasant odor is felt at a distance from the patient. It is emitted by dead microbes, from which the toxin has been released, placed in the pharynx and absorbed into the body through the vessels, through breathing - into the lungs, through the digestive tract. There is a powerful bacteremia - the body is filled with toxic substances and bacteria.
The danger of sore throat is that the body, fighting the streptococcus that causes sore throat, destroys its own organs. Streptococcus contains a special protein similar to some proteins in the human body. Because of this similarity, the body’s protective antibodies against streptococcus begin to attack its own tissues in the heart, kidneys, and joints. This is a complication of angina.
If a sore throat is not treated correctly, complications may include heart defects, kidney disease - glomerulonephritis, and joint damage. It is believed that the huge number of heart defects in modern 70-80 year old people is due to the fact that in the 30s, when they were children, there were no drugs to combat such microbes. These drugs were invented only in the late 30s and early 40s.
Sore throats can be complicated by a paratonsillar abscess - suppuration of the soft tissue around the tonsil. This is a very serious disease that requires hospital treatment.
It is important to note that many people often mistake any sore throat for a sore throat. Typically, a sore throat, especially a very severe one, is a sign of acute or exacerbation of chronic pharyngitis, and not a sore throat. In any case, the diagnosis of angina should be made by a doctor, preferably an otolaryngologist.
Indications and contraindications for tonsillectomy
The procedure for removing the tonsils is recommended for children if:
- frequent relapses of tonsillitis - more than 5-7 exacerbations in 2 years;
- attacks of sleep apnea;
- purulent complications with every inflammation of the tonsils;
- impaired swallowing function;
- danger of developing secondary complications - kidney, liver, heart failure, rheumatism;
- difficulty breathing;
- decompensated form of pathology.
In some cases, doctors perform not complete, but partial removal of the tonsils - tonsillotomy.
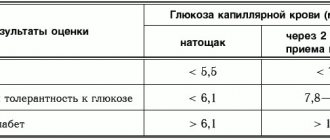
Contraindications to the procedure are divided into absolute and relative (temporary). Absolute contraindications include:
- severe hematopoietic diseases;
- diabetes;
- severe mental and psychoneurological disorders;
- active pulmonary tuberculosis;
- severe renal, liver and heart failure.
Conditions in which tonsillectomy will have to be temporarily postponed include:
- acute infectious diseases accompanied by fever and general intoxication;
- caries, stomatitis, which increase the risk of infection during surgery;
- skin rashes of various origins - dermatitis, herpes, exacerbation of atopic dermatitis.
The list of possible contraindications may include other conditions. It all depends on the age and health characteristics of the individual patient, which are fully assessed by the doctor before planning the operation.
Chronic tonsillitis
Chronic tonsillitis is an active chronic inflammatory process in the tonsils with periodic exacerbations and a general infectious-allergic reaction.
If a sore throat occurs with severe sore throat and high fever, then chronic tonsillitis may manifest itself with minor symptoms, and patients do not consult a doctor for a long time. Meanwhile, chronic infection in the tonsils leads to diseases such as rheumatism, kidney disease, heart disease and a number of others. Therefore, chronic tonsillitis must be treated.
Signs of chronic tonsillitis may include:
• Accumulation of “plugs” in the lacunae of the tonsils - whitish cheesy masses with an unpleasant odor, which are sometimes independently released from the tonsils. • A slight increase in body temperature that lasts weeks or months (low-grade fever). • Frequent sore throats. Sore throats that occur more than once a year are considered frequent.
In addition, there are signs of chronic tonsillitis, which are determined by the doctor when examining the pharynx.
Also, there is a method for determining the functional activity of the palatine tonsils, on the basis of which the doctor makes a decision - to treat the tonsils conservatively or to remove them.
Treatment of tonsillitis is aimed at combating infectious inflammation of the tonsils. Antibiotics are prescribed for this. For local effects on the tonsils, gargling with various antiseptic solutions, physiotherapy, lubrication of the tonsils, and washing the lacunae of the tonsils with antibiotics or antiseptics are used.
If conservative treatment is ineffective, surgical intervention (tonsillectomy) is used.
How to treat this disease?
The choice of treatment tactics for a patient with chronic tonsillitis is largely determined by the form of the disease.
There are several classifications of chronic tonsillitis. According to one version, there are two forms of chronic tonsillitis - compensated and decompensated, according to another version - compensated, subcompensated, decompensated. In practice, otolaryngologists use both classifications.
The compensated form of chronic tonsillitis implies the nature of the course of the disease in which complications do not develop, both local (peritonsillitis, peritonsillar abscess, cervical lymphadenitis, neck phlegmon) and distant (rheumatic heart valve disease, rheumatoid arthritis, kidney parenchyma damage), and exacerbations occur less frequently 5 times a year. This form of the disease is subject to conservative treatment, which involves courses of anti-relapse treatment 1-2 times a year, dynamic observation and evaluation of the effectiveness of such treatment.
The decompensated form of chronic tonsillitis , accordingly, includes the presence of local or distant (metatonsillar) complications listed above, as well as exacerbations of the disease more than 5 times within a year or more than 7 times within 2 years. Surgical tactics for treating patients with decompensated chronic tonsillitis is an option that significantly reduces the risk of complications or aggravation of their course. However, if it is impossible to perform surgical intervention for one reason or another, conservative treatment is justified, which does not solve the problem of decompensated chronic tonsillitis, but helps to achieve a relatively stable remission, which in turn improves the patient’s prognosis.
Tonsillectomy – “removal of tonsils”, “removal of tonsils”.
Indications for this operation are:
• frequent sore throats, severe, with high fever and prolonged low-grade fever; • unsuccessful conservative treatment; • risk of complications (glomerulonephritis, rheumatism, hemorrhagic vasculitis and other infectious and allergic diseases); • recurrent and chronic diseases of the ENT organs; • paratonsillar abscess; • endocrine diseases against the background of chronic tonsillitis; • sleep apnea syndrome caused by enlarged tonsils and adenoids.
There are contraindications for tonsillectomy. It is not recommended to operate during acute or exacerbation of chronic infectious or inflammatory diseases of internal organs and ENT organs; dental caries; hypertension; furunculosis; period of influenza outbreaks; menstruation.
Absolute contraindications are:
• blood diseases (acute and chronic leukemia, hemorrhagic diathesis; immune hemopathy and capillary toxicosis in the acute stage); • vascular anomalies of the pharynx (angiodysplasia, aneurysms, submucosal pulsation of the vessel); • severe neuropsychiatric diseases; • active form of pulmonary tuberculosis; • severe form of diabetes mellitus; • decompensated conditions in diseases of the heart, lungs, liver and kidneys.
The issue of surgical treatment of chronic tonsillitis in patients with concomitant diseases must be approached strictly individually. The final decision is made by the otolaryngologist together with the therapist.
A correspondent of the Kazanskie Vedomosti newspaper talked about this with Boris Revzin, an otorhinolaryngologist of the highest category at the ENT center of the city clinical hospital No. 16.
— Boris Arkadyevich, in what cases does the question of removing the tonsils arise? — Very often we remove tonsils when conservative treatment of chronic tonsillitis is ineffective. Chronic tonsillitis is a long-term inflammation of the pharyngeal and palatine tonsils, often accompanied by inflammation of the mucous membrane of the pharynx. If a person has frequent tonsillitis (more than twice a year), we first carry out conservative treatment. First of all, the patient is examined for microflora and its sensitivity to various medications (for this, a swab is taken from the throat). Next, rinsing of the lacunae of the palatine tonsils is prescribed to cleanse them of caseous plugs, massage of the palatine tonsils. And if this treatment does not produce results - namely, long-term remission, then in such a situation it is possible to perform a tonsillectomy - an operation to remove the tonsils.
We also perform this operation if chronic tonsillitis causes complications in the form of concomitant diseases: rheumatoid arthritis, endocarditis, inflammatory autoimmune diseases of the thyroid gland, chronic inflammatory kidney diseases.
The absolute indication for removal of the tonsils is a complication of tonsillitis such as a peritonsillar abscess. This is an acute inflammation in the peritonsil tissue, a severe purulent lesion of the oropharynx. It occurs when a sore throat is treated incorrectly, when, for example, a person does not take antibiotics or takes them incorrectly. Or in the absence of treatment for the disease.
— And how does removing tonsils solve the problem of frequent sore throat? — In cases where there are indications for tonsillectomy. The tonsils are a source of chronic infection for the body. Microbes live in their lacunae and caseous plugs are formed: waste products of these microbes, desquamated epithelium and food debris. Sometimes the tonsils, by their very structure, are very loose, with widened lacunae. In this case, food debris will often get stuck in them, which can lead to chronic inflammation.
In addition, if antibodies begin to be produced to the causative agent of inflammation, streptococcus, then after some time they attack the body’s own cells and tissues. Thus, here we are already dealing with the autoimmune nature of the disease, affecting the tissues of the heart, kidneys, liver, and thyroid gland.
— Why does the issue of removing the tonsils cause a lot of controversy and there is no consensus among doctors about whether the patient needs to take this step? What do you think about this? — Regarding tonsillectomy, there is often a lot of conflicting information in the media and on the Internet. This may be due to the fact that earlier, in the 1970s and 1980s, tonsils were removed very often; this did not always give the desired result. Now we carefully examine the patient before referring him for a tonsillectomy. Before this step, it is necessary to determine whether there are any other causes of tonsil disease. Maybe the tonsils suffer from problems of the upper respiratory tract, such as a deviated nasal septum with delayed nasal breathing and so on. Or, as often happens in the case of pharyngotonsillitis, the development of a chronic disease is provoked by the Helicobacter bacterium, which causes diseases of the gastrointestinal tract.
— What are the contraindications for this operation? - Absolute contraindication - blood diseases. Because tonsillectomy may cause heavy bleeding. Relative contraindications are severe somatic pathology: myocardial infarction, angina pectoris, severe heart and renal failure, high degree of hypertension, severe diabetes mellitus, active form of tuberculosis. You should not remove tonsils during menstruation, in the last months of pregnancy, or during acute infection. The operation is carried out no earlier than two to three weeks after suffering from a sore throat, flu or other illness.
— Can removal of the tonsils lead to a decrease in immunity? After all, they are part of the human immune system... - No, you don’t need to be afraid of that. First, we do not remove all lymphoid tissue. Lymphoid tissue is present both at the root of the tongue and in the nasopharynx. The lingual tonsil is also part of the immune system. After the tonsils are removed, they take over the function of the palatine tonsils. Secondly, diseased tonsils are no longer of any use: they do not protect a person from infection, but themselves are its source and poison the body.
— Is it true that after such an operation a person’s voice can become quieter? - No, her voice does not become quieter, except perhaps only in the first time after the operation.
— Is tonsil removal performed under general anesthesia? — We perform tonsillectomy under both local and general anesthesia. When choosing it, we look at the overall picture, the severity of the pharyngeal gag reflex. Because of this, not every patient can, in principle, have this operation without anesthesia. Therefore, if a person has a pronounced gag reflex, it is, of course, more advisable to perform a tonsillectomy under general anesthesia. Many patients themselves want to have this operation performed under anesthesia.
— How is tonsillectomy performed? — The operation lasts from 30 minutes to an hour, depending on the severity of the bleeding. This is a surgical operation during which a radio wave scalpel is used. This modern radio wave equipment can reduce bleeding. It is also used after direct cutting of the tonsils, when it is necessary to cauterize the bleeding vessels at the site of the removed organ. The radio wave coagulator does this superficially without causing severe burns.
By the way, I want to note that tonsillectomy is not the only type of surgery on the tonsils. There is also a tonsillotomy (partial removal of the tonsils), which is usually done for children if the tonsils are enlarged. And lacunotomy - when, after washing the tonsils, incisions are made on them with a radio wave scalpel in order to thus seal the recesses in the tonsils, preventing the accumulation of microbes in this organ and the formation of plugs in it.
— Is lacunotomy an alternative to tonsil removal? - No. Rather, it is an intermediate stage between conservative treatment and tonsillectomy. But, unfortunately, this method is not as effective as removing tonsils. It can be used for tonsil cysts.
— Does removal of tonsils require hospitalization? And if so, how long does the person spend in the hospital? — In the absence of any postoperative complications, patients remain in the clinic for two to three days. But even after discharge, we keep in touch with them just in case. On the first day after surgery, the patient should not talk or eat.
In the following days, in this case, a gentle diet using mainly liquid food is required. For two weeks after tonsillectomy, the patient should limit physical activity, not lift weights, not visit the bathhouse or sauna, and follow a diet.
— Do you have many patients whose tonsils are removed? “We carry out about three or four such operations a week. Many people do not want to part with their tonsils and go on rinsing ad infinitum. I would like to add that if there are indications for tonsillectomy, it is better to do it at a young age, when the body tolerates the operation more easily and complications in the form of associated diseases have not yet appeared.
Preparing for tonsillectomy (removal of tonsils)
In preparation for the operation, a clinical examination is carried out to ensure the safety of the surgical intervention: determination of blood group and Rh factor, blood test, urine test, determination of HIV and Australian antigen, sanitation of the oral cavity, in young children - chest x-ray to exclude thymomegaly; a thorough examination to diagnose diseases that may complicate the course of the operation and postoperative period; On the eve of the operation for children, a certificate is obtained from the clinic stating that there is no contact with carriers of childhood infections.
Several weeks before surgery, you should not take aspirin or medications containing it. It impairs blood clotting and increases the risk of bleeding. You need to tell your doctor if you are constantly taking any medications, if you are allergic to anything, if you have had reactions to a blood transfusion, if you have an increased tendency to bleed.
You should not eat or drink anything before the operation. This must be especially monitored if you plan to operate on a child. A light dinner is allowed the night before.
Tonsillectomy methods
Depending on the size of the palatine tonsils, the characteristics of the disease and the anatomy of the nasopharynx of a small patient, different methods of tonsillectomy are used.
- Radio wave. An operation to remove the palatine tonsils is a surgical intervention performed by otorhinolaryngologists (ENT doctors) according to strict indications, which are based on a diagnosis of chronic decompensated tonsillitis.
- Electrocoagulation. The method involves excision of affected tissue using electric current. The method is absolutely bloodless, very fast, but is associated with a fairly high risk of injury to surrounding healthy tissue due to their heating
- Ultrasonic excision. Removal of overgrown tonsils is performed using a special ultrasonic scalpel. The method is less traumatic, but there is a risk of slight bleeding.
- Radiofrequency destruction. This method of therapy is most often indicated for small tissue growths, since radio waves are not able to remove space-occupying formations. The method is also used for partial removal of the tonsils.
- Vaporization. Excision of tissue is performed using a carbon laser. The method is fast, has minimal impact on surrounding healthy tissue, and shortens the recovery time after the procedure.
- Cryodestruction. Involves freezing damaged areas with liquid nitrogen. The method is specific and requires long-term therapy and repeated procedures, but with this option of tonsillectomy the likelihood of bleeding is excluded. Cryodestruction is recommended for use in children with an increased risk of bleeding: hemophilia, severe endocrine pathologies.
- Classic tonsillectomy. It remains one of the most popular methods for removing tonsils. Involves excision of inflamed areas using a scalpel and other instruments. During the operation, the doctor also opens the foci of infection and cleanses them of purulent contents.
The operation time depends on the chosen method of operation and ranges from 60 minutes to 1.5 hours. After the tonsillectomy is completed, the child remains under medical supervision for 24 to 48 hours to monitor his well-being and prevent complications.
Surgery to remove tonsils
The operation is usually performed under general anesthesia. In extreme cases, tonsillectomy is performed under local anesthesia. For this, a solution of ultracaine is usually used. General anesthesia is usually performed using a combination of inhaled and intravenous anesthetic.
Classic tonsillectomy is as follows: after infiltration of the paratonsillar region, through an arcuate incision along the edge of the anterior arch, the upper pole of the tonsil is bluntly isolated with an elevator and grasped with forceps or a clamp. Then the tonsil is isolated with an elevator to the lower pole. The separated tonsil is removed with a special loop. Bleeding is stopped by tamponade of the niche, coagulation of blood vessels, or application of ligatures. The duration of a tonsillectomy is usually 20-30 minutes.
The numerous methods of tonsillectomy that exist today do not fundamentally change the essence of the operation. The use of lasers, radiofrequency surgery, microdebrider, and ultrasonic scalpel is aimed at reducing tissue bleeding and has virtually no effect on healing time or the severity of pain in the postoperative period.
IF YOU DECIDE TO HAVE AN OPERATION, YOU NEED TO CHOOSE THE TECHNIQUE THAT IS BEST IN THE DOCTOR YOU TRUST.
After removal of tonsils
After the operation, the patient is placed on his side in a bed with a low pillow. Drinking is allowed no earlier than after 6-8 hours.
Constant monitoring is carried out in order to timely diagnose possible bleeding. On the day of surgery, fasting is prescribed. In the following days, a gentle diet (semi-liquid and non-hot food) is prescribed. They are treated with drugs that increase blood clotting, and aerosols with anesthetics are used; in the presence of metatonsillar complications, a short course of antibacterial therapy is carried out. Bed rest is observed for 2-3 days. Fibrinous plaque in the tonsillar niches usually disappears on the 7-10th day.
Complications after tonsillectomy
The most common complication is bleeding from the tonsillar niches, mainly in the early postoperative period in the presence of concomitant diseases;
bleeding can be vascular and parenchymal. Vascular bleeding is stopped with hemostatic clamps followed by ligation of the vessel. In case of parenchymal bleeding, the niche is tamponade with hemostatic agents (if it is necessary to hold the tampon for a long time in the niche above it, the palatine arches are sutured). Other complications are extremely rare: subcutaneous emphysema, acute inflammation of the lingual tonsil, stomatitis, glossitis, acute otitis media, exacerbation of chronic diseases of the ENT organs, exacerbation of chronic diseases of the internal organs, phlegmon of the neck, paresis of the cranial nerves, pharyngeal hematoma. [/td]