Pharmacological properties of the drug Fragmin
Pharmacodynamics. The antithrombotic effect of dalteparin is associated with its ability to enhance the inhibition of factor Xa and thrombin. In general, dalteparin enhances the inhibition of factor Xa rather than prolonging the time of thrombus formation in the blood plasma. Dalteparin has almost no effect on the primary link of hemostasis since its effect on the function and adhesive properties of platelets is insignificant compared to heparin. Pharmacokinetics. Bioavailability, measured by antifactor Xa activity, was 87±6% in healthy patients. Increasing the drug dose from 2500 to 10,000 IU caused a proportional increase in the AUC for antifactor Xa by almost 1/3. The volume of distribution of anti-factor Xa activity of dalteparin was 40–60 ml/kg. After intravenous administration of 40 and 60 IU/kg, the mean terminal half-life was 2.1 ± 0.3 and 2.3 ± 0.4 hours, respectively. After subcutaneous administration, a significant increase in the terminal half-life (3–5 hours) is observed, which may be due to slower absorption. Dalteparin is primarily excreted by the kidneys, but the biological activity of the fragments of the molecule that are excreted by the kidneys has not been well studied. ≤5% anti-Xa activity is detected in urine. In healthy volunteers, after a single intravenous bolus administration of 30 and 120 antifactor Xa IU/kg, the average plasma clearance of antifactor Xa activity was 24.6±5.4 and 15.6±0.3 hours. Hemodialysis. In patients with chronic renal failure who require hemodialysis, the average half-life of anti-factor Xa activity after a single intravenous dose of 5000 IU dalteparin was 5.7 ± 2.0 hours, which significantly exceeds the values obtained in healthy volunteers, since these patients may experience greater accumulation of the drug. Regardless of the route of administration, dose or duration of treatment, no data were obtained that indicated the organotoxicity of the drug. Also, no mutagenic effect was noted. Animal studies have not revealed embryotoxic, fetotoxic or teratogenic effects or adverse effects on fertility, copulation or peri- and postnatal development.
FRAGMIN 2500IU/0.2ML. No. 10 SYRINGE
Instructions for use:
Registration number
: P N014647/02-100610
Trade name of the drug
: Fragmin®
International Nonproprietary Name (INN)
: dalteparin sodium
Dosage form
: solution for intravenous and subcutaneous administration
Compound
:
Active substance
: dalteparin sodium 2500 IU (anti-Xa)/0.2ml, 5000 IU (anti-Xa)/0.2ml, 10000 IU (anti-Xa)/ml, 7500 IU (anti-Xa)/0, Zml, 10000 IU (anti-Xa)/0.4ml, 12500 IU (anti-Xa)/0.5ml, 15000 IU (anti-Xa)/0.6ml and 18000 IU (anti-Xa)/0.72ml, respectively .
Excipients
: water for injection; if necessary (to adjust the pH) - hydrochloric acid or sodium hydroxide qs (for dosages of 2500 IU (anti-Xa)/0.2 ml, 5000 IU (anti-Xa)/0.2 ml and 10000 IU (anti-Xa)/ml ) and sodium chloride (for dosages of 2500 IU (anti-Xa)/0.2 ml and 10,000 IU (anti-Xa)/ml).
Description
: transparent, colorless or yellowish solution.
Pharmacotherapeutic group
: direct acting anticoagulant
Code ATX
В01АВ04
PHARMACOLOGICAL PROPERTIES
Characteristics
. Dalteparin sodium is a low molecular weight heparin isolated by controlled depolymerization (with nitrous acid) of sodium heparin from the mucous membrane of the small intestine of pigs and subjected to further purification using ion exchange chromatography. The drug consists of sulfated polysaccharide chains with an average molecular weight of 5,000 daltons; while 90% have a molecular weight from 2,000 to 9,000 daltons; degree of sulfation - from 2 to 2.5 per disaccharide.
Pharmacodynamics
Dalteparin sodium inhibits the activity of factor Xa and thrombin through plasma antithrombin. The anticoagulant effect of dalteparin sodium is primarily due to the inhibition of factor Xa; The drug has a slight effect on blood clotting time. Compared to heparin, dalteparin sodium has a weak effect on platelet adhesion and thus has less effect on primary hemostasis.
Pharmacokinetics
. The half-life after intravenous administration of the drug is 2 hours, after subcutaneous administration it is 3-5 hours. Bioavailability after subcutaneous administration is approximately 90%; pharmacokinetic parameters are independent of dose. In patients with uremia, the half-life of the drug is prolonged. Dalteparin sodium is excreted primarily through the kidneys, but the biological activity of fragments excreted by the kidneys has not been well studied. Less than 5% of anti-Xa activity is detected in urine. The clearance of anti-Xa activity of dalteparin from plasma after a single intravenous administration of the drug in the form of a bolus at a dose of 30 and 120 IU (anti-Xa)/kg averaged 24.6±5.4 and 15.6±2.4 ml/h/kg, respectively, and the half-life - 1.47±0.3 and 2.5±0.3 hours.
Special groups
Hemodialysis
- In patients with chronic renal failure receiving hemodialysis treatment, the half-life of anti-Xa activity after a single intravenous administration of dalteparin at a dose of 5000 IU was 5.7 ± 2.0 hours and was significantly higher than in healthy volunteers. Accordingly, a more pronounced accumulation of the drug can be expected in such patients.
Indications for use
- treatment of acute deep vein thrombosis and pulmonary embolism;
- prevention of blood coagulation in the extracorporeal circulatory system during hemodialysis or hemofiltration in patients with acute or chronic renal failure;
- prevention of thrombus formation during surgical interventions;
- prevention of thromboembolic complications in patients with a therapeutic disease in the acute phase and limited mobility (including in conditions requiring bed rest);
- unstable angina and myocardial infarction (without Q wave on ECG),
- long-term treatment (up to 6 months) to prevent recurrence of venous thrombosis and pulmonary thromboembolism in patients with cancer.
Contraindications
- hypersensitivity to dalteparin sodium or to other low molecular weight heparins and/or heparin;
- immune thrombocytopenia (caused by a history of heparin or suspected of its presence);
- bleeding (clinically significant, for example, from the gastrointestinal tract against the background of gastric and/or duodenal ulcers, intracranial bleeding);
- severe disorders of the blood coagulation system;
- septic endocarditis;
- recent injuries or surgical interventions on the central nervous system, organs of vision and/or hearing;
- Due to the increased risk of bleeding, high doses of Fragmin (eg, for the treatment of acute deep vein thrombosis, pulmonary embolism, unstable angina, and non-Q-wave myocardial infarction on the ECG) should not be given to patients who are scheduled for spinal or epidural anesthesia, or other procedures accompanied by lumbar puncture.
With caution
High doses of Fragmin (for example, for the treatment of acute deep vein thrombosis, pulmonary embolism, unstable angina and myocardial infarction without a Q-wave on the ECG) should be prescribed with extreme caution to patients in the early postoperative period. Caution should be exercised when prescribing Fragmin to patients with an increased risk of bleeding; This group includes patients with thrombocytopenia, platelet dysfunction, severe liver or kidney failure, uncontrolled hypertension, hypertensive or diabetic retinopathy.
Application in pediatric practice
There is only limited information about the safety and effectiveness of Fragmin in pediatric practice. When using Fragmin in children, it is necessary to monitor the level of anti-Xa (see section “Method of administration and dosage”).
Pregnancy and lactation
In the experiment, Fragmin does not have a teratogenic or fetotoxic effect. When used in pregnant women, there were no adverse effects on the course of pregnancy, as well as on the health of the fetus and newborn. When using Fragmin during pregnancy, the risk of adverse effects on the fetus is assessed as low. However, since the possibility of adverse effects cannot be completely excluded, Fragmin during pregnancy can be prescribed only if there are clear indications when the expected benefit outweighs the possible risk. It has not been established whether Fragmin is excreted into breast milk.
Method of administration and dosage
Fragmin cannot be administered intramuscularly
!
Treatment of acute deep vein thrombosis and pulmonary embolism
Fragmin is administered subcutaneously 1-2 times a day. In this case, you can immediately begin therapy with indirect anticoagulants (vitamin K antagonists). This combination therapy should be continued until the prothrombin index reaches a therapeutic level (usually this is noted no earlier than after 5 days). Treatment of patients on an outpatient basis can be carried out in the same doses that are recommended for treatment in a hospital setting.
- Administration 1 time per day - a dose of 200 IU/kg body weight is administered subcutaneously. A single daily dose should not exceed 18,000 IU. Monitoring of the anticoagulant activity of the drug may not be carried out.
- Administration 2 times a day - 100 IU/kg body weight subcutaneously 2 times a day. Monitoring of anticoagulant activity may not be necessary, but it should be borne in mind that it may be required when treating special groups of patients (see section "Special Instructions"). The recommended maximum concentration of the drug in blood plasma should be 0.5-1 IU anti-Xa/ml.
Prevention of blood coagulation in the extracorporeal circulation system during hemodialysis or hemofiltration
Fragmin should be administered intravenously (IV), choosing a dosage regimen from those given below.
- Patients with chronic renal failure, or patients without a risk of bleeding.
These patients usually require minor dosage adjustments and therefore there is no need for frequent monitoring of anti-Xa levels in most patients. When administered at recommended doses during hemodialysis, a plasma level of 0.5 -1 IU anti-Xa/ml is usually achieved.
|
- Patients with acute renal failure, or patients at high risk of bleeding
IV jet administration of 5-10 IU/kg body weight, followed by IV drip administration of 4-5 IU/kg/hour. In patients undergoing hemodialysis for acute renal failure, the drug is characterized by a narrower therapeutic index than in patients on chronic hemodialysis (and therefore require adequate monitoring of anti-Xa levels). The recommended maximum plasma level should be 0.2 - 0.4 IU anti-Xa/ml). Prevention of thrombus formation during surgical interventions
Fragmin should be administered subcutaneously. Monitoring of anticoagulant activity is generally not required. When using the drug in recommended doses, maximum plasma concentrations range from 0.1 to 0.4 IU anti-Xa/ml.
- When performing operations in general surgical practice Patients at risk of developing thromboembolic complications - subcutaneously 2500 IU 2 hours before surgery, then after surgery - subcutaneously 2500 IU / day (every morning) for the entire period while the patient is on bed rest (usually 5-7 days).
- Patients with additional risk factors for the development of thromboembolic complications (for example, patients with malignant tumors) - Fragmin should be used for the entire period while the patient is on bed rest (usually 5-7 days or more). 1. When starting therapy the day before surgery: 5000 IU subcutaneously on the evening before surgery, then 5000 IU subcutaneously every evening after surgery. 2. When starting therapy when surgery is too lazy: 2500 IU subcutaneously 2 hours before surgery and 2500 IU subcutaneously 8-12 hours later, but not earlier than 4 hours after the end of the operation. Then, from the next day, 5000 IU is administered s.c. every morning.
Prevention of thromboembolic complications in patients with a therapeutic disease in the acute phase and limited mobility (including in conditions requiring bed rest)
Fragmin should be administered subcutaneously at 5000 IU once a day, usually for 12-14 days or longer (in patients with ongoing mobility restrictions).
Monitoring of anticoagulant activity is generally not required. Unstable angina and myocardial infarction (without Q-wave on ECG)
Monitoring of anticoagulant activity is usually not required, but it should be borne in mind that it may be required when treating special groups of patients (see section "Special instructions"). The recommended maximum concentration of the drug in plasma should be 0.5-1 IU anti-Xa/ml (at the same time, it is advisable to carry out therapy with acetylsalicylic acid in a dose of 75 to 325 mg/day). Fragmin is administered subcutaneously at 120 IU/kg body weight every 12 hours. The maximum dose should not exceed 10,000 IU every 12 hours. Therapy should be continued until the patient's clinical condition becomes stable (usually at least 6 days), or longer (at the discretion of the physician). Then it is recommended to switch to long-term therapy with Fragmin at a constant dose until revascularization (percutaneous interventions or coronary artery bypass grafting). The total duration of therapy should not exceed 45 days. The dose of Fragmin is selected taking into account the gender and body weight of the patient:
- Women weighing less than 80 kg and men weighing less than 70 kg should be administered 5000 IU subcutaneously every 12 hours;
- Women weighing 80 kg or more and men weighing 70 kg or more should administer 7500 IU subcutaneously every 12 hours.
Long-term treatment to prevent recurrence of venous thrombosis in patients with cancer.
- 1 month
Administration 1 time per day - 200 IU/kg body weight subcutaneously. A single daily dose should not exceed 18,000 IU. - 2-6 months
Administration once a day - at a dose of about 150 IU/kg body weight subcutaneously, using syringes with a fixed dose (Table 1).
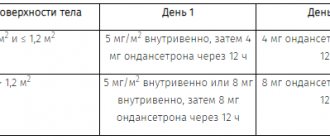
Table 1. Determination of the dose of Fragmin depending on body weight for a treatment period of 2 - 6 months.
| Body weight, kg | Dose of Fragmin, ME |
| <56 | 7500 |
| 57-68 | 10000 |
| 69-82 | 12500 |
| 83-98 | 15000 |
| >99 | 18000 |
Thrombocytopenia
- In case of thrombocytopenia that developed during chemotherapy with a platelet count <50,000/μl, the use of Fragmin should be suspended until the platelet count increases above 50,000/μl. For platelet counts from 50,000/μl to 100,000/μl, the dose of the drug should be reduced by 17% to 33% relative to the initial dose, depending on the patient’s body weight (Table 2). When the platelet count is restored to a level of >100,000/µl, the drug should be prescribed at full dose.
Table 2. Reducing the dose of Fragmin for thrombocytopenia 50,000/μl-100,000/μl.
| Body weight, kg | Planned dose of Fragmin, ME | Reduced dose of Fragmin | Dose reduction,% |
| <56 | 7500 | 5000 | 33 |
| 57-68 | 10000 | 7500 | 25 |
| 69-82 | 12500 | 10000 | 20 |
| 83-98 | 15000 | 12500 | 17 |
| >99 | 18000 | 15000 | 17 |
Renal Insufficiency
- In cases of significant renal insufficiency, defined as creatinine levels greater than 3 times the upper limit of normal, the dose of Fragmin should be adjusted to maintain a therapeutic anti-Xa level of 1 IU/mL (range 0.5-1.5 IU/ml), measured within 4-6 hours after administration of dalteparin. If the anti-Xa level is below or above the therapeutic range, the dose of Fragmin should be increased or decreased accordingly and the anti-Xa measurement should be repeated after administration of 3-4 new doses. Dose adjustments should be made until therapeutic levels of anti-Xa are achieved.
Side effect
The following side effects are observed (on average in 1% of patients): bleeding, hematoma at the injection site, reversible non-immune thrombocytopenia, pain at the injection site, allergic reactions, as well as a transient increase in the activity of “liver” transaminases (AST, ALT). Several cases of immune thrombocytopenia (with or without thrombotic complications), as well as cases of skin necrosis, anaphylactic reactions, spinal or epidural hematoma, peritoneal and intracranial bleeding, some of which were fatal, have been reported.
Overdose
An excessive dose of Fragmin can lead to hemorrhagic complications. In case of overdose, in most cases, bleeding of the skin and mucous membranes, gastrointestinal and urogenital tracts is possible. A decrease in blood pressure, a decrease in hematocrit, or other symptoms may indicate occult bleeding. In case of bleeding, the use of dalteparin sodium should be suspended to assess the severity of bleeding and the risk of thrombosis. The anticoagulant effect of Fragmin can be eliminated by the administration of protamine sulfate, which is an emergency treatment. 1 mg of protamine sulfate partially neutralizes the effect of 100 IU (anti-Xa) dalteparin sodium (and although the induced increase in clotting time is completely neutralized, 25 to 50% of the anti-Xa activity of dalteparin sodium is still retained).
Interaction with other drugs and other forms of interactions
When used simultaneously with drugs that affect hemostasis, such as thrombolytic agents (alteplase, streptokinase, urokinase), indirect anticoagulants, vitamin K antagonists, non-steroidal anti-inflammatory drugs (acetylsalicylic acid, indomethacin, etc.), as well as platelet function inhibitors, anticoagulant effect Fragmina may increase (increases the risk of bleeding).
Compatible with intravenous solutions
. Fragmin is compatible with isotonic sodium chloride solution (9 mg/ml) and isotonic dextrose solution (50 mg/ml).
Special instructions
Fragmin cannot be administered intramuscularly
! When neuraxial anesthesia (epidural/spinal anesthesia) or spinal puncture is performed in patients who are receiving anticoagulant therapy, or who are planned to undergo anticoagulant therapy using low molecular weight heparins or heparinoids to prevent thromboembolic complications, there is an increased risk of developing epidural or spinal hematoma. which in turn can lead to long-term or permanent paralysis. The risk of such complications increases with the use of indwelling epidural catheters for the administration of analgesics or with the simultaneous use of drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs, platelet function inhibitors and other anticoagulants. The risk also increases with trauma and with repeated epidural or lumbar punctures. In such cases, patients should be under constant observation for timely detection of pathological neurological symptoms. If a neurological pathology is detected, emergency intervention (spinal cord decompression) is indicated. There are no clinical data on the use of Fragmin in patients with pulmonary embolism who also had circulatory disorders, arterial hypotension or shock. Particular attention is required for patients who, when treated with Fragmin, experience rapid development of thrombocytopenia, or thrombocytopenia with a platelet count of less than 100,000/μl. In such cases, it is recommended to perform an in vitro test for antiplatelet antibodies in the presence of heparin or low molecular weight heparins. If the result of this in vitro test is positive or equivocal, or no testing has been performed at all, then treatment with Fragmin should be discontinued (see section "Contraindications"). Monitoring the anticoagulant activity of Fragmin is usually not necessary, however, it may be necessary when treating special groups of patients: children, patients with underweight or obesity, pregnant women, and patients with an increased risk of bleeding or recurrent thrombosis. Blood samples for analysis of Fragmin activity should be taken during the period when the maximum concentration of the drug in the blood plasma is reached (3-4 hours after subcutaneous injection). To determine anti-Xa activity, laboratory tests that use a chromogenic substrate are recognized as the method of choice. Activated partial thromboplastin time (aPTT) and thrombin time tests should not be used in this case because these tests are relatively insensitive to the activity of dalteparin sodium. Increasing the dose of Fragmin in order to increase the aPTT may lead to bleeding (see section "Overdose"). The units of action of Fragmin, unfractionated heparin and other low molecular weight heparins are not equivalent, therefore, when replacing one drug with another, a dose adjustment is required. When using multi-dose vials, unused solution must be destroyed 14 days after the first piercing of the stopper with a needle.
Release form
Ampoules
: Solution for intravenous and subcutaneous administration of 10,000 ME (anti-Xa)/ml, 1 ml of the drug in a type I colorless glass ampoule;
2 blister packs of 5 ampoules each are placed in a cardboard box along with instructions for use. Syringes
: Solution for intravenous and subcutaneous administration of 2500 IU (anti-Xa)/0.2 ml, 5000 IU (anti-Xa)/0.2 ml, 7500 IU (anti-Xa)/0.3 ml, 10000 IU (anti-Xa)/0.4 ml, 12,500 IU (anti-Xa)/0.5 ml, 15,000 IU (anti-Xa)/0.6 ml or 18,000 IU (anti-Xa)/0.72 ml placed in a type I glass syringe (Eur.Pharm.) with a stainless steel needle and a protective latex-free cap. 5 syringes in a blister; 2 blisters for volumes of 0.2 ml (for both dosages) or 0.3 ml, or 1 blister for volumes of 0.4; 0.5; 0.6 or 0.72 ml is placed in a cardboard box with instructions for use.
Best before date
: 3 years. Do not use after the expiration date stated on the package.
Storage conditions
Ampoules
: at a temperature not exceeding 30°C
Syringes
: at a temperature not exceeding 25°C Keep out of the reach of children.
Conditions for dispensing from pharmacies
: on prescription.
Ampoule
manufacturer : Pfizer MFG.
Belgium N.V., Belgium Syringes
: Pfizer MFG.
Belgium N.V., Belgium, produced by Vetter Pharma-Fertigung GmbH, Germany Other drugs from the group Drugs affecting blood clotting and thrombus formation, antiplatelet agents, anticoagulants, angioprotectors
Indications for use of the drug Fragmin
- acute deep vein thrombosis, pulmonary embolism;
- prevention of blood coagulation in the extracorporeal circulatory system during long-term hemodialysis or hemofiltration in patients with acute renal failure or chronic renal failure;
- prevention of thrombus formation during surgical interventions;
- prevention of thrombus formation in patients requiring long-term immobilization;
- unstable angina or non- ST (non- Q );
- long-term treatment of symptomatic venous thromboembolism (proximal deep vein thrombosis and/or pulmonary embolism) in order to reduce the frequency of relapses of venous thromboembolism in patients with cancer.
Use of the drug Fragmin
Dalteparin should not be prescribed IM! Compatible with solutions administered intravenously. Dalteparin is compatible with isotonic sodium chloride solution (9 mg/ml) or isotonic glucose solution for infusion (50 mg/ml) in glass or plastic bottles. Acute deep vein thrombosis Fragmin is administered subcutaneously 1 or 2 times a day. At the same time, concomitant therapy with indirect oral anticoagulants (vitamin K antagonists) can be carried out. Combination therapy is continued until the required changes in the prothrombin index are achieved (usually for at least 5 days). The dosage of the drug does not change during outpatient or inpatient treatment. Administration 1 time per day. When administered once a day, Fragmin is prescribed subcutaneously at a dose of 200 IU/kg. The dose for a single administration should not exceed 18,000 IU. Monitoring of the anticoagulant activity of the drug may not be carried out. Administration 2 times a day. When administered 2 times a day, Fragmin is prescribed subcutaneously at 100 IU/kg for each administration. In general, monitoring of the anticoagulant activity of the drug may not be necessary (certain groups of patients are an exception). If necessary, perform a functional analysis of anti-Xa activity; Blood samples are taken for analysis 3–4 hours after drug administration, when the maximum level of anti-Xa activity in the blood serum is reached. The recommended level of anti-Xa activity in blood serum should be in the range of 0.5–1 anti-Xa/ml. Prevention of blood coagulation in the extracorporeal circulatory system during hemodialysis and hemofiltration When preventing blood coagulation in the extracorporeal circulatory system, Fragmin is administered intravenously, choosing the appropriate dosage regimen. Patients with chronic renal failure or patients without risk factors for bleeding. Such patients are usually given only a few doses of Fragmin, so there is no need to monitor anti-Xa levels in most patients. The use of the drug in recommended doses ensures the level of anti-Xa during dialysis in the range of 0.5–1 IU anti-Xa/ml. With a duration of hemodialysis or hemofiltration of a maximum of 4 hours. The drug can be administered to adults at a dose of 30–40 IU/kg body weight as an IV bolus with further fractional administration of 10–15 IU/kg/h or as an IV bolus at a dose of 5000 IU . When the duration of hemodialysis or hemofiltration is 4 hours. For adults, the drug is administered intravenously as a bolus at a dose of 30–40 IU/kg body weight, then dropwise at a rate of 10–15 IU/kg/h. ARF or patients at high risk of bleeding. For acute renal failure in patients with a high risk of bleeding, the drug is administered intravenously as a bolus at a dose of 5–10 IU/kg, then intravenously at a rate of 4–5 IU/kg/h. The number of patients undergoing hemodialysis for acute indications is smaller than the number of patients undergoing hemodialysis for chronic indications and they should be closely monitored for anti-Xa levels. It is recommended to achieve a level of factor Xa suppression activity in blood plasma within the range of 0.2–0.4 IU/ml. Prevention of thromboembolic complications during surgical interventions The drug is administered subcutaneously. Monitoring of anticoagulant activity may not be necessary. If necessary, anti-Xa activity is assessed; blood samples are taken for analysis 3–4 hours after administration of the drug, when the maximum level of anti-Xa activity in the blood serum is reached. Use at the recommended dose typically produces a maximum level of anti-Xa activity in the blood plasma of 0.1–0.4 IU anti-Xa/ml. General surgery Use in cases of high risk of thromboembolism. Adult patients are administered subcutaneously at a dose of 2500 IU 1–2 hours before surgery and then 2500 IU subcutaneously every morning after surgery for the entire period while the patient is on bed rest (usually for 5–7 days or more). If there are additional risk factors for the development of thromboembolic complications (for example, in patients with malignant neoplasms). The drug should be administered for as long as the patient is on bed rest (usually 5–7 days or more). Start of use the day before surgery - administer 5000 IU subcutaneously in the evening before surgery, then 5000 IU every evening. Start of use on the day of surgery - adults are administered 2500 IU subcutaneously 1–2 hours before surgery and 2500 IU 8–12 hours later, but not earlier than 4 hours after the end of the operation. Starting from the next day after surgery, 5000 IU is prescribed subcutaneously every morning. Orthopedic surgeries (for example, joint replacement) The drug can be administered up to 5 weeks after surgery according to one of the following regimens. Beginning of therapy in the evening before surgery - adults are administered 5000 IU subcutaneously in the evening before the day of surgery, after surgery they are administered 5000 IU subcutaneously every evening. Start of therapy on the day of surgery - administer 2500 IU subcutaneously 2 hours before surgery and 2500 IU subcutaneously 8–12 hours later, but not earlier than 4 hours after surgery. Starting the next day after surgery, 5000 IU is administered subcutaneously every morning. Beginning of therapy after surgery - adults are administered 2500 IU subcutaneously 4–8 hours after surgery, but not earlier than 4 hours after its completion. Starting from the next day after surgery, 5000 IU is administered subcutaneously daily. Prevention of thromboembolic complications in patients with limited mobility Adults use 5000 IU Fragmin subcutaneously once a day for 12–14 days or more in patients with prolonged limited mobility. Monitoring the anticoagulant effect of the drug in most cases is not required. Unstable angina and myocardial infarction without elevation of the S-T interval Fragmin is administered subcutaneously at a dose of 120 IU/kg 2 times a day every 12 hours, not exceeding the dose of 10,000 IU/12 hours. In the absence of contraindications, concomitant therapy with acetylsalicylic acid in low doses is recommended doses (75–325 mg/day). Treatment should be continued for at least 6 days or more until the patient's condition is clinically stabilized (at the discretion of the physician). The use of Fragmin in recommended doses should be continued until myocardial revascularization measures are carried out. The total duration of use should not exceed 45 days. The dose of the drug is selected taking into account the gender and body weight of the patient:
- women weighing ≤80 kg and men weighing ≤70 kg are prescribed subcutaneously at a dose of 5000 IU every 12 hours;
- women weighing 80 kg and men weighing 70 kg are prescribed subcutaneously at a dose of 7500 IU every 12 hours.
In most cases, monitoring the anticoagulant effect of the drug is not required, with the exception of certain groups of patients. In the case of such control, studies should be carried out 3-4 hours after subcutaneous injection, when the maximum level of anti-Xa activity in the blood plasma is reached. It is advisable to achieve a level of anti-Xa activity in the range of 0.5–1 IU anti-Xa/ml. Treatment of symptomatic venous thromboembolism to reduce the incidence of venous thromboembolic complications in patients with cancer 1st month. For adults, Fragmin is prescribed at a dose of 200 IU/kg body weight subcutaneously once a day in the first 30 days of treatment. The total daily dose should not exceed 18,000 IU. 2–6 months. For adults, Fragmin is prescribed at a dose of about 150 IU/kg body weight subcutaneously once a day, using a fixed amount of the drug in one syringe according to the data in the table. Doses of the drug during the 2nd–6th month of treatment
Body weight, kg | Dose of Fragmin, IU |
| ≤56 | 7500 |
| 57–68 | 10 000 |
| 69–82 | 12 500 |
| 83–98 | 15 000 |
| ≥99 | 18 000 |
Dose reduction for patients with chemotherapy-induced thrombocytopenia In cases of chemotherapy-induced thrombocytopenia with a platelet count ≤50,000/mm3, use of Fragmin should be interrupted until the platelet count rises to 50,000/mm3. At platelet levels of 50,000–100,000/mm3, the dose of Fragmin should be reduced by 17–33% of the initial dose depending on the patient's body weight, as indicated in the table below. If the platelet count increases to 100,000/mm3, you should switch to the maximum dose of Fragmin. Reducing the dose of Fragmin for thrombocytopenia within the range of 50,000–100,000/mm3
Body weight, kg | Usual dose of Fragmin, IU | Reduced dose of Fragmin, IU | Average dose reduction,% |
| ≤56 | 7500 | 5000 | 33 |
| 57–68 | 10 000 | 7500 | 25 |
| 69–82 | 12 500 | 10 000 | 20 |
| 83–98 | 15 000 | 12 500 | 17 |
| ≥99 | 18 000 | 15 000 | 17 |
Kidney failure. In case of severe renal failure (creatinine level 3 times higher than normal), the dose of Fragmin should be adjusted to maintain a level of anti-Xa activity of about 1 IU/ml (range 0.5–1.5 IU/ml), which should be determined 4–6 hours after injection of the drug. If the level of anti-Xa activity is above or below the therapeutic limit, the dose of Fragmin should be changed according to the amount of the drug in one syringe and the level of anti-Xa activity should be determined after administering new 3-4 doses of the drug. This dose adjustment should be repeated until a therapeutic level of anti-Xa activity is achieved.
Fragmin, 2500 anti-Xa IU/0.2 ml, solution for intravenous and subcutaneous administration, 0.2 ml, 10 pcs.
INSTRUCTIONS for use
APPROVED by the Federal Committee of the Ministry of Health of the Russian Federation on May 30, 2002, pr. No. 1.
Description.
Transparent, colorless or yellowish solution.
Compound.
Active ingredient:
dalteparin sodium 2500 IU (anti-Xa)/0.2 ml, 5000 IU (anti-Xa)/0.2 ml, 10000 IU (anti-Xa)/ml, 7500 IU (anti-Xa)/0 ,3 ml, 10000 IU (anti-Xa)/0.4 ml, 12500 IU (anti-Xa)/0.5 ml, 15000 IU (anti-Xa)/0.6 ml and 18000 IU (anti-Xa) /0.72 ml respectively.
Excipients:
water for injection, sodium chloride, (sodium hydroxide or hydrochloric acid qs - for a solution of 2500 IU (anti-Xa)/0.2 ml and 5000 IU (anti-Xa)/0.2 ml).
Characteristic.
Dalteparin sodium is a low molecular weight heparin isolated by controlled depolymerization (with nitrous acid) of sodium heparin from the mucosa of the small intestine of pigs and subjected to further purification using ion exchange chromatography. The drug consists of sulfated polysaccharide chains with an average molecular weight of 5000 daltons; while 90% have a molecular weight from 2000 to 9000 daltons; degree of sulfation - from 2 to 2.5 per disaccharide.
Pharmacological properties.
Pharmacodynamics.
Dalteparin sodium inhibits the activity of factor Xa and thrombin through plasma antithrombin. The anticoagulant effect of dalteparin sodium is primarily due to the inhibition of factor Xa; The drug has a slight effect on blood clotting time. Compared with heparin, dalteparin sodium has a weak effect on platelet adhesion and, thus, has less effect on primary hemostasis.
Pharmacokinetics.
T1/2 after intravenous administration of the drug - 2 hours, after subcutaneous administration - 3-5 hours. Bioavailability after subcutaneous administration is approximately 90%; pharmacokinetic parameters are independent of dose. In patients with uremia, T1/2 of the drug increases. Dalteparin sodium is excreted primarily through the kidneys.
Indications for use.
Treatment of acute deep vein thrombosis and pulmonary embolism.
Prevention of blood coagulation in the extracorporeal circulatory system during hemodialysis or hemofiltration in patients with acute or chronic renal failure.
Prevention of thrombus formation during surgical interventions.
Unstable angina and myocardial infarction (without Q wave on ECG).
Contraindications.
Hypersensitivity to dalteparin sodium or to other low molecular weight heparins and/or heparin.
Immune thrombocytopenia (history of heparin-induced or suspected presence).
Bleeding (clinically significant, for example, from the gastrointestinal tract against the background of gastric and/or duodenal ulcers, intracranial bleeding).
Severe disorders of the blood coagulation system.
Septic endocarditis.
Recent injuries or surgical interventions on the central nervous system, visual and/or hearing organs.
Due to the increased risk of bleeding, high doses of Fragmin (eg, for the treatment of acute deep vein thrombosis, pulmonary embolism, unstable angina, and non-Q-wave myocardial infarction on the ECG) should not be given to patients who are scheduled for spinal or epidural anesthesia, or other procedures accompanied by lumbar puncture.
Precautionary measures.
High doses of Fragmin (for example, for the treatment of acute deep vein thrombosis, pulmonary embolism, unstable angina and myocardial infarction without a Q-wave on the ECG) should be prescribed with extreme caution to patients in the early postoperative period. Caution should be exercised when prescribing Fragmin to patients with an increased risk of bleeding; This group includes patients with thrombocytopenia, platelet dysfunction, severe liver or kidney failure, uncontrolled hypertension, hypertensive or diabetic retinopathy.
Method of administration and dose.
Fragmin cannot be administered intramuscularly.
Treatment of acute deep vein thrombosis and pulmonary embolism
Fragmin is administered subcutaneously 1–2 times a day. In this case, you can immediately begin therapy with indirect anticoagulants (vitamin K antagonists). This combination therapy should be continued until the prothrombin index reaches a therapeutic level (usually this is noted no earlier than after 5 days). Treatment of patients on an outpatient basis can be carried out in the same doses that are recommended for treatment in a hospital setting.
Administration 1 time per day - a dose of 200 IU/kg body weight is administered subcutaneously. A single daily dose should not exceed 18,000 IU. Monitoring the anticoagulant activity of the drug
may not be carried out.
Administration 2 times a day - 100 IU/kg body weight subcutaneously 2 times a day. Monitoring of anticoagulant activity may not be necessary, but it should be borne in mind that it may be required when treating special groups of patients (see section "Special Instructions"). The recommended plasma Cmax should be 0.5–1 IU anti-Xa/ml.
Prevention of blood coagulation in the extracorporeal circulation system during hemodialysis or hemofiltration
Fragmin should be administered intravenously, choosing a dosage regimen from those given below.
Patients with chronic renal failure, or patients without risk of bleeding
.
These patients usually require minor dosage adjustments and therefore there is no need for frequent monitoring of anti-Xa levels in most patients. When administered at recommended doses during hemodialysis, plasma levels of 0.5–1 IU anti-Xa/ml are typically achieved.
When the duration of hemodialysis or hemofiltration is no more than 4 hours
— IV bolus at 30–40 IU/kg body weight, followed by IV drip administration at 10–15 IU/kg/h, or a single IV bolus at a dose of 5000 IU.
If the duration of hemodialysis or hemofiltration is more than 4 hours
- intravenous injection of 30–40 IU/kg body weight, followed by intravenous drip administration of 10–15 IU/kg/hour.
Patients with acute renal failure, or patients at high risk of bleeding
.
IV jet administration of 5–10 IU/kg body weight followed by IV drip administration of 4–5 IU/kg/hour. In patients undergoing hemodialysis for acute renal failure, the drug is characterized by a narrower therapeutic index than in patients on chronic hemodialysis (and therefore they require adequate monitoring of anti-Xa levels). The recommended maximum plasma level should be 0.2–0.4 IU anti-Xa/ml.
Prevention of thrombus formation during surgical interventions
Fragmin should be administered subcutaneously. Monitoring of anticoagulant activity is generally not required. When using the drug in recommended doses, maximum plasma concentrations range from 0.1 to 0.4 IU anti-Xa/ml.
When performing operations in general surgical practice
Patients at risk of developing thromboembolic complications
- SC 2500 IU 2 hours before surgery, then after surgery - SC 2500 IU / day (every morning) for the entire period while the patient is on bed rest (usually 5-7 days).
Patients with additional risk factors for thromboembolic complications (eg, patients with malignancies)
— Fragmin should be used for the entire period while the patient is on bed rest (usually 5–7 days or more).
1. When starting therapy the day before surgery: 5000 IU subcutaneously on the evening before surgery, then 5000 IU subcutaneously every evening after surgery.
2. When starting therapy on the day of surgery: 2500 IU subcutaneously 2 hours before surgery and 2500 IU subcutaneously 8–12 hours later, but not earlier than 4 hours after the end of the operation. Then, from the next day, 5000 IU is administered s.c. every morning.
When performing orthopedic operations (for example, during hip replacement operations).
Fragmin should be administered for up to 5 weeks after surgery using one of the dosing regimens listed below.
1. When starting therapy the evening before surgery: 5000 IU subcutaneously the evening before surgery, then 5000 IU subcutaneously every evening after surgery.
2. When starting therapy on the day of surgery: 2500 IU subcutaneously 2 hours before surgery and 2500 IU subcutaneously 8–12 hours later, but not earlier than 4 hours after the end of the operation. Then from the next day every morning - 5000 IU subcutaneously.
3. When starting therapy after surgery: 2500 IU subcutaneously 4–8 hours after surgery, but not earlier than 4 hours after the end of surgery. Then from the next day, 5000 IU subcutaneously per day.
Unstable angina and myocardial infarction (without Q-wave on ECG)
Monitoring of anticoagulant activity is generally not required, but it should be borne in mind that it may be required when treating special groups of patients (see section "Special Instructions"). The recommended Cmax in plasma should be 0.5–1 IU anti-Xa/ml (at the same time, it is advisable to carry out therapy with acetylsalicylic acid in a dose of 75 to 325 mg/day). Fragmin is administered subcutaneously at 120 IU/kg body weight every 12 hours. The maximum dose should not exceed 10,000 IU every 12 hours. Therapy should be continued until the patient’s clinical condition becomes stable (usually at least 6 days), or longer (at the discretion of the doctor). Then it is recommended to switch to long-term therapy with Fragmin at a constant dose until revascularization (percutaneous interventions or coronary artery bypass grafting). The total duration of therapy should not exceed 45 days. The dose of Fragmin is selected taking into account the gender and body weight of the patient:
- women weighing less than 80 kg and men weighing less than 70 kg should be administered 5000 IU subcutaneously every 12 hours;
- women weighing 80 kg or more and men weighing 70 kg or more should be administered 7500 IU subcutaneously every 12 hours.
Side effect.
The following side effects are observed (on average in 1% of patients): bleeding, hematoma at the injection site, reversible non-immune thrombocytopenia, pain at the injection site, allergic reactions, as well as a transient increase in the activity of “liver” transaminases (AST, ALT). Several cases of immune thrombocytopenia (with or without thrombotic complications), as well as cases of skin necrosis, anaphylactic reactions, and the development of spinal or epidural hematoma, have been reported.
Overdose.
The anticoagulant effect of Fragmin can be eliminated by the administration of protamine sulfate, which is an emergency treatment. 1 mg of protamine partially neutralizes the effect of 100 IU (anti-Xa) dalteparin sodium (and although there is complete neutralization of the induced increase in clotting time, 25 to 50% of the anti-Xa activity of dalteparin sodium is still retained).
Interaction with other drugs and other forms of interactions.
When used simultaneously with drugs that affect hemostasis, such as thrombolytic agents, other anticoagulants, NSAIDs, and platelet function inhibitors, the anticoagulant effect of Fragmin may be enhanced.
Weakening of the effect when used together with antihistamines, cardiac glycosides, tetracyclines, ascorbic acid.
Compatible with solutions for intravenous administration.
Fragmin is compatible with isotonic sodium chloride solution (9 mg/ml) and isotonic dextrose solution (50 mg/ml).
Special instructions.
Fragmin cannot be administered intramuscularly.
When neuraxial anesthesia (epidural/spinal anesthesia) or spinal puncture is performed in patients who are receiving anticoagulant therapy, or who are planned to undergo anticoagulant therapy using low molecular weight heparins or heparinoids to prevent thromboembolic complications, there is an increased risk of developing epidural or spinal hematoma. which in turn can lead to long-term or permanent paralysis. The risk of such complications increases with the use of indwelling epidural catheters for the administration of analgesics or with the simultaneous use of drugs that affect hemostasis, such as NSAIDs, platelet function inhibitors and other anticoagulants. The risk also increases with trauma and with repeated epidural or lumbar punctures. In such cases, patients should be under constant observation for timely detection of pathological neurological symptoms. If a neurological pathology is detected, emergency intervention (spinal cord decompression) is indicated.
There are no clinical data on the use of Fragmin in patients with pulmonary embolism who also had circulatory disorders, arterial hypotension or shock.
Particular attention is required for patients who, when treated with Fragmin, experience rapid development of thrombocytopenia, or thrombocytopenia with a platelet count of less than 100,000/μl. In such cases, it is recommended to perform an in vitro test for antiplatelet antibodies in the presence of heparin or low molecular weight heparins. If the result of this in vitro test is positive or equivocal, or no testing has been performed at all, then treatment with Fragmin should be discontinued (see section "Contraindications").
Monitoring the anticoagulant activity of Fragmin is usually not necessary, however, it may be necessary when treating special groups of patients: children, patients with underweight or obesity, pregnant women, and patients with an increased risk of bleeding or recurrent thrombosis.
Blood samples for analysis of Fragmin activity should be taken during the period when Cmax in plasma is reached (3-4 hours after subcutaneous injection).
To determine anti-Xa activity, laboratory tests that use a chromogenic substrate are recognized as the method of choice. Activated partial thromboplastin time (aPTT) and thrombin time tests should not be used in this case because these tests are relatively insensitive to the activity of dalteparin sodium. Increasing the dose of Fragmin in order to increase the aPTT may lead to bleeding (see section "Overdose").
The units of action of Fragmin, unfractionated heparin and other low molecular weight heparins are not equivalent, therefore, when replacing one drug with another, a dose adjustment is required.
When using multi-dose vials, unused solution must be destroyed 14 days after the first piercing of the stopper with a needle.
Application in pediatric practice.
There is only limited information about the safety and effectiveness of Fragmin in pediatric practice. When using Fragmin in children, it is necessary to monitor the level of anti-Xa (see section “Method of administration and dosage”).
Pregnancy and breastfeeding.
In the experiment, Fragmin does not have a teratogenic or fetotoxic effect. When used in pregnant women, no adverse effects on the course of pregnancy were detected. as well as the health of the fetus and newborn. When using Fragmin during pregnancy, the risk of adverse effects on the fetus is assessed as low. However, since the possibility of adverse effects cannot be completely excluded, Fragmin during pregnancy can be prescribed only if there are clear indications when the expected benefit outweighs the possible risk. It has not been established whether Fragmin is excreted into breast milk.
Release form.
Solution for injection 10,000 ME (anti-Xa)/ml, 10 ampoules of 1 ml with instructions for use in a cardboard box.
Solution for injection 2500 IU (anti-Xa)/0.2 ml, 10 disposable syringes of 0.2 ml each with instructions for use in a cardboard box.
Solution for injection 5000 ME (anti-Xa)/0.2 ml, 10 disposable syringes of 0.2 ml each with instructions for use in a cardboard box.
Solution for injection 7500 ME (anti-Xa)/0.3 ml, 10 disposable syringes of 0.3 ml with instructions for use in a cardboard box.
Injection solution 10,000 ME (anti-Xa)/0.4 ml, 5 disposable syringes of 0.4 ml each with instructions for use in a cardboard box.
Solution for injection 12500 ME (anti-Xa)/0.5 ml, 5 disposable syringes of 0.5 ml with instructions for use in a cardboard box.
Solution for injection 15000 ME (anti-Xa)/0.6 ml, 5 disposable syringes of 0.6 ml with instructions for use in a cardboard box.
Solution for injection 18000 ME (anti-Xa)/0.72 ml, 5 disposable syringes of 0.72 ml with instructions for use in a cardboard box.
Storage conditions.
Store out of the reach of children, at a temperature not exceeding 30 °C.
Best before date.
3 years.
Conditions for dispensing from pharmacies.
By doctor's prescription.
Manufacturer.
Disposable syringes: Pharmacia N.V./S.A., Belgium, manufactured by Vetter Pharma-Fertigung GmbH, Germany.
Ampoules: Pharmacy and Upjohn N.V./S.A., Belgium.
Contraindications to the use of the drug Fragmin
- reliable or probable history data on the presence of immune heparin-induced thrombocytopenia;
- active clinically significant bleeding (peptic ulcer of the stomach or duodenum, clinical manifestations of active ulcer bleeding or cerebral hemorrhage);
- severe blood clotting disorders;
- septic endocarditis;
- injuries to the central nervous system, organs of vision, hearing, as well as surgical interventions on these organs;
- hypersensitivity to dalteparin and other heparins. In addition, high doses of Fragmin (used in the treatment of acute deep vein thrombosis, pulmonary thromboembolism or unstable angina) should not be used in patients who have received spinal or epidural anesthesia or spinal puncture, as there is a high risk of bleeding.
Side effects of the drug Fragmin
During clinical studies, the following side effects occurred with a frequency of 1%:
- from the blood and lymphatic systems - reversible thrombocytopenia of non-immune origin (type I);
- hepatobiliary disorders - transient increase in the activity of liver transaminases (ALAT, AST);
- general disorders and changes at the injection site - bleeding, hematoma formation at the injection site, allergic reactions, pain at the injection site.
The following violations have been reported post-marketing:
- on the part of the blood and lymphatic system - the appearance of immune heparin-induced thrombocytopenia (type II) in combination with or without thrombotic complications;
- from the skin - skin necrosis, alopecia;
- from the immune system - anaphylactic reactions;
- injuries, poisoning and complications of procedures - spinal or epidural hematomas, retroperitoneal and intracranial hemorrhages, which can sometimes be fatal.
Special instructions for the use of the drug Fragmin
Epidural or spinal anesthesia. When conducting anticoagulant therapy to prevent thromboembolic complications (anticoagulants of the group of low molecular weight heparins or heparinoids) in patients who have undergone neuraxial anesthesia (epidural or spinal) or spinal puncture, there is a risk of developing an epidural or spinal hematoma, which can cause prolonged or irreversible paralysis. The risk of developing this complication increases when using an indwelling epidural catheter for prolonged anesthesia or while using drugs that affect hemostasis (NSAIDs, platelet aggregation inhibitors or other anticoagulants). The risk also increases with traumatic or repeated epidural or spinal puncture. Such patients should be monitored frequently for neurological complications. If neurological symptoms are detected, therapy with spinal cord decompression should be immediately performed. Risk of bleeding. The drug should be used with caution in patients with an increased risk of bleeding, namely in patients with thrombocytopenia, impaired platelet function, severe renal or hepatic impairment, uncontrolled hypertension (arterial hypertension) and in patients with hypertensive or diabetic retinopathy. Caution should also be exercised when treating Fragmin in high doses (necessary for the treatment of deep vein thrombosis, pulmonary embolism and unstable angina or myocardial infarction without ST ) in patients in the early postoperative period. Thrombocytopenia. Particular attention is required if thrombocytopenia develops rapidly or if there is a significant decrease in platelet levels (≤100,000/mm3) during treatment with Fragmin. In such cases, an in vitro to detect antiplatelet antibodies in the presence of heparin or low molecular weight heparin. If the results of such a test are positive or equivocal, or the test was not performed, use of Fragmin should be discontinued. Monitoring of anti-Xa activity. Monitoring the anticoagulant effect of Fragmin in most cases is not necessary, but it should be carried out in certain groups of patients: children, patients with renal failure, patients with insufficient or overweight, pregnant women, patients with an increased risk of bleeding or recurrent thrombosis. For laboratory monitoring of treatment with Fragmin, tests should be used to determine anti-Xa activity using a chromogenic substrate. It is not practical to determine activated partial prothrombin time or thrombin time, since these tests are insensitive to the activity of dalteparin. Increasing the dose of dalteparin to increase the activated partial prothrombin time may result in bleeding. Interchangeability with other anticoagulants. Fragmin is not interchangeable (in the same units) with unfractionated heparin, other low molecular weight heparins or synthetic polysaccharides. Each of these drugs differs in raw materials, manufacturing processes, physicochemical, biological and clinical properties, which determines the difference in their biochemical properties, dosing, clinical effectiveness and safety. Each of these drugs is unique and has its own instructions for use. Application in pediatrics. Given the insufficient experience with the use of the drug in children, the level of anti-Xa activity should always be determined in this category of patients. During pregnancy and breastfeeding. When using Fragmin during pregnancy, the likelihood of harm to the fetus is low. However, since the possibility of harmful effects on the fetus cannot be completely excluded, the drug should be prescribed during pregnancy only if absolutely necessary. Limited data are available on the excretion of dalteparin into breast milk. One study of 15 breastfeeding mothers who received prophylactic doses of dalteparin found negligible levels of anti-Xa activity in breast milk (breast milk to plasma concentration ratio ≤0.025–0.224). Although the oral absorption of low molecular weight heparins is negligible, limited clinical data do not allow conclusions to be drawn regarding the effect of this small level of anticoagulant activity in the nursing infant. The effect of dalteparin on the ability to drive vehicles and operate machinery has not been studied .
Instructions for use FRAGMIN
Fragmin should not be administered intramuscularly. Due to the risk of hematoma, IM administration of other drugs should be avoided if the dose of dalteparin sodium in 24 hours exceeds 5000 IU.
Risk of bleeding
Fragmin should be used with caution in patients with thrombocytopenia and impaired platelet function, severe hepatic and renal failure, uncontrolled hypertension, hypertensive or diabetic retinopathy and known hypersensitivity to heparin and/or low molecular weight heparins. Caution should also be exercised when using high doses of dalteparin (eg, doses required for the treatment of acute deep vein thrombosis, pulmonary embolism and acute coronary artery disease) in recently operated patients, as well as in patients with other conditions with a possible increased risk of bleeding.
If a patient suffering from acute ischemic disease (unstable angina and non-Q wave myocardial infarction) develops myocardial infarction, thrombolytic therapy may be required. This does not mean that dalteparin therapy should be discontinued, but it does mean that there is an increased risk of bleeding.
Epidural and spinal anesthesia
When performing neuraxial anesthesia (epidural or spinal anesthesia) or spinal puncture while using low molecular weight heparins in patients (including patients planned to use anticoagulants), the risk of epidural or spinal hematoma increases, which can cause neurological complications of varying severity, including long-term or persistent paralysis. The risk of these complications increases with the use of indwelling epidural catheters after surgery or with concomitant use of medications that affect hemostasis, such as NSAIDs, platelet inhibitors, or other anticoagulants. The risk also increases with traumatic or repeated epidural or lumbar punctures. Patients should be monitored frequently for the development of signs and symptoms of neurological impairment when anticoagulant therapy is administered in conjunction with epidural/spinal anesthesia.
In order to reduce the risk of bleeding during spinal or epidural anesthesia while using Fragmin, it is better to insert or remove a catheter at the moment when the anticoagulant effect of the drug is least pronounced. Insertion or removal of catheter should be delayed 10-12 hours after the last dose of Fragmin prescribed for thrombosis prophylaxis while patients receiving higher therapeutic doses of dalteparin (such as 100-120 IU/kg every 12 hours or 200 IU /kg 1 time/day), the minimum interval should be 24 hours. Performing epidural/spinal anesthesia or spinal puncture during the treatment of deep vein thrombosis with anticoagulants is contraindicated. After removal of the catheter, the next dose of Fragmin should be administered no earlier than 4 hours later.
When prescribing an anticoagulant to a patient prior to epidural/spinal anesthesia or spinal tap, extreme caution and close and frequent monitoring should be performed for signs or symptoms of nervous system involvement, such as back pain, sensory or motor disturbances (numbness or weakness of the lower extremities), and bowel or bladder dysfunction. Nursing staff should be able to recognize symptoms of nervous system damage at an early stage. Patients should be advised to report the occurrence of neurological symptoms to their physician. If signs or symptoms of a possible intraspinal hematoma appear, immediate diagnostic and therapeutic procedures, including spinal cord decompression, are necessary.
Artificial heart valves
Appropriate studies have not been conducted to evaluate the safety and effectiveness of Fragmin as a prophylaxis for valve thrombosis in patients with artificial heart valves. Prophylactic doses of Fragmin are not sufficient to prevent valve thrombosis in patients with artificial heart valves. The use of Fragmin cannot be recommended for this purpose.
Thrombocytopenia
Due to the risk of thrombocytopenia, it is recommended to determine the platelet count before starting treatment with dalteparin and regularly during treatment. Particular caution is required in patients with rapidly developing thrombocytopenia or severe thrombocytopenia (<100,000/mcL) associated with positive or unknown in vitro platelet antibody test results in the presence of dalteparin or other low molecular weight heparins and/or unfractionated heparins.
If thrombocytopenia occurs, treatment should be discontinued. Subsequently, treatment should be initiated with fractionated heparin, which did not cause aggregation of the patient's platelets in an in vitro aggregation study. In the future, the platelet count should be determined at least 2 times a week, especially during the first 3 weeks.
It is important to note that heparin-induced thrombocytopenia type II should not be confused with early postoperative thrombocytopenia.
Monitoring Anti-Xa Levels
Monitoring for the anticoagulant effect of dalteparin is generally not required but may be considered in special patient populations, such as children, patients with renal impairment, patients with very low body weight or morbid obesity, pregnant women, or patients at increased risk of bleeding or recurrence. thrombosis
The time required for clot formation, defined as aPTT, is the only indicator that is moderately prolonged by dalteparin treatment and should not be used because it is relatively insensitive to the effects of dalteparin. Therefore, increasing the dose in order to prolong the aPTT may lead to drug overdose and bleeding. For laboratory monitoring of the risk of bleeding, it is recommended to use functional methods for determining the level of anti-Xa.
Hyperkalemia, renal failure
Heparin may suppress adrenal aldosterone secretion and lead to hyperkalemia, especially in patients with diabetes mellitus, chronic renal failure, pre-existing metabolic acidosis, elevated plasma potassium levels, or in patients taking potassium-sparing drugs. The risk of hyperkalemia increases with increasing duration of therapy, but is usually reversible. In patients at risk, plasma potassium levels should be measured before starting heparin therapy and monitored regularly thereafter, especially if treatment lasts more than 7 days. In patients receiving dalteparin and undergoing chronic hemodialysis, dose adjustment and, as a result, monitoring of anti-Xa levels in the blood is required less frequently. In patients undergoing emergency hemodialysis, the pharmacokinetics of dalteparin may be more unstable and their therapeutic index may be narrowed. More careful monitoring of anti-Xa levels in these patients is necessary.
For long-term treatment of acute ischemic heart disease, for example, before revascularization, the need for dose reduction should be assessed in case of reduced renal function (serum creatinine level >150 µmol/l).
Interchangeability with other anticoagulants
The biological activity of various low molecular weight heparins, unfractionated heparin or synthetic polysaccharides cannot be determined using a test that simply compares doses of different drugs. Due to the fact that different low molecular weight heparins have different properties, their doses require adjustment. Thus, using one anticoagulant drug instead of another should be done with extreme caution and guided by the approved instructions for use of each specific drug.
Use in elderly patients
In elderly patients (especially patients aged 80 years and older), the risk of bleeding may be increased when using therapeutic doses of the drug. The clinical condition of such patients should be carefully monitored.
Use in pediatrics
Clinical experience in treating children is limited. When using dalteparin in children, monitoring of anti-Xa levels is necessary.
Preclinical safety data
The degree of acute toxicity is significantly lower with dalteparin sodium compared to heparin. In toxicology studies, local bleeding at the injection site was the only significant reaction regularly reported following high-dose subcutaneous administration of the drug. The frequency and severity of this phenomenon were dose-related. There was no cumulative effect on injection site bleeding.
Hemorrhagic reactions led to dose-dependent changes in the anticoagulant effect, which was assessed by measuring APTT and anti-Xa activity.
The osteoporotic effect of dalteparin sodium does not exceed that of heparin.
The study results did not reveal organotoxicity, regardless of the method of drug administration, dose and duration of therapy. No mutagenic effect was detected. No embryotoxic or teratogenic effects were observed; no effects on fertility or peri- or postnatal development were noted.
Impact on the ability to drive vehicles and operate machinery
Fragmin does not affect the ability to drive vehicles or operate mechanical equipment.