- Causes of the disease
- Bell's Palsy Symptoms
- Classification
- At-risk groups
- Diagnostics
- Treatment of Bell's palsy
- Complications
- Rehabilitation and prognosis
Bell's palsy is a pathology that develops as a result of inflammation of the facial nerve, which is responsible for the facial muscles of one half of the face. In this case, sensitivity decreases, muscle weakness develops, and facial movements are difficult. Facial asymmetry becomes pronounced, and problems with the organs of vision begin. The occurrence of Bell's palsy can be associated with prolonged hypothermia, viruses, neoplasms or inflammatory processes. The disease requires treatment and rehabilitation, otherwise persistent asymmetry and complete paralysis may develop.
General information
Facial nerve neuropathy (synonym: facial nerve neuritis, Bell's palsy) is paralysis/paresis of the facial nerve, accompanied by sensory, motor and autonomic disturbances in the area of innervation of the facial muscles and facial asymmetry.
Facial nerve neuropathy (FN) is one of the most common and pressing problems in neurology. Specific lesions of the facial nerve, according to various authors, range from 9.3 to 12.8% of all diseases of the peripheral nervous system. Facial nerve neuritis code according to ICD-10: G51.0 - Bell's palsy. In modern terminology, the term “Bell's palsy” is usually used only to refer to damage to the facial nerve of unknown etiology (idiopathic origin), while neuropathy of the facial nerve is a broader concept that includes a whole variety of forms.
First of all, it should be noted that NLN always develops only when the nerve fiber is damaged from the motor nucleus of the facial nerve to its exit from the stylomastoid foramen (peripheral paresis) and always on the same side, in contrast to central paresis, which occurs mainly during a stroke and is often combined with paresis of the limbs developing on the side opposite to the lesion (Fig. below).
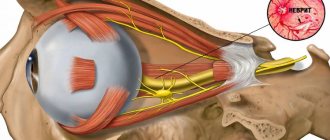
The facial nerve (FN) refers primarily to the motor nerves that provide facial expressions, the processes of blinking, chewing, swallowing, and frowning. However, the trunk of the facial nerve also contains components of the intermediate nerve - parasympathetic (secretory) and sensory (taste) fibers innervating the salivary glands, as well as the taste sensitivity of the tongue.
The relatively high incidence of damage to the facial nerve is largely due to its inherent anatomical and topographical features - the nerve has a complex and long course in the narrow bony canal of the temporal bone. The most vulnerable segment of the FN (in which it is pinched/compressed) is the segment located in a narrow convoluted canal where, in cases of edema development due to various reasons (for example, inflammation), it is compressed.
Among different localizations of damage to the peripheral part of the FN, Bell's palsy is the most common pathology (16-25 cases / 100,000 population) and is caused by the development of edema and its subsequent compression in the bone canal ( tunnel syndrome ). The high vulnerability of the FN in the fallopian canal is explained by its prevalence in the cross section of the canal, where it occupies 40%-70% of the total area. Moreover, despite the fact that the canal narrows in some places, the thickness of the nerve trunk itself remains unchanged.
In the vast majority of cases, peripheral paresis of the facial nerve is manifested by unilateral damage to the facial nerve. The right/left facial side is affected with equal frequency. Bilateral neuropathy of the FN accounts for only 6.2% of all its lesions. The average age of onset is about 40 years, but can occur at any age. The lowest incidence rate is observed in children under 10 years of age, increases in persons in the age group 10–29 years, stable rates are typical for persons 30–69 years of age, and reaches maximum rates in the population of patients after 70 years of age.
The disease is characterized by a high frequency of complications (7–18% of cases); recurrent FN neuropathies are observed in 24.5% of cases. Recurrent neuropathies, compared to primary ones, are more severe, more difficult to treat, and extremely rarely result in complete recovery. Neuropathy of the facial nerve, as many patients who visit a special forum write, is an extremely psychotraumatic situation for patients and has an extremely negative impact on the psycho-emotional sphere and physical condition of patients, up to the development of neurosis. FN palsy is a common cause of long-term disability and significantly reduces quality of life.
Pathogenesis
The triggering factor for FLN is irritation of the vessels of the craniocervical region, which contributes to the development of vasospasm of the vertebral and branches of the external carotid artery, which leads to primary ischemia of the FLN root. Increasing disturbances of microcirculation in the structures of the FN lead to anoxic swelling of the nerve . This, in turn, leads to compression (squeezing) of the nervous tissue in the facial (fallopian) canal of the temporal bone, disruption of neuromuscular conduction caused by blockade of the process of release of acetylcholine and a disorder in the interaction of acetylcholine with receptors located on the postsynaptic membrane. As disorders increase in the nervous tissue, secondary ischemia of the FN develops.
Alternative medicine
Although there is no scientific evidence to support the use of alternative medicine for people with Bell's palsy, some people with the condition may benefit from the following:
- Acupuncture. Placing thin needles at a specific point on your skin helps stimulate the nerves and muscles, which may provide some relief.
- Biofeedback training. Teaching you to use your thoughts to control your body can help you gain better control of your facial muscles.
Classification
There are primary lesions of the FN, caused by hypothermia, and secondary, as a complication of other diseases.
Based on etiology, they are distinguished:
- Bell's palsy (idiopathic neuropathy).
- Otogenic neuritis (with inflammation of the middle ear/mastoid process of the temporal bone).
- Infectious neuritis ( influenza , herpes , mumps , polio , etc.).
- Traumatic neuritis (damage to the facial nerve).
- Ischemic (in cases of impaired blood supply to the nerve).
Affected Populations
Bell's palsy is a fairly common condition, affecting men and women in equal numbers. It is estimated that 25-35 out of 100,000 people suffer from Bell's palsy. Approximately 40,000 people are diagnosed with the disease each year.
Older people are more likely to develop Bell's palsy than children, but the disorder can affect people of any age. However, pregnant women or people with diabetes or upper respiratory disease are affected more often than the general population.
Causes of neuritis of the facial nerve
With the peripheral nature of the FN lesion, it is quite difficult to establish the causes of the disease in most cases. It is generally accepted that the causes of FN neuropathy are polyetiological (ischemic, otogenic, idiopathic, traumatic, infectious and other origins). As already indicated, Bell's palsy develops as a result of compression of the nerve in the narrow convoluted canal of the temporal bone, which occurs for various reasons (inflammation, hereditary predisposition in the form of congenital narrowness of the facial nerve canal).
Provoking factors for FN neuropathy include hypothermia, infections, nerve compression by a tumor ( neurinoma ), trauma to the bones of the base of the skull/face with mechanical damage/rupture of nerve fibers, and poisoning. Also, neuropathy can develop as a complication of otitis , mumps , mesotympanitis , neurotropic viral infection ( poliomyelitis , herpes ), inflammatory processes in the brain.
Diagnostics
This disease has a clear clinical picture, so already at the examination stage the doctor can make a preliminary diagnosis, which will only need to be differentiated from other similar ailments and determine the cause.
So, a neurological examination includes:
- determining the degree of damage to the facial muscles (puffing out the cheeks, closing the eyes, frowning);
- determining the presence of a “sail sign” (the doctor asks you to take a deep breath and exhale; when you exhale, a kind of puffing of the cheek is noted on the affected side);
- To differentiate the disease from the symptoms of a stroke, an examination of the face is carried out (for example, with a stroke, weakness of the lower part of the face is noted, while with Bell's palsy, weakness is observed in the entire affected part).
In addition to a neurological examination, the doctor will prescribe a comprehensive diagnosis of the body, which includes:
- radiography;
- Magnetic resonance imaging;
- rheoencephalography;
- CT scan;
- Dopplerography of cerebral vessels;
- collection of cerebrospinal fluid to determine pleocytosis.
Symptoms
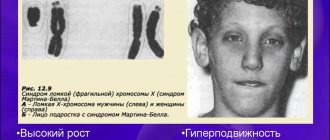
Symptoms of facial neuritis are determined by the level of its damage. Let us consider only the symptoms of compression-ischemic damage to the FN (Bell's palsy). Most often, compression-ischemic neuropathy manifests itself as acutely developed paresis/paralysis of facial muscles in the form of:
- Marked smoothness of all skin folds of the face on the affected side, the eyelid and corner of the mouth are drooping.
- Bloating of the cheek when exhaling/speaking when pronouncing consonants (sail sign).
- “Hare eye” - when you close your eyes, the eye does not close on the affected side, while the eyeball turns slightly outward/upward.
- Inability to raise an eyebrow, close an eye, wrinkle a forehead, whistle, the mouth slit is pulled to the healthy side when grinning.
- Getting solid food between the gum and cheek when chewing and pouring liquid over the edge of the mouth on the affected side.
- Problems with diction (not always).
- Pain behind the ear.
Facial asymmetry is extremely specific and difficult to miss (photo below). In the acute stage of the disease, the patient’s face is asymmetrical and at rest, while the “healthy” side of the face pulls on the paretic muscles, thereby causing additional discomfort.
Facial paralysis usually begins suddenly. At the onset of the disease, some patients develop moderate/mild pain and paresthesia in the mastoid/ear area 1-2 days before the onset of movement disorders or simultaneously.
Preparing for your appointment
You'll probably start by seeing your family doctor. However, in some cases, when you call to make an appointment, you may be able to see a neurologist immediately.
It's nice to prepare for the meeting. Here's some information to help you prepare.
What can you do
- Write down any symptoms you experience. Be sure to include anything that may seem unrelated to the reason you made the appointment.
- Write down key personal information. Have you had any major stress or life changes recently? Sharing this type of information can help your doctor make a diagnosis.
- Make a list of all medications. Include the dosage of any medications you take, and be sure to write down any vitamins or supplements you take.
- Take a family member or friend if possible. Sometimes it can be difficult to remember all the information during a meeting. Someone accompanying you may remember what you missed or forgot.
- Write down questions you want to ask your doctor.
Preparing a list of questions will help you make the most of your time with your doctor. For Bell's palsy, some basic questions to ask your doctor include:
- What is the most likely cause of my symptoms?
- Are there other possible causes for my symptoms?
- What tests do I need?
- Is this condition likely to be temporary or long lasting?
- What treatments are available for Bell's palsy? What do you recommend?
- Are there alternatives to the first approach you suggest?
- I have other health conditions. How can I best manage these conditions together?
- Are there any brochures or other printed materials that I can take home with me? What sites do you recommend?
Feel free to ask any additional questions you have during your appointment.
What to expect from your doctor
Be prepared to answer your doctor's questions, such as:
- When did your symptoms start?
- Were your symptoms constant or occasional?
- How severe are your symptoms?
- What if something seems to improve your symptoms?
- What if something seems to make your symptoms worse?
- Have any of your relatives had Bell's palsy or facial paralysis problems?
- Have you had any symptoms of a more common infection?
What can you do during this time?
If you have facial pain:
- Take over-the-counter pain relievers. Aspirin, ibuprofen (Advil, Motrin IB, others), or acetaminophen (Tylenol, others) may help with pain.
- Apply moist heat. Placing a washcloth soaked in warm water on your face several times a day can help relieve pain.
If your eye won't close completely, try these tips:
- Use your finger to close your eyes several times throughout the day.
- Use lubricating eye drops.
- Wear glasses during the day to protect your eyes.
- Carry a handkerchief.
Share link:
- Click to share on Twitter (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Telegram (Opens in new window)
Liked this:
Like
Similar
Facial nerve paresis in newborns
The cause of FN paresis in newborns is birth trauma - damage to the FN at the site of exit from the stylomastoid foramen, or, alternatively, its terminal branches in the buccal/parotid region, caused by compression by the fetal shoulder, protrusions of the mother's pelvic bones, and obstetric forceps.
It occurs with a frequency of 0.3 to 1 case per 1000 live births, mainly in large newborns. Manifests with paresis of facial muscles of varying degrees of severity (from almost imperceptible to severe). In the vast majority of cases (90%), during the first months of a child’s life, spontaneous and complete restoration of the function of facial muscles occurs. If there is no recovery by 2-3 months of life, the need for surgical treatment is decided.
Lifestyle and Home Remedies
Home treatments may include:
- While protecting your eye, you cannot close it. Using lubricating eye drops during the day and eye ointment at night will help keep your eye moist. Wearing glasses or glasses during the day and an eye patch at night can protect the eye from being jostled or scratched.
- Exercise. Massaging and exercising your face as advised by your physical therapist can help relax your facial muscles.
Taking over-the-counter pain relievers. Aspirin, ibuprofen (Advil, Motrin IB, others), or acetaminophen (Tylenol, others) may help relieve your pain.
List of sources
- Alperovich P.M. Bell's palsy (etiology, pathogenesis, clinical picture, course, outcome) / P.M. Alperovich, A.G. Korneychuk, T.I.
- Konstantinovich and others //J. neuropathology and psychiatry named after. S.S. Korsakov. 1978. - T.78, No. 6. -WITH. 836-846.
- Batysheva T.T., Kostenko E.V., Boyko A.N. Complex treatment of facial nerve neuropathy using neuromidin and antioxidant therapy // Journal. psychiatrist, and psychopharmacologist. - 2008. No. 4. - P. 199-201.
- Complex treatment of patients with facial neuropathy and trigeminal neuralgia. Guidelines. - M., 2005. - 32 p.
- Maksimova M. Yu., Sharov M. N., Domashenko M. A. et al. Neuropathy of the facial nerve // Pharmateka. - 2011. - No. 14. - P. 46-51.
- Markin S.P. Neuropathy of the facial nerve // Neurology and Rheumatology. Supplement to the journal Consilium Medicum. - 2010. - No. 1. - P. 10-14.
Treatment of Bell's palsy
There are no separate medications for the treatment of facial neuritis. Treatment is aimed at relieving symptoms and alleviating the patient’s condition. For this purpose, drops are used to prevent the eye from drying out. In case of prolonged decompensation, tarsorrhaphy - correction of the palpebral fissure - may be required. To restore nerve function, physiotherapeutic procedures are prescribed:
- galvanization;
- massage of the cervical-collar area;
- electrophoresis.
Taking glucocorticosteroids is necessary to suppress autoimmune and inflammatory processes. The use of such drugs is effective in the first two days after the onset of paralysis.