Neurologist (algologist)
Vasilenko
Marina Gennadievna
25 years of experience
Head of the Pain Treatment Center, neurologist-algologist, member of the Society of Neurologists and Neurosurgeons, Russian Society for the Study of Pain, Association of Interdisciplinary Medicine, International Association for the Study of Pain (IASP)
Make an appointment
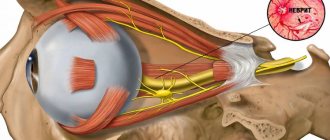
The trigeminal nerve is the largest of the 12 cranial nerves, specifically their fifth pair. It belongs to the nerves of a mixed type and includes very sensitive fibers. This name is due to the fact that the nerve is divided into three branches, providing mobility and sensitivity of the face, mucous membranes of the mouth and teeth. These are the ophthalmic, maxillary and mandibular branches.
Inflammation of the trigeminal nerve is a serious pathology that causes severe pain in the facial area. Otherwise it is called neuritis. In turn, neuralgia is pain along the trigeminal nerve. It can act as an independent sensitivity disorder, but it often accompanies inflammation, i.e. neuritis.
Symptoms and signs
Acute trigeminal neuralgia causes sudden and very severe pain along the nerve fiber. It manifests itself in attacks and is shooting and burning in nature. On average, the duration of an attack is up to 3 minutes; in approximately 7% of patients it lasts up to 3 days. Their number can reach 200 per day.
Pain from trigeminal neuralgia can be observed in different parts of the face. It all depends on which branch of the nerve was affected:
- if maxillary - in the area of the facial muscles, upper jaw and nose.
- mandibular – the pain will resemble a toothache.
- ophthalmic – in the area of the temples, forehead and above the eyebrows.
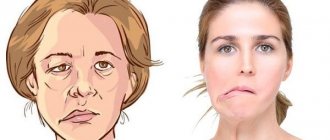
Against the background of pain, the patient develops increased anxiety and even phobias. A person strives to avoid those poses and movements that provoke unpleasant sensations in him. Other characteristic symptoms of inflammation of the trigeminal nerve:
- facial muscle spasms;
- increased salivation;
- increased or decreased sensitivity of facial skin;
- moderate increase in temperature;
- weakness and muscle pain.
Are you experiencing symptoms of trigeminal neuralgia?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
- Surgery
- Oncology
- Neurosurgery
- Radiology and Radiation Therapy
- Gynecology and new reproductive technologies
- Traumatology and Orthopedics
- Cardiology
- Neurology
- Laser surgery
- Urology, andrology and microsurgery
- Plastic surgery
- Mammalogy
- Lithotripsy
- Psychological support service
- ECO
- Weight loss
- Pressure chamber
- Endovascular surgery
- Pituitary adenomas
- Arnold-Chiari malformation and syringomyelia
- Parkinson's disease
- Hydrocephalus
- Hemifacial spasm
- Herniated discs
- Violent movements
- Brain tumors
- Vascular diseases of the brain
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Essential tremor
The trigeminal nerve (V pair of cranial nerves) contains sensory, motor and autonomic fibers (Fig. 1). The nuclei of the trigeminal nerve are located in the brain stem, at the exit from which the fibers that make up the large root reach the top of the pyramid of the temporal bone, where the trigeminal ganglion (Gasserian ganglion) lies, from which 3 branches extend: the orbital (sensory) nerve leaves the skull through the superior orbital gap, innervates the upper eyelid, conjunctiva of the eye, skin of the forehead and scalp in front; the maxillary (sensitive) nerve leaves the skull through the round foramen, penetrates the pterygopalatine fossa, innervates the skin of the lower eyelid, cheeks and nose, mucous membrane of the nasal cavity, upper jaw, etc.; The mandibular nerve (the small root of the trigeminal nerve, containing motor fibers, joins it) leaves the skull through the foramen ovale, innervates the skin of the lower part of the face, the mucous membrane of the cheeks, tongue, lower jaw, masticatory muscles, etc. The trigeminal nerve takes part in many reflexes ( corneal, mandibular, etc.). Fig. 1 Anatomy of the trigeminal nerve and its branches. Trigeminal neuralgia is a disease accompanied by paroxysmal intense unilateral facial pain in the area of the chin, lips, gums, cheeks, eyes, lasting several seconds or minutes. As a rule, middle-aged and elderly people suffer. A characteristic feature is the ability to cause pain by touching a specific area of the face or mouth.
Clinic and diagnostics.
The first attack of pain seems subjectively so pronounced and unexpected that, as a rule, patients well remember all the circumstances of the initial paroxysm even after many years. Sometimes the disease begins gradually with a slight unpleasant feeling of twitching, “electrification” in a certain area of the face, or with a toothache, which forces you to seek help from a dentist. Only the characteristic paroxysmal pain that subsequently appears allows a correct clinical diagnosis to be made and appropriate examination and treatment to be carried out. Trigger zones for the development of an attack (trigger zones) with trigeminal neuralgia are localized close to the midline, covering the lips, wings of the nose, eyebrows and chin, in rare cases located in the external auditory canal. Localization of trigger zones on the gums, tongue and palate makes it impossible to eat, talk, and perform basic hygiene requirements. Some patients with a similar arrangement of the trigger zones and severe pain lose weight, become weak and fall into a depressive state, sometimes leading to suicide attempts. The attacks recur day and night for several weeks, and then often subside. After some time, the disease appears again, and after a few years the attacks become permanent. The diagnosis of trigeminal neuralgia is confirmed by relief of pain when taking carbamazepine drugs (finlepsin, tegretol). After several years of taking carbamazepine, the effectiveness of the previous dosage usually decreases and there is a need to increase the dose of medication. Some patients cannot tolerate this drug due to side effects such as drowsiness, dizziness and staggering when walking, pain in the liver, suppression of white blood cells (leukopenia). The cause of such facial pain in most cases is compression of the trigeminal nerve root by an arterial vessel at the level of the posterior cranial fossa. Less commonly, trigeminal neuralgia can be caused by brain tumors or multiple sclerosis. Trigeminal neuralgia in multiple sclerosis, tens of times lower in frequency than typical trigeminal neuralgia, occurs as a result of demyelination of trigeminal sensory structures, mainly the entrance zone of the sensory root and the descending tract of the trigeminal nerve. It is likely that the subsequent replacement of foci of demyelination by glial cells, causing an increase in the excitability of neighboring sensory fibers, also contributes to the persistence of the pain syndrome. In addition, the development of trigeminal neuralgia in patients with multiple sclerosis may be due to vascular compression of the trigeminal sensory root. Trigeminal neuralgia in brain tumors can occur with tumors of the posterior and middle cranial fossa, pituitary tumors, epidermoids in the case where tumor growth leads to direct compression of the trigeminal nerve root or changes the spatial relationship of vessels and nerves in such a way that one of the vessels leads to compression of the trigeminal nerve root (Fig. 2). Fig. 2 Trigeminal neuralgia with epidermoid tumor. Intraoperative photography. 1 – tumor. 2 – trigeminal nerve root. To exclude a brain tumor, vascular pathology, or multiple sclerosis, all patients undergo magnetic resonance imaging (MRI) of the brain. Often in such photographs you can see the “culprit” vessel compressing the trigeminal nerve root.
Treatment.
The diagnosis of neuralgia is confirmed by relief of pain when taking carbamazepine drugs (finlepsin, tegretol). After several years of taking carbamazepine, the effectiveness of the previous dosage usually decreases and there is a need to increase the dose of medication. Some patients cannot tolerate this drug due to side effects such as drowsiness, dizziness and staggering when walking, pain in the liver area. Surgical treatment is indicated for patients who cannot tolerate carbamazepine drugs or when their effectiveness decreases. Our center is a leading institution in Russia performing all types of surgical interventions for trigeminal neuralgia with more than 20 years of experience in the diagnosis and treatment of this disease. A method of treating pathology that has proven to be highly effective is percutaneous radiofrequency trigeminal rhizotomy, an operation that involves partial destruction of the trigeminal nerve root under local anesthesia. The procedure is carried out as follows: a) a thin needle is passed through the face to the base of the skull under X-ray control (Fig. 3). Fig. 3 Percutaneous high-frequency trigeminal rhizotomy in a patient with trigeminal neuralgia of the I-II branches. Intraoperative radiography (lateral projection), confirming the correct position of the curved electrode b) stimulation of the root is carried out, which is accompanied by a pain attack in the “sick” area of the face. This stage of surgery is the most unpleasant for patients. c) partial destruction of the root is carried out due to setting an increased temperature at the tip of the needle until sensitivity in the desired area of the face decreases. Such an operation may be preferable for elderly people, those who are afraid of open surgery, and those with multiple sclerosis. In most patients, after a few years (on average 5–7 years), the numbness in the face disappears, and facial pain reappears. A more physiological operation that does not lead to numbness in the area of innervation of the trigeminal nerve is the operation of vascular decompression of the facial nerve root (Microvascular decompression). This is a microsurgical operation performed under general anesthesia, in which, after performing a small trepanation behind the ear on the side of pain, the vessel is diverted from the trigeminal nerve root in the posterior cranial fossa (Fig. 4 and 5). The effectiveness of this technique is more than 90% if patients are correctly selected for surgery. Fig. 4 Intraoperative photo of a patient with trigeminal neuralgia. The arrow indicates compression of the input zone of the trigeminal nerve root by the loops of the superior cerebellar artery (V - trigeminal nerve, SMA - 2 branches of the superior cerebellar artery, CV - petrosal vein) Fig. 5 Intraoperative photo: decompression of the input zone of the trigeminal nerve root at the brain stem was performed (V - trigeminal nerve, SMA - loop of the superior cerebellar artery, M - fragment of muscle tissue) The recovery process after microvascular decompression surgery rarely takes more than a week, after which patients are discharged home and forget about their disease forever.
Causes and risk factors
Neuralgia of the trigeminal nerve branch is a disease with many possible causes. First of all, this is compression by vessels: displaced arteries or veins. Inflammation can also be provoked by metabolic disorders and diseases that are associated with them. These are diabetes mellitus, gout and other similar pathologies.
There are other possible causes of trigeminal neuralgia:
- inflammations that occur during dental treatment;
- hypothermia (general or facial area);
- mental disorders;
- purulent diseases of the jaw bones or skull;
- infection of the body with worms;
- chronic caries or sinusitis;
- infectious and viral diseases (herpes, adenoviruses, mumps, pulmonary tuberculosis, herpes zoster);
- very severe allergies;
- brain tumors;
- inflammation of the outer, middle or inner ear;
- multiple sclerosis;
- too narrow canal of the facial nerve from birth;
- injuries or operations on the temporal bone.
Function
The sensory function of the trigeminal nerve is to provide tactile proprioceptive and nociceptive input to the face and mouth. Its motor function activates the muscles of mastication, the tensor tympani, the tensor veli palatini, the hyoid and the anterior belly of the digastric.
The trigeminal nerve carries general somatic afferents (GSAs) that innervate the facial skin through the ophthalmic (V1), maxillary (V2), and mandibular (V3) divisions. The trigeminal nerve also carries special visceral efferent (SVE) axons that innervate the muscles of mastication through the mandibular (V3) division.
Chewing muscles
The motor component of the mandibular division (V3) of the trigeminal nerve controls the movement of eight muscles, including the four masseter muscles: the stallion, the temporalis, and the medial and lateral pterygoids. The other four muscles are the tensor Veli palatini, the hyoid, the anterior digastric, and the tensor tympani. A useful mnemonic for remembering these muscles is “My ant tensor hooves 4 MoM” (Mylohyoid - Tensor Tympani + Tensor Veli Palatini - Digastric (Anterior) - 4 muscles of mastication (Temporalis, Masseter, Medial and Lateral Pterygoids))
With the exception of the tensor tympani, all of these muscles are involved in biting, chewing, and swallowing, and all are bilateral. cortical representation. A unilateral central lesion (eg, stroke), no matter how large, is unlikely to result in the observed deficit. Peripheral nerve injury can cause paralysis of the muscles on one side of the jaw, causing the jaw to deviate toward the paralysis when opened. This direction of the lower jaw is associated with the action of the functioning pterygoid bones on the opposite side.
Feeling
Main article: Somatosensory system
The two main types of sensations are the position of the touch and the temperature of the pain. Inputting the touch position attracts attention immediately, but entering the pain temperature reaches the level of consciousness with a delay; when a person steps on a pin, he is immediately aware that he has stepped on something, but the pain associated with it is postponed.
Information about the position of touch is usually conveyed by myelinated (fast-conducting) nerve fibers, and information about pain temperature is usually transmitted by unmyelinated (slow-conducting) fibers. The primary sensory sensory receptors (Meissner's corpuscles, Merkel's corpuscles, Pacinian corpuscles, Ruffini corpuscles, hair receptors, muscle spindle organs, and Golgi tendon organs) are structurally more complex than the nerve endings for pain-temperature.
Sensation in this context refers to the conscious perception of information about the position of touch and the temperature of pain, rather than the special senses (smell, vision, taste, hearing, and balance) being processed by different cranial nerves and sent to the cerebral cortex through different pathways. The perception of magnetic fields, electric fields, low frequency vibrations, and infrared radiation in some non-human vertebrates is processed by their equivalent of the fifth cranial nerve.
Touch in this context refers to the perception of detailed, localized tactile information, such as two-point discrimination (the difference between touching one point and two closely spaced points) or the difference between coarse, medium, or fine sandpaper. People without touch position perception can sense the surface of their body and perceive touch in a broad sense, but they lack perceptual details.
Position in this context refers to conscious proprioception. Proprioceptors (muscle spindle and Golgi tendon organs) provide information about joint position and muscle movement. Although most of this information is processed at the unconscious level (primarily the cerebellum and vestibular nuclei), some is available at the conscious level.
The sensations of touch and pain temperature are processed in different ways in the central nervous system. This rigid distinction persists all the way to the cerebral cortex. In the cerebral cortex, sensations are connected to other areas of the cortex.
Sensory pathways
Sensory pathways from the periphery to the cerebral cortex are separated for the sensations of touch and temperature. All sensory information is sent to specific nuclei in the thalamus. The thalamic nuclei, in turn, send information to specific areas in the cerebral cortex. Each pathway consists of three sequentially connected bundles of nerve fibers:
Secondary neurons in each tract decussate (cross the spinal cord or brainstem) because the spinal cord is segmented. Intersecting fibers later reach and connect these segments to higher centers. The optic chiasm is the main cause of chiasm; The nasal fibers of the optic nerve are crossed (so each hemisphere of the brain receives contralateral - opposite - vision) to keep the interneuronal connections responsible for processing information short. All sensory and motor pathways converge and diverge to the contralateral hemisphere.[2]
Although sensory pathways are often depicted as chains of individual neurons connected in series, this is an oversimplification. Sensory information is processed and modified at each level of the chain by interneurons and input from other areas of the nervous system. For example, cells of the main nucleus of the trigeminal nerve (Main V in the diagram below) receive input from the reticular formation and the cerebral cortex. This information facilitates the final exit of cells in Main V to the thalamus.
C = Cervical Segment, S = Sacral Segment, VPL = Ventral Posterolateral Nucleus, SI = Primary Somatosensory Cortex, VM = Ventromedial Prefrontal Cortex, MD = Medial Dorsal Thalamic Nucleus, IL = Intralaminar Nucleus, VPM = Ventrally Posteromedial Nucleus, Principal V = Principal trigeminal nucleus, Spine V = Trigeminal nucleus
Information about the position of the touch is transmitted from the body to the thalamus through the middle lemniscus, and from the face through the trigeminal lemniscus (both anterior and posterior trigeminothalamic tracts). Information about temperature and pain is transmitted from the body to the thalamus through the spinothalamic tract, and from the face by the anterior trigeminal lemniscus (also called the anterior trigeminothalamic tract).
The sensory position and pain temperature pathways from the face and body merge in the brainstem, and the whole body sensory maps of touch position and pain temperature are projected to the thalamus. Information about the position of the touch and the temperature of the pain is projected from the thalamus to the cerebral cortex.
Summary
The complex processing of pain temperature information in the thalamus and cortex (as opposed to the relatively simple and straightforward processing of touch position information) reflects a phylogenetically older, more primitive sensory system. The detailed information obtained from peripheral touch position receptors is superimposed on a background of awareness, memory, and emotion set in part by peripheral pain temperature receptors.
Although touch position perception thresholds are relatively easy to measure, pain temperature perception thresholds are difficult to define and measure. “Touch” is an objective sensation, while “pain” is an individual sensation that varies from person to person and is driven by memory and emotion. Anatomical differences between the pathways for sensing the position of touch and the sensation of temperature and pain help explain why pain, especially chronic pain, is difficult to manage.
Possible complications
Over time, symptoms of inflammation of the trigeminal nerve can give rise to neuropathic complications and lead to the development of secondary pain syndrome in the head. In the chronic form of the disease, the auditory and facial nerves are irritated. Without treatment, trigeminal neuralgia can lead to more serious complications:
- dystrophy of masticatory muscles;
- decreased sensitivity of the affected area;
- Sykinesia (cooperative movements in which one nerve controls many muscles);
- contracture and spontaneous contraction of the facial muscles;
- conjunctivitis.
What is mandibular nerve injury?
By this concept, dentists mean injury to one of the nerves:
- chin;
- lingual;
- alveolar.
Types of injuries include sprain, compression, crushing and rupture - partial or complete. The cause of the stretching is the long-term retraction of the mucoperiosteal flap, which is created by an implant of greater length than necessary. Crush injuries and compression are caused by needle injuries during the administration of anesthesia. Rupture occurs in two cases: when cutting the mucosa or during preparation of the hole for the implant.
When to see a doctor
If you experience symptoms of trigeminal neuralgia, you should immediately consult a doctor, as it may be a sign of another serious disease. In the treatment of neurological pathologies, accurate and timely diagnosis is extremely important. This is done by a neurologist, with whom you can make an appointment at our clinic in the center of Moscow. The specialist knows not only how to relieve trigeminal neuralgia, but also how to correctly diagnose it in order to prescribe effective treatment in the future.
Recommendations
- "trigeminal nerve". TeachMeAnatomy.info
. - Excerpt from Cunningham's Textbook of Anatomy
- Luebbert, Matthias; Kereme, Jessica; Schoebel, Nicole; Beltran, Leopoldo; Wetzel, Christian Horst; Hutt, Hans (21 October 2013). "Receptor potential transient channels encode volatile chemicals sensed by rat trigeminal ganglion neurons." PLOS ONE
.
8
(10): e77998. Bibcode:2013PLoSO ... 877998L. doi:10.1371/journal.pone.0077998. PMC 3804614. PMID 24205061. Received October 10, 2014. - Kell CA, von Kriegstein K, Rösler A, Kleinschmidt A, Laufs H (2005). "Sensory cortical representation of the human penis: new insights into somatotopy in the male homunculus". J. Neurosci
.
25
(25):5984–5987. Doi:10.1523/JNEUROSCI.0712-05.2005. PMC 6724806. PMID 15976087.
Diagnosis of trigeminal neuralgia
A preliminary diagnosis can be made by a neurologist based on the patient’s complaints, studying the history of his disease and an objective examination of the face with an assessment of symmetry at rest and when trying to smile. Also, during the consultation, the doctor may conduct additional tests, asking the patient to close his eyes, purse his lips, frown, etc.
Laboratory and instrumental diagnostics of trigeminal neuralgia include the following examinations:
- general blood and urine tests;
- computed tomography (CT) and magnetic resonance imaging (MRI);
- radiography of the paranasal sinuses;
- panoramic radiography of the oral cavity;
- electroneuromyography to determine the localization of inflammation.
Treatment
Treatment of inflammation of the trigeminal nerve is carried out depending on the severity of symptoms. First, conservative therapy is prescribed. If this does not help, doctors resort to surgical methods. Their essence is to eliminate the cause of neuralgia. This may be compression of the nerve by the vessel. Surgical treatment is carried out using radiofrequency destruction, microvascular decompression or percutaneous surgery.
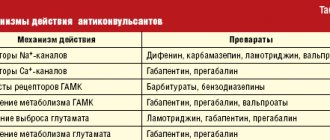
What drugs are most effective for the treatment of trigeminal neuralgia:
- antibiotics. Prescribed for infectious nature of the disease;
- glucocorticosteroids. Relieves severe inflammation in the body;
- non-steroidal anti-inflammatory drugs (NSAIDs). Helps suppress inflammatory processes;
- painkillers. Relieves soreness in the facial muscles;
- muscle relaxants.
To improve metabolic processes in the nervous tissue, the patient is prescribed B vitamins. How to relieve acute pain with trigeminal neuralgia:
- use anticonvulsants;
- provide physical rest, preferably bed rest;
- Apply an anti-inflammatory ointment or a warm compress to the site of pain.
Home remedies
Before treating trigeminal neuralgia at home, you should consult a doctor, since many remedies can only worsen the situation. If the specialist allows it, it is also possible to use various home recipes.
According to recommendations for trigeminal neuralgia, it is worth consuming orally or lubricating the affected side with birch sap. You need to drink 4-5 glasses per day. Heated buckwheat folded in cotton cloth will help relieve pain. The compress is made 2 times a day, keeping it at the site of inflammation until it cools down. At home, it is useful to massage the sore area: rub, stroke and lightly knead the area of inflammation.
Sources
- Blumenfeld, H. Neuroanatomy in Clinical Cases
. Sinauer Associates, 2002. - Brodahl, A. Neurological anatomy in relation to clinical medicine
, 3rd ed. Oxford University Press, 1981. - Brodahl, P. The Central Nervous System
. Oxford University Press, 2004. - Carpenter, M.B., Soutine, J. Human Neuroanatomy
, 8th ed. Williams and Wilkins, 1983. - DeJong, R. N. Neurological Examination
, 3rd ed. Hober, 1970. - Kandel, E. R., Schwartz, J. H., Jessel, T. M. Principles of Neuroscience
, 4th ed. McGraw-Hill, 2000. - Martin, J. H. Text and Atlas of Neuroanatomy
, 3rd ed. McGraw-Hill, 2003. - Patten, J. Neurological Differential Diagnosis
, 2nd ed. Springer, 1996. - Ropper, A.H., Brown, R.H. Adam and Victor's Principles of Neuroscience
, 8th ed. McGraw-Hill, 2001. - Wilson-Pauwels, L., Akesson, E. J., Stewart, P. A. Cranial nerves: anatomy and clinical commentary
. B. K. Dekker, 1998.
Myths and dangerous misconceptions in treatment
Due to the fact that neuralgia does not affect the general condition of the body, many patients postpone visiting a doctor and treating the trigeminal nerve. In fact, this is the wrong approach, since the disease can lead to paralysis and muscle paresis. In addition, it has a significant impact on psychological and social aspects of life.
No less important is the fact that painkillers for trigeminal neuralgia provide only a temporary effect. Over time, anticonvulsant medications may also stop working as they become addictive. Therefore, you should not abuse medications. They only relieve the symptoms of neuralgia, and its cause can only be identified by a qualified specialist.
Prevention
There is no specific prevention against neuralgia. Doctors only recommend eliminating as much as possible exposure to the body of those risk factors that can lead to nerve inflammation. To avoid this, it is necessary to prevent hypothermia of the face, especially in the summer when using fans and air conditioners. It is important to harden yourself and worry less in order to reduce the impact of stress. It is also imperative to treat underlying diseases that are risk factors for neuralgia.
Causes and prevention of mandibular nerve injuries
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.