Ulcerative colitis
- inflammatory bowel disease, which belongs to the group of immune-mediated chronic diseases of the large intestine.
Inflammatory bowel diseases are one of the most complex pathologies in modern gastroenterology and coloproctology. The treatment of these diseases is based on an interdisciplinary approach, and its effect depends entirely on the mutual understanding and productive interaction of gastroenterologists and coloproctologists, who develop a treatment strategy during a multidisciplinary consultation.
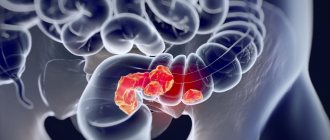
Ulcerative colitis is a chronic autoimmune inflammation of the colon mucosa. Usually the process starts from the rectum and then spreads to the overlying parts of the large intestine (sigmoid, descending, transverse colon, right colon). With extensive damage, the terminal ileum is involved in the pathological process (retrograde ileitis). The pathology is characterized by alternating periods of exacerbation and remission, as well as the development of local and systemic complications.
The disease can also be found under the name ulcerative colitis.
Causes of the disease
The exact etiology of the disease has not yet been determined. Ulcerative colitis is believed to occur when a number of factors interact. Among them: genetic predisposition, disorders of the immune system, imbalance of intestinal microflora and the influence of certain environmental factors.
Thus, the presence of ulcerative colitis or Crohn's disease in relatives increases the risk of its occurrence in the patient. However, genetic predisposition is not associated only with a mutation of one gene. Currently, 163 gene loci responsible for the development of ulcerative colitis or Crohn's disease have been identified. It is also known that genetic factors influence the severity of inflammation of the colon, the localization of the inflammatory process, the occurrence of complications and extraintestinal manifestations.
The state of the symbiont (normal) intestinal microflora plays an important role in the development of the disease. Normally, each gram of feces contains from 1010 to 1012 bacteria (approximately 400-500 species), i.e. up to 60% of the stool mass is represented by microorganisms. Immunocompetent cells of the mucous membrane constantly interact with the contents of the colon, ensuring the tolerance of bacteria. Impaired recognition of bacterial markers leads to activation of the inflammatory process and the onset of the disease.
It is also known that the first attack of ulcerative colitis or its recurrence can be triggered by food-borne antigens that cause allergies, or the cause can be stress.
Pathogenesis of ulcerative colitis
The development of the disease is ensured by various mechanisms of tissue and cellular damage. This leads to immunological imbalance, release of pro-inflammatory mediators and tissue damage. The resulting antigens (bacterial and tissue) cause stimulation of cells of the immune system (T- and B-lymphocytes). Inflammation leads to a deficiency of immunoglobulins. As a result, these processes increase the activity of B cells with the release of immunoglobulins M and G and promote the penetration of microorganisms.
Active synthesis of immunoglobulins M and G is accompanied by the formation of immune complexes and activation of the complement system, which exhibits a cytotoxic effect and causes the migration of neutrophils and macrophages. Immunocompetent cells release inflammatory mediators, causing the destruction of epithelial cells.
In addition to the pathological reaction of the immune system, epithelial tissues are damaged under the influence of active oxygen and protease, which leads to activation of the cell death mechanism.
Defects in the intestinal mucosa also play an important role in the development of the disease. The impaired ability to restore the mucous membrane and damage to its barrier function enable various bacterial and food antigens to penetrate deep tissues, triggering a chain of immune and inflammatory reactions.
The psychological characteristics of the patient’s personality, especially emotional instability, are also important. The trigger for the development of the disease can be an abnormal neurohumoral response obtained during the individual reaction to stress.
Manifestations of the disease
Ulcerative colitis is characterized by a wide variety of clinical manifestations. The Montreal classification helps to systematize manifestations (Table 1). According to it, it is possible to assess the characteristics of the course of the disease, the extent of the lesion, the severity of the attack and the presence of complications.
| Proctitis | The lesion is limited to the rectum |
| Left-sided colitis | The lesion extends to the left flexure of the colon (including proctosigmoiditis) |
| Total colitis | (Including subtotal colitis, as well as total UC with retrograde ileitis) |
Table 1. Montreal classification of ulcerative colitis by extent of lesion.
The course of ulcerative colitis is characterized by three options:
- Acute course (less than 6 months from the onset of the disease). It can occur with a fulminant (quick) or gradual onset.
- Chronic continuous course, which is characterized by the absence of more than 6-month periods of remission against the background of adequate therapy.
- Chronic relapsing course (presence of more than 6-month periods of remission). It can be either rarely recurrent (once a year or less) or frequently recurrent (2 or more times a year).
The presence of extraintestinal manifestations, the development of complications, the intensity and severity of the current exacerbation and the emergence of resistance to treatment in the patient (for example, hormonal dependence) determines the severity of ulcerative colitis.
The severity of the current exacerbation or attack is also used to create a treatment plan and formulate a diagnosis. In clinical practice, the Truelove-Witts criteria and the disease activity index (Mayo index) are used for this purpose. There are three levels of attack: light, medium, heavy.
The course of ulcerative colitis has periods of exacerbation (relapse) and remission.
Relapse (exacerbation or attack) is characterized by the appearance of symptoms of the disease against the background of remission, which was achieved through medication or occurred spontaneously. If a relapse occurs less than 3 months after remission, then it is considered early. Signs of relapse: an increase in the frequency of bowel movements with the release of blood, as well as changes in the colon mucosa, which are found during endoscopic examination.
Remission of ulcerative colitis involves healing of the colon mucosa in the absence of the main symptoms of the disease.
Publications in the media
Nonspecific ulcerative colitis (UC) is a chronic inflammatory disease of the colon of unknown etiology, characterized by ulcerative-necrotic changes in its mucous membrane.
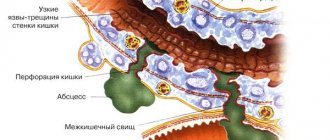
The disease always begins in the rectum and spreads proximally. Total damage to the colon occurs in 25% of cases. In severe cases, the damage can spread to the submucosa, muscular and serous membranes of the intestinal wall. Characterized by the formation of ulcers in the colon and rectum, bleeding, abscessation of the crypts of the mucous membrane and inflammatory pseudopolyposis. The disease often causes anemia, hypoproteinemia and electrolyte imbalance, and, less frequently, can lead to perforation or colon cancer.
Frequency - 2-7: 100 000. Two peaks of incidence - 15-30 years (larger peak) and 50-65 years (smaller). The predominant gender is female.
Classification • By clinical course •• acute form •• Chronic recurrent •• Chronic continuous • By severity •• Mild severity ••• Stool 4 times a day or less, pasty ••• Small amounts of blood in the stool •• • Fever, tachycardia, anemia are uncharacteristic; body weight does not change, ESR is not changed •• Severe course ••• Stool 20–40 r/day, liquid ••• Stool in most cases contains an admixture of blood ••• Body temperature 38 °C and above ••• Pulse 90 V minute or more ••• Decrease in body weight by 20% or more ••• Severe anemia ••• ESR more than 30 mm/h •• Moderate severity includes indicators that are between the parameters of mild and severe degrees.
Clinical picture
• The onset of the disease may be acute or gradual.
• The main symptom is repeated watery stools mixed with blood, pus and mucus, combined with tenesmus and false urge to defecate. During the period of remission, diarrhea may completely stop, but the stool is usually pasty, 3-4 times a day, with a slight inclusion of mucus and blood.
• Cramping pain in the abdomen. Most often this is the area of the sigmoid, colon and rectum, less often - the area of the navel and cecum. Typically, the pain intensifies before defecation and decreases after bowel movement. The localization of pain depends on the level of the lesion. Typically, the pain intensifies before defecation and decreases after bowel movement.
• Possible damage to other organs and systems •• Skin and mucous membranes: dermatitis, aphthous stomatitis (5–10%), gingivitis and glossitis, erythema nodosum (1–3%) and erythema multiforme, pyoderma gangrenosum (1–4%), ulcers lower extremities •• Arthralgia and arthritis (in 15–20% of cases), incl. and spondylitis (3–6%) •• Ophthalmological complications (4–10%): episcleritis, uveitis, iridocyclitis, conjunctivitis, cataracts, retrobulbar optic neuritis, corneal ulcers •• Liver: fatty hepatosis (7–25%), cirrhosis (1–5%), amyloidosis, primary sclerosing cholangitis (1–4%), chronic active hepatitis.
Laboratory tests • Analysis of peripheral blood •• Anemia (post-hemorrhagic - as a result of blood loss; bone marrow reaction to latent inflammation; malabsorption of iron, folic acid, vitamin B12) •• Leukocytosis of varying severity •• Increased ESR •• Hypoprothrombinemia •• Hypoalbuminemia due to malabsorption of amino acids •• Increased content of a1- and a2-globulins •• Hypocholesterolemia • Electrolyte disturbances •• Hypokalemia as a result of decreased absorption of both ions directly and vitamin D •• Hypomagnesemia.
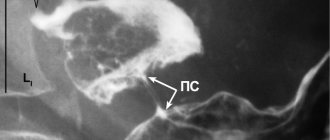
Special studies • Sigmoidoscopy during an exacerbation is carried out without preliminary bowel preparation • Colonoscopy is prescribed after the acute phenomena have subsided, because in severe cases of the disease, perforation of the ulcer or toxic dilation is possible •• Mild UC - granularity of the mucous membrane •• Moderate UC - the mucous membrane bleeds on contact, there are ulcerative lesions and mucous exudate •• Severe UC - spontaneous bleeding from the intestinal mucosa , extensive ulcerative lesions and the formation of pseudopolyps (epithelium-covered granulation tissue) • Irrigography •• Reduced severity or absence of haustration •• Uniform narrowing of the intestinal lumen, its shortening and rigidity of the walls (the appearance of a “water pipe”) •• Longitudinal orientation of the folds of the mucous membrane with changes their structure according to the type of small and large retina •• Jagged and unclear contours of the intestinal tube due to the presence of ulcers and pseudopolyps (in the acute phase) •• The procedure is contraindicated in the development of toxic megacolon • Plain radiography of the abdominal organs is especially important in cases of severe UC, when colonoscopy and irrigography are contraindicated •• Shortening of the colon •• Lack of haustration •• Irregularity of the mucous membrane •• Dilatation of the colon (toxic megacolon) •• Free gas under the dome of the diaphragm during perforation.
Differential diagnosis • Acute dysentery • Crohn's disease • Intestinal tuberculosis • Diffuse familial polyposis of the colon • Ischemic colitis.
TREATMENT
Diet. Various diet options No. 4. You should avoid eating raw fruits and vegetables for the purpose of mechanically sparing the inflamed mucous membrane of the colon. In some patients, a dairy-free diet can reduce the severity of clinical manifestations, but if it is ineffective, it should be abandoned.
Lead tactics
• For sudden exacerbations, bowel emptying with intravenous fluids for a short period of time is indicated. Total parenteral nutrition allows for long-term rest for the intestines.
• Salicylosulfonamide drugs are effective for all degrees of severity of the disease, causing remission and reducing the frequency of exacerbations •• Sulfasalazine 0.5–1 g 4 times a day until clinical manifestations subside, then 1.5–2 g/day for a long time (up to 2 years ) for the prevention of relapses, or •• Salazodimethoxin 0.5 g 4 times / day for 3-4 weeks, then 0.5 g 2-3 times / day for 2-3 weeks •• Mesalazine - 400– 800 mg 3 times a day orally for 8–12 weeks; for the prevention of relapses - 400–500 mg 3 times a day if necessary for several years. The drug should be taken after meals with plenty of water. For left-sided UC, the drug can be used rectally (suppositories, enema). Indicated in cases of insufficient effectiveness and poor tolerability of sulfasalazine.
• GK - for acute forms of the disease, severe relapses and moderate forms, resistant to other drugs •• For distal and left-sided colitis - hydrocortisone 100-250 mg 1-2 times a day rectally by drip or in microenemas. If effective, the drug should be administered daily for 1 week, then every other day for 1–2 weeks, then gradually, over 1–3 weeks, the drug is discontinued •• Prednisolone orally 1 mg/kg/day, in extremely severe cases - 1.5 mg/kg/day In case of an acute attack, it is possible to prescribe 240–360 mg/day intravenously, followed by switching to oral administration. 3-4 weeks after achieving clinical improvement, the dose of prednisolone is gradually reduced to 40-30 mg, then sulfasalazine can be added, and then the reduction is continued until complete withdrawal.
• As an adjuvant in combination with sulfasalazine or GC - cromoglycic acid in an initial dose of 200 mg 4 times a day 15 minutes before meals.
• For mild to moderate manifestations without signs of toxic megacolon, a consolidative (eg, loperamide 2 mg) or anticholinergic drugs are cautiously prescribed. However, the use of drugs that actively inhibit peristalsis can lead to the development of toxic dilatation of the colon.
• Immunosuppressants, such as mercaptopurine, azathioprine, methotrexate (25 mg IM 2 times a week), hydroxychloroquine.
• If there is a risk of developing anemia, take iron supplements orally or parenterally; in case of massive bleeding - blood transfusion.
• For toxic megacolon •• Immediate withdrawal of consolidating and anticholinergic drugs •• Intensive infusion therapy (0.9% sodium chloride solution, potassium chloride, albumin) •• Corticotropin 120 units/day or hydrocortisone 300 mg/day intravenous drip •• Antibiotics (eg, ampicillin 2 g or cefazolin 1 g IV every 4–6 hours).
Contraindications • Sulfasalazine is contraindicated in case of hypersensitivity, liver or kidney failure, blood diseases, porphyria, glucose-6-phosphate dehydrogenase deficiency, breastfeeding • Mesalazine is contraindicated in case of hypersensitivity to salicylates, blood diseases, liver failure, gastric and duodenal ulcers, children under 2 years old, breastfeeding.
Surgical treatment • Indications •• Development of complications ••• Toxic megacolon with ineffective intensive drug therapy for 24–72 hours ••• Perforation ••• Excessive bleeding with unsuccessful conservative therapy (rare) ••• Carcinoma ••• Suspicion of carcinoma with intestinal strictures •• Lack of effect from conservative therapy, rapid progression of the disease •• Growth retardation in adolescents, not corrected by conservative treatment •• Dysplasia of the mucous membrane •• Disease duration of more than 10 years (increased risk of cancer) • The following groups of surgical interventions are distinguished • • Palliative (disconnection operations) - the application of a double-barreled ileo- or colostomy •• Radical - segmental or subtotal resection of the colon, colectomy, coloproctectomy •• Restorative-reconstructive - the application of an ileo-rectal or ileo-sigmoid anastomosis end to end.
Complications • Acute toxic dilatation (toxic megacolon) of the colon (up to 6 cm in diameter) develops in 3–5% of cases. It is probably caused by severe inflammation with damage to the muscular lining of the colon over a large area and disruption of the nervous regulation of intestinal functions. A certain role belongs to the inadequate prescription of anticholinergics and fixative drugs. The condition is usually severe, with high fever, abdominal pain, significant leukocytosis, exhaustion, and death is possible. Treatment is intensive drug therapy for 48–72 hours. Failure to respond to treatment is an indication for immediate total colonectomy. Mortality is about 20% with a higher rate in patients over 60 years of age • Major bleeding. The main symptom of UC is bleeding from the rectum (up to 200–300 ml/day). Massive bleeding is considered to be blood loss of at least 300-500 ml/day • Perforation of colon ulcers in UC occurs in approximately 3% of cases and often leads to death • Strictures in UC - 5-20% of cases • Colon cancer. Patients with subtotal or total colon disease and a disease duration of more than 10 years have an increased risk of colon cancer (at 10 years, the risk of carcinoma is 10% and can increase to 20% after 20 years and to 40% after 25–30 years) • • Colon cancer arising in the context of UC is usually multifocal and aggressive •• In patients with UC more than 8–10 years old, annual colonoscopy examinations with biopsies every 10–20 cm should be performed. In the presence of high-grade dysplasia, the possibility of prophylactic total colonectomy.
Synonyms • Ulcerative-hemorrhagic colitis, nonspecific • Ulcerative-hemorrhagic colitis, idiopathic • Ulcerative-trophic colitis • Ulcerative proctocolitis • Ulcerative-hemorrhagic rectocolitis • Purulent hemorrhagic rectocolitis.
Reduction. UC - nonspecific ulcerative colitis.
ICD-10 • K51 Ulcerative colitis
Treatment of ulcerative colitis
Ulcerative colitis requires complex treatment, which includes drug therapy, surgical treatment if complications occur, and a special diet. The choice between a conservative and surgical method takes into account a number of criteria. These include: the extent of damage to the colon, the severity of the exacerbation, the effectiveness of the therapy already carried out, the presence of extraintestinal manifestations and complications.
The main goal of treatment for ulcerative colitis is to achieve long-term and stable remission, healing of the colon mucosa, prevention of surgical complications, and improvement of the patient’s quality of life. If the disease progresses or life-threatening complications develop, surgical treatment is performed.
When remission is achieved, the patient should remain on maintenance (anti-relapse) pharmacotherapy. It is important to note that glucocorticosteroids should not be used as maintenance therapy. They are used in severe attacks to induce remission, and then the patient must be switched to drugs of other groups (5-ASA, cytostatics, biological therapy, etc.)
Postoperative period
In the normal course of the postoperative period, discharge is made 5-7 days after surgery.
In the postoperative period, a gradual reduction in the intake of hormonal drugs is required, up to their discontinuation.
Regular examination and observation by an endocrinologist, gastroenterologist and proctologist is required.
Cost of treatment
Free treatment under compulsory medical insurance policy
A type of social insurance for citizens of the Russian Federation, which provides guarantees of free medical care in the detection of surgical diseases.
Quota treatment (VMP)
Providing medical care for the most severe diseases of the gastrointestinal tract, requiring the mandatory use of expensive instruments and/or the use of complex surgical techniques.