- Causes of pulmonary edema
- What diseases are there a risk of edema?
- Types of pathology
- Symptoms of pulmonary edema
- Diagnostics
- Treatment of pulmonary edema
- Predictions and prevention
Pulmonary edema is a condition in which gas exchange is disrupted and respiratory failure develops. Swelling occurs due to an imbalance of pressure in the pulmonary capillaries and the release of a large amount of edematous fluid into the lung tissue without its reabsorption.
Causes of pulmonary edema
A mixture of edematous fluid (transudate) and a liquid substance that “lines” the alveoli of the lungs from the inside (it is called “pulmonary surfactant”) enters the lumen of the alveoli, where it combines with air. This leads to the formation of foam, which creates an obstacle to the flow of oxygen. Lack of oxygen provokes the development of shortness of breath, due to which the pressure inside the chest decreases and blood flow to the right side of the heart increases.
Pulmonary edema causes infiltration of the alveoli and is manifested by symptoms that indicate oxygen starvation, which is dangerous for tissues. The patient requires emergency care due to the high risk of death due to suffocation.
First aid for pulmonary edema in the elderly
Pulmonary edema is a serious and serious pathological condition that requires urgent medical attention. What to do in case of pulmonary edema in older people and fluid appearing in the lungs?
Basic rules for providing first aid:
- The patient must be brought into the following position: lower his legs, holding the edge of the bed with his hands. This will help reduce pressure in the chest area and improve gas exchange. Shortness of breath will decrease as the stagnation of blood in the pulmonary circulation will weaken.
- It is necessary to apply venous tourniquets to the upper thigh for 30 minutes. This will lead to the fact that the flow of venous blood to the heart will decrease, and the patient will feel better.
- In the room where an elderly person is, you need to open the windows, as he needs fresh air. A stuffy room can aggravate the condition.
- In a situation where pulmonary edema is a consequence of a heart attack, the patient needs to be given drugs from the nitrate group, for example, nitroglycerin.
- Monitoring the respiration and pulse of an elderly person.
- To prevent foaming, vapors of 30% ethyl alcohol help (only if the patient is not susceptible to an allergic reaction to it).
Treatment of pulmonary edema occurs in the intensive care unit of the hospital, regardless of what caused it. A set of measures is being carried out to alleviate the patient’s condition.
Read material on the topic: Inhaler for older people: how to choose and how to use correctly
What diseases are there a risk of edema?
Pathology indicates a complication of the underlying disease, increases its duration and worsens the prognosis of treatment. The most dangerous from the point of view of pulmonary edema include:
- Heart diseases. Respiratory failure often occurs against the background of pathologies of the heart and blood vessels. Cardiogenic pulmonary edema is a life-threatening complication that develops with myocardial infarction, aneurysm, endocarditis and myocarditis, severe hypertension, and pathological conditions caused by congenital or acquired heart defects.
- Pulmonary diseases. At risk are patients with injuries and severe diseases of the respiratory tract. Respiratory edema develops against the background of exacerbation of chronic bronchitis and bronchial asthma, tuberculosis, and lobar pneumonia. The risk is increased by tumor lesions of the lung tissue, pleurisy, and chest injuries, which are accompanied by pneumothorax. If a person is connected to a ventilator for a long time and receives a mixture with a high concentration of oxygen, this also leads to an imbalance of pressure in the pulmonary capillaries and the release of exudate.
- Infectious diseases. In severe cases or inadequate treatment of whooping cough, scarlet fever, influenza, diphtheria and other infectious diseases, edema develops, followed by acute pulmonary failure. In young children, this clinical syndrome can cause acute laryngitis and the proliferation of adenoids.
- Pathologies of intrauterine development and difficult childbirth. Severe pregnancy, prematurity, oxygen hypoxia, fetal bronchopulmonary dysplasia - these factors increase the risk of developing pulmonary failure in newborns. In pregnant women, pulmonary failure can develop due to eclampsia. The same phenomenon occurs with ovarian hyperstimulation syndrome against the background of stimulation of ovulation by hormonal drugs.
- Foreign bodies entering the respiratory tract. Mechanical asphyxia is one of the possible causes of acute respiratory failure. Pathology occurs when foreign objects enter the respiratory tract, after drowning or attempted hanging, or blockage of the respiratory tract with vomit.
- Diseases of the urinary system and gastrointestinal tract. Nephrogenic pulmonary edema can be complicated by acute inflammatory diseases, which are accompanied by renal dysfunction and the development of severe renal failure. In gastroenterology, patients with liver cirrhosis, severe pancreatitis, and intestinal obstruction have to deal with respiratory failure.
- Neurological diseases. Traumatic brain injuries, meningitis, encephalitis, neoplasms, cerebral hemorrhages, complications after brain surgery - all this leads to neurogenic pulmonary edema.
- Allergies, injuries, poisoning. Acute respiratory failure can be caused by the ingestion of various toxic substances into the body. Pulmonary edema is encountered by patients with alcohol and drug intoxication, poisoning with drugs, salts of heavy metals, and toxic gases. Pulmonary insufficiency is diagnosed in case of blood poisoning, burns with a large affected area, acute allergic reactions.
What complications can there be?
The main threat posed by pulmonary edema in older people is insufficient oxygen supply to tissues. Even if the disease can be stopped, serious transformations will occur in the brain. Pulmonary edema will cause significant damage to heart tissue.
Other adverse consequences of the disease include:
- phenomena of stagnation in the respiratory organs;
- decreased local blood circulation;
- pulmonary emphysema (a disease in which destructive morphological changes in the alveolar walls are observed).
Insufficient oxygen supply leads to memory deterioration in the patient. During the day he will always want to sleep. With this pathology, general lethargy and bad mood are observed. The condition requires careful monitoring; in case of serious deterioration, you should seek medical advice.
Pulmonary edema in older people is a serious pathology. Even when the disease manifests itself in a subacute or prolonged form, the likelihood of complications is high. In such cases, you should immediately seek medical help.
Types of pathology
Depending on the cause of development, pulmonary edema can be cardiogenic or non-cardiogenic. In the first case, the cause of respiratory failure is cardiovascular disease. The second category includes all other pulmonary edema caused by diseases of the gastrointestinal tract, nervous system, and injuries.
Pulmonary edema is also classified according to the nature of its course. There are four types of pathology development:
- With fulminant development, severe respiratory failure occurs within a few minutes and leaves no chance of survival.
- Acute swelling can take up to four hours to develop. This form is considered less dangerous than the previous one, but in the absence of timely assistance, the risk of death is extremely high. Most often, acute pulmonary edema develops with myocardial infarction, traumatic brain injury, and acute allergic reactions.
- In case of intoxication, renal and liver failure, subacute pulmonary edema may occur. The intensity of symptoms is constantly changing, so continuous medical monitoring of the patient's condition is required.
- Prolonged swelling may take several days to develop. Symptoms are mild compared to the acute and subacute forms. Prolonged pulmonary edema usually occurs against the background of various chronic diseases, including heart failure.
Symptoms
Acute pulmonary edema is usually manifested by severe shortness of breath, a feeling of lack of air, anxiety and fear of death. The patient experiences heart rhythm disturbances. Wheezing, chest pain, and increased sweating appear. On auscultation, a prolonged exhalation is heard against the background of harsh breathing.
If the swelling is localized in the interstitial tissue, it is difficult for the patient to take a breath, as if he is trying to catch air in his mouth. It is more difficult to breathe while lying down, so he is forced to take a sitting or standing position. Due to lack of oxygen, cyanosis develops - a bluish coloration of the skin. An increase in blood pressure and the appearance of profuse sweat are also possible. Another clinical sign is moist bubbling rales. First they appear in the lower parts of the lungs, then spread to the entire surface of the lungs, large bronchi, trachea and become audible even at a distance. Foamy pink sputum appears.
Rate of edema development:
- A few seconds - lightning-fast swelling, ending in death.
- Several hours - acute edema, which is usually a complication of myocardial infarction and anaphylactic shock. It is characterized by high mortality even with timely medical care.
- Several days - prolonged (chronic pulmonary edema), which occurs against the background of chronic bronchopulmonary diseases or chronic heart failure. As a rule, it occurs with a blurred clinical picture, which makes timely diagnosis difficult
Separately, subacute edema is distinguished, characterized by a wave-like course. Occurs against the background of endogenous intoxication (for example, with liver failure). It has a fairly favorable prognosis, provided timely assistance is provided.
Symptoms of pulmonary edema
Before the main symptoms of pulmonary failure appear, patients experience weakness and dizziness, a feeling of tightness in the chest, headache, and dry cough. A few hours after the first symptoms of the pathology, an attack of cardiac asthma develops - the first stage of pulmonary edema. It manifests itself:
- severe lack of air;
- severe dry cough;
- increased heart rate;
- hoarse breathing;
- profuse sweating;
- pale skin, blueness of nails and lips;
- feelings of fear and anxiety.
As a rule, the attack occurs at night or before dawn. In patients with cardiac diseases, cardiac asthma can be caused by physical or emotional stress and hypothermia.
As edema develops, the alveoli become involved in the pathological process. This leads to increased suffocation. The patient experiences severe shortness of breath, the face becomes burgundy-blue and puffy, the veins in the neck swell, and mental retardation appears. Breathing becomes hoarse, foam mixed with blood comes out of the mouth.
In the absence of medical care, the patient loses consciousness and falls into a coma. In this state, blood pressure decreases critically, breathing becomes shallow, and the pulse weakens. The cause of human death is asphyxia, in which the body experiences an acute lack of oxygen with an excess of carbon dioxide.
How to give first aid
First aid to a patient who has pulmonary edema should be provided by those around him:
- First of all, make the victim sit comfortably, his legs should hang over the seat. This will help reduce the amount of blood entering the pulmonary circle.
- In some cases, the patient can be given medications. For example, if the swelling was caused by heart disease, then it is necessary to put nitroglycerin under the victim’s tongue. Diuretics that reduce venous return (eg, Furosemide) may also help. This medicine is administered intravenously, but the dosage is selected only by a doctor.
- Next, to reduce venous return, you need to apply a cuff to your leg or arm. This will partially compress the veins, leaving only a small flow of air under the pressure cuff. It is especially useful for pulmonary edema in bedridden elderly patients.
- Before the ambulance arrives, the patient should be given sedatives (Relanium is excellent). During this procedure, the amount of catecholamines in the bloodstream will decrease, and the venous flow of blood to the heart muscle will also decrease.
- If the patient suddenly begins to foam, then you need to moisten a cotton swab in medical alcohol and let the patient smell it. By inhaling ethyl alcohol vapor for ten minutes, the patient will be able to hold out until the ambulance arrives. However, sometimes the reaction to alcohol vapor can be completely unexpected - instead of relief, the patient may feel that he does not have enough air. In this case, the tampon should be immediately removed from the nose.
Diagnostics
A doctor can determine the development of pulmonary edema by numerous external symptoms. In addition, the patient is prescribed instrumental and laboratory examinations. Among them:
- measurement of blood oxygen levels, determination of carbon dioxide content;
- blood chemistry;
- electrocardiogram and ultrasound of the heart;
- chest x-ray to evaluate the condition of the lungs.
Inserting a catheter into the pulmonary artery allows you to determine the type of edema: cardiogenic or non-cardiogenic.
If pulmonary edema is suspected, it is important to carry out the necessary tests and examinations as soon as possible, identify the cause and type of pathology, and begin treatment. Saving the patient's life directly depends on this.
Stages of the disease
The development of pulmonary edema in bedridden elderly people occurs in stages. The fluid accumulates gradually over some time, and the person becomes difficult to breathe. It is worth noting that there are different types of pathology, which depend on the cause that provoked pulmonary edema in older people. There are three stages of the disease. The difference between them is the rate at which swelling and symptoms develop. If swelling occurs very quickly, the patient’s symptomatic picture is clearly defined. Stage 1: lightning fast. The development of edema occurs at a rapid pace, unexpectedly for an elderly person. This situation has a negative effect on the blood vessels due to the fact that the patient experiences shock, the capillaries are injured, and the rate of growth of fluid and blood into the alveoli increases. Stage 2: acute. It develops over three to four hours. Symptoms of pulmonary edema in older people appear gradually, and the patient does not immediately pay attention to them. Stage 3: protracted.
In this case, the course of the disease is imperceptible. The elderly man does not realize that pulmonary edema has begun inside him. This stage is treatable. Read material on the topic: Diseases of the elderly
Treatment of pulmonary edema
People with acute respiratory failure are treated in the intensive care unit. First aid consists of measures that reduce venous return to the heart. To do this, the patient must take a semi-sitting position. Applying tourniquets to the limbs and hot foot baths have a positive effect.
It is imperative to monitor blood oxygen saturation levels. Oxygen therapy is used to compensate for its deficiency. If pulmonary edema has developed against the background of mechanical asphyxia, it is necessary to clear the airways of foreign objects. If it is impossible to breathe independently, the patient is connected to a ventilator.
A combination of medications is used to eliminate pulmonary edema. Among them:
- morphine and other narcotic analgesics;
- drugs to stimulate diuresis;
- nitroglycerine;
- drugs to lower blood pressure.
Depending on the underlying disease, patients with pulmonary edema are prescribed antihistamines, antibiotics, hormonal and antiarrhythmic drugs, and cardiac glycosides. The task of the resuscitator is to stop the attack and prevent acute hypoxia, which leads to cell death and death of the patient. After the symptoms of respiratory failure are relieved, treatment of the disease that caused it begins.
It is very important to eliminate the root cause that led to the clinical syndrome. Otherwise, a relapse of the disease is possible.
Publications in the media
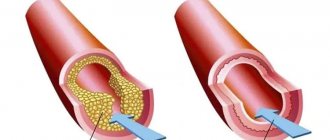
Pulmonary edema (PE) is the accumulation of fluid in the interstitial tissue and/or alveoli of the lungs as a result of extravasation of plasma from the vessels of the pulmonary circulation. Pulmonary edema is divided into interstitial and alveolar, which should be considered as two stages of one process • Interstitial pulmonary edema - edema of the interstitial tissue of the lungs without the release of transudate into the lumen of the alveoli. Clinically manifested by shortness of breath and cough without sputum. As the process progresses, alveolar edema occurs • Alveolar pulmonary edema is characterized by the leakage of blood plasma into the lumen of the alveoli. Patients develop a cough with foamy sputum, suffocation, and first dry and then moist rales are heard in the lungs.
The predominant age is over 40 years. Etiology • Cardiogenic OA with low cardiac output •• MI - large affected area, rupture of the heart walls, acute mitral regurgitation •• Decompensation of chronic heart failure - inadequate treatment, arrhythmias, severe concomitant disease, severe anemia •• Arrhythmias (supraventricular and ventricular tachycardia, bradycardia) •• Obstruction to blood flow - mitral or aortic stenosis, hypertrophic cardiomyopathy, tumors, blood clots •• Valvular insufficiency - mitral or aortic insufficiency •• Myocarditis •• Massive PE •• Pulmonary heart •• Hypertensive crisis •• Cardiac tamponade • • Cardiac trauma • Cardiogenic OB with high cardiac output •• Anemia •• Thyrotoxicosis •• Acute glomerulonephritis with arterial hypertension •• Arteriovenous fistula • Non-cardiogenic OB - see Adult respiratory distress syndrome.
Pathomorphology of cardiogenic OB • Intra-alveolar transudate of pink color • In the alveoli - microhemorrhages and hemosiderin-containing macrophages • Brown induration of the lungs, venous congestion • Hypostatic bronchopneumonia • At autopsy - heavy, enlarged lungs of pasty consistency, fluid drains from the cut surface. Clinical picture • Severe shortness of breath (dyspnea) and increased breathing (tachypnea), participation in the act of breathing of auxiliary muscles: inspiratory retraction of the intercostal spaces and supraclavicular fossa • Forced sitting position (orthopnea), anxiety, fear of death • Cyanotic cold skin, profuse sweating • Features of the clinical picture of interstitial OA (cardiac asthma) •• Noisy wheezing, difficulty breathing (stridor) •• Auscultation - against the background of weakened breathing, dry, sometimes scanty fine rales • Features of the clinical picture of alveolar OA •• Cough with discharge of foamy sputum, usually pink in color •• In severe cases - aperiodic Cheyne-Stokes breathing •• Auscultation - moist fine bubbling rales, initially arising in the lower parts of the lungs and gradually spreading to the apices of the lungs • Changes in the cardiovascular system •• Tachycardia •• Alternating pulse (inconstancy of the amplitude of the pulse wave) with severe left ventricular failure •• Pain in the heart area •• In the presence of heart defects - the presence of corresponding clinical symptoms.
Laboratory tests • Hypoxemia (the degree changes during oxygen therapy) • Hypocapnia (concomitant lung diseases may complicate interpretation) • Respiratory alkalosis • Changes depending on the nature of the pathology that caused OA (increased levels of MB-CPK, troponins T and I in MI, increased concentration thyroid hormones for thyrotoxicosis, etc.).
Special studies • ECG - possible signs of left ventricular hypertrophy • EchoCG is informative for heart defects • Insertion of a Swan-Ganz catheter into the pulmonary artery to determine pulmonary artery wedge pressure (PAWP), which helps in the differential diagnosis between cardiogenic and non-cardiogenic OA. PAWP <15 mmHg. characteristic of adult respiratory distress syndrome, and PAWP >25 mmHg. — for heart failure • Chest X-ray • Cardiogenic OB: expansion of the borders of the heart, redistribution of blood in the lungs, Kerley lines (linear striations due to increased image of the pulmonary interstitium) with interstitial OB or multiple small foci with alveolar OB, often pleural effusion •• Non-cardiogenic OB: the boundaries of the heart are not expanded, there is no redistribution of blood in the lungs, effusion into the pleural cavity is less pronounced.
Differential diagnosis • Pneumonia • Bronchial asthma • PE • Hyperventilation syndrome.
TREATMENT. Emergency measures • Place the patient in a sitting position with his legs down (reducing the venous return of blood to the heart, which reduces preload) • Adequate oxygenation using a mask with 100% oxygen supplied at a rate of 6–8 l/min (preferably with defoamers - ethyl alcohol, antifomsilan). With the progression of pulmonary edema (determined by the coverage of all pulmonary fields with moist coarse rales), intubation and mechanical ventilation under positive expiratory pressure are performed to increase intra-alveolar pressure and reduce extravasation • Administration of morphine in a dose of 2-5 mg IV to suppress excessive activity of the respiratory center • Administration of furosemide IV in a dose of 40–100 mg to reduce blood volume, dilate venous vessels, reduce venous return of blood to the heart • Administration of cardiotonic drugs (dobutamine, dopamine) to increase blood pressure (see Cardiogenic shock) • Reduction of afterload using sodium nitroprusside at a dose of 20–30 mcg/min (using a special dispenser) with systolic blood pressure more than 100 mm Hg. until pulmonary edema resolves. Instead of sodium nitroprusside, intravenous administration of nitroglycerin solution is possible • Use of aminophylline in a dose of 240–480 mg IV to reduce bronchoconstriction, increase renal blood flow, increase the excretion of sodium ions, increase myocardial contractility • Application of venous tourniquets (tourniquets) on the extremities to reduce venous return to the heart. Sphygmomanometer cuffs applied to three limbs, with the exception of the one where intravenous drugs are administered, can be used as venous tourniquets. The cuff is inflated to values intermediate between systolic and diastolic blood pressure, and the pressure in the cuff must be reduced every 10–20 minutes. Inflating the cuffs and reducing the pressure in them should be carried out sequentially on all three limbs • The advisability of prescribing cardiac glycosides is debated • If pulmonary edema occurs against the background of a hypertensive crisis, it is necessary to administer antihypertensive drugs • Non-cardiogenic edema - see Adult respiratory distress syndrome.
Additionally • Bed rest • Diet with a sharp restriction of table salt • Therapeutic bloodletting • Blood ultrafiltration (also to reduce blood volume) • Foam aspiration for alveolar OA. Complications • Ischemic lesions of internal organs • Pneumosclerosis, especially after non-cardiogenic OA. Prognosis • Depends on the underlying disease that caused AL • Mortality in cardiogenic AL is 15–20%. Age characteristics • Children: AL often occurs with malformations of the pulmonary system and heart or as a result of injuries • Elderly: AL is one of the most common causes of death.
Pregnancy • Timing of occurrence of OB: 24–36 weeks of pregnancy, during childbirth and in the early postpartum period • The method of delivery depends on the obstetric situation •• In the absence of conditions for vaginal delivery - cesarean section •• For vaginal delivery - application of obstetric forceps •• In the absence of conditions for application of forceps - craniotomy • Prevention of OA in pregnant women is important: timely resolution of the issue of the possibility of maintaining pregnancy, stabilization of heart pathology in pregnant women, dynamic monitoring of the state of the cardiovascular system.
Synonyms for cardiogenic OA: • Acute left ventricular failure • Cardiac asthma. Abbreviations • PH - pulmonary edema • PPA - pulmonary artery wedge pressure
ICD-10 • I50.1 Left ventricular failure • J81 Pulmonary edema.
Predictions and prevention
Pulmonary edema is a deadly condition; Mortality with this clinical syndrome is up to 50%. Patients with anaphylactic shock most often develop fulminant or acute pulmonary edema, which in more than 90% leads to death.
The consequences of acute pulmonary failure are no less serious than the disease itself. Many patients who have suffered pulmonary edema experience ischemic damage to internal organs, the appearance of areas of pneumosclerosis, and congestive pneumonia. This affects the functioning of the respiratory system, in the organs of which irreversible changes occur. The pathology is manifested by shortness of breath, chest pain, and cough. Pneumosclerosis and other consequences of pulmonary edema require long-term treatment, can lead to disability and shorten the patient's life expectancy.
The likelihood of a favorable prognosis and outcome of the disease with pulmonary edema increases if the diagnosis was made in a timely manner and doctors began to stop the attack at the initial stage.
How does the pathology progress?
The key stages of disease progression are:
- Increase in vascular pressure. With this phenomenon, the permeability of the capillary walls taking part in the pulmonary circulation suddenly decreases, resulting in the release of tissue into the lung cavity. The alveoli absorb fluid abundantly, losing the ability to participate in gas exchange. Because of this, older people with pulmonary edema feel suffocated, and their skin begins to turn blue.
- Gradual decrease in oncotic blood pressure.
- Loss of solidity of the alveolar-capillary membrane.
If there are any suspicious signs indicating an exacerbation of the pathology, you should consult a doctor.