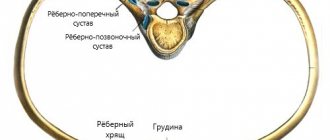
Tietze syndrome was first described by the German surgeon Alexander Tietze in 1921. Tietze syndrome usually affects the third, fourth, and fifth costochondral joints. Less commonly, the manubriosternal joint and the xiphoid joint are affected. The disease is characterized by chest pain (with coughing and deep breathing) and morning stiffness, as well as local swelling and hyperemia of the costal cartilages.
Joint swelling distinguishes Tietze's syndrome from costochondritis, or chronic inflammation of the cartilage of one or more ribs at the junction of the sternum and the ribs.
Characteristics/Clinical picture
The cartilage connects the sternum to the ribs and collarbone and allows the chest to move during breathing. Inflammation of the cartilage of one or more ribs causes swelling and redness of the skin. This is visible and tangible. The pain can vary in intensity, but is usually worse with trunk movements, coughing, deep breathing and straining.
Friends, very soon, as part of the RehabTeam project, Valentina Yudakova’s seminar “Thorax (Block 1)” will take place. Find out more...
These problems appear gradually and may disappear spontaneously after a few days, but sometimes they can take years to disappear. Even after spontaneous recovery, the disease may return, and pain may occur in the same or a different location. Pain syndrome can lead to disruption of normal movement in other joints, for example, shoulder movements can be accompanied by crepitus and pain. Patients with Tietze syndrome may experience a variety of functional limitations. Daily activities such as ironing, combing hair or lifting objects may be difficult.
Tietze syndrome - symptoms
The main symptom of TS is sharp, dull or aching pain in the chest. The pain usually occurs on only one side of the chest. If the disease affects multiple ribs, you may experience pain on both sides of the chest. In some cases, chest pain may spread to the neck, shoulders and arms.
The pain can range from mild to severe and may come on gradually or suddenly. Pain may worsen during the following activities:
- deep breathing
- cough
- sneezing
- exercises
- performing quick movements
Symptoms usually appear in patients under 40 years of age.
Differential diagnosis
Possible differential diagnoses are:
- Seronegative spondyloarthropathy.
- Rheumatoid arthritis.
- Xyphoidalgia.
- Slipping rib syndrome.
- Myelomalacia.
- Neoplasms of bones and soft tissues.
- Chondrosarcoma of the costochondral joints.
- Costochondritis.
- Tumors of the breast and/or lungs with extension to the costal cartilage.
- Metastases of neoplasms of the breast, kidneys and prostate gland.
- Rib injury and painful swelling of the ribs.
- Arthritis of the sternoclavicular and manubriosternal joints.
Symptoms
The main manifestation of Tietze's symptom is acute chest pain. It gradually increases and becomes more intense with deep breaths, sneezing, laughing, sudden movements, as well as with increased emotional and physical stress.
It is unilateral and often radiates to the arm on the corresponding side. Patients spare the affected side and try to close the sore spot. With this disease, there is no clear relationship between the occurrence of an attack of pain and the time of day. In some cases, the pain becomes so severe that patients cannot lie on their side; any movement brings them agony and suffering. Crepitation appears at the lesion site. The costal cartilage is hypertrophied and unusually curved. No histochemical changes are found in it. The surrounding soft tissues are swollen and inflamed.
Outwardly, the disease manifests itself sluggishly. Irregular acute attacks of pain can last several days, months, years. Pain is often combined with hypersensitivity of the xiphoid process. Palpation reveals a dense and clear spindle-shaped swelling. If you press on the junction of the ribs and sternum, noticeable pain appears. Discomfort and chest pain go away on their own and do not require specific treatment. The syndrome does not pose a threat to the life and health of the patient.
Secondary signs of pathology include:
- Violation of the depth, frequency and rhythm of breathing,
- Lack of appetite,
- Cardiopalmus,
- Insomnia,
- Local hyperthermia, hyperemia and swelling,
- Unmotivated fear, irritability and anxiety.
Residual signs of pathology occur extremely rarely.
Usually the general condition of patients is not disturbed and remains satisfactory. The muscles of the shoulder girdle and neck contract tonically. The skin over the affected area does not change, regional lymph nodes do not enlarge. As Tietze syndrome progresses, excessive calcification of cartilage develops, which is eventually replaced by bone tissue. As a result of fibrous metaplasia, the costal cartilages become deformed and lose their functions. The pain becomes intense and constant. A dense swelling on the chest interferes with the patient’s normal life. A rigid chest disrupts the normal breathing process, resulting in respiratory failure.
Diagnostic procedures
Appropriate studies such as electrocardiography (ECG) and computed tomography (CT) are necessary. They are used to rule out other diseases. Research suggests that this diagnosis is a diagnosis of exclusion. Plain radiographs are often normal/non-diagnostic. CT may reveal sclerosis of the sternum, partial calcification of the costal cartilage, and soft tissue edema. A costal cartilage biopsy may show chronic inflammation with fibrosis and ossification. Gallium scans have been reported to show increased uptake, similar to costochondritis.
Rating scales
- Visual analogue scale (VAS).
- Digital pain rating scale.
- McGill Pain Questionnaire (short form).
How the disease develops
Rett syndrome in children is a rather insidious disease. At birth, it practically does not manifest itself. Its first symptoms appear within 6 months. up to one and a half years. However, there are still some barely noticeable signs in the first half of the year. But they are so insignificant that they do not attract attention.
This is what the mother of one of the girls with the syndrome says about the first half of her life. She attached importance to these little things only after 1 year and 7 months had passed since the birth of her daughter, when the manifestations had already become obvious. Among the harbingers of the disease, she noted that her baby began to hold her head at 3 months, and not at 2, as expected. At 6 months she could not sit yet, and she began to walk only at 1 year and 4 months. She developed normally psychologically, and began to speak early, but these were not the standard words “mom”, “dad”, but “bunny”, “bear”, etc.
At 1 year and 7 months. she stopped recognizing her parents and did not seem to need them. I spent the whole day doing one monotonous activity: throwing a ball or pushing a stroller. She walked in circles for hours until she was stopped or she stammered. This stereotypical behavior is called field behavior, when the action drags on the patient and he cannot do anything.
At the age of four, epileptoid seizures joined the symptoms. However, upon reaching school age, the girl was home-schooled and made some progress.
12–6 years – this was a period of remission, when the disease practically did not bother me. But from the age of 16, new, deeper problems appeared related to bone deformations and diseases of the internal organs. One of the girl’s legs was almost 10 cm shorter than the other, which could not but interfere with walking. At 20 years old, she weighed only 24 kg and was 158 cm tall.
Typically, SR occurs in 4 stages.
The first stage , which, as a rule, starts from 6 months to one and a half years, is manifested by an increase in irritability and lability of mood in the child. Episodes of crying and psychomotor agitation are replaced by increasing passivity. The baby moves aimlessly around the room and loses interest in toys. But contact with the mother remains.
This is how a woman describes her daughter’s behavior at the beginning of the disease: she screamed all day long without stopping, banged her head against the walls, and could not sleep. No matter what we did, she did not calm down. It was real hell. But what was more depressing was that not a single doctor could make a clear diagnosis.
A disproportion of the head and limbs in relation to the body develops. They become disproportionately small. Growth slows and muscle tone decreases.
The second stage , which lasts several years, is characterized by a variety of symptoms. A decrease in intellectual abilities immediately attracts attention, and mental dementia develops. Almost all acquired skills regress. Speech completely disappears or progresses to the level of echolalia - mechanical repetition of what was heard.
Acquired motor skills and object-role behavior are lost and replaced by motor stereotypes. A characteristic symptom: numerous repetitive movements reminiscent of hand washing. In addition, the child constantly wrings or rubs them, waves them, and claps his hands. Clenching of the fingers is quite normal at 4 months, but at a later age it indicates a stoppage of development. The baby loses his grasp reflex and is unable to make rotational movements with his hands.
Gradually, physical activity fades away. The gait is disturbed, the child walks without bending his knees.
The third stage lasts 10 years or more, and is characterized by the development of persistent, profound dementia, even idiocy. There is a complete loss of the ability to speak and understand speech addressed to the child. A tremor of the whole body appears, aggravating movements. Convulsive seizures intensify.
The fourth, final stage is a period of worsening of previously manifested symptoms. Persistent loss of mental abilities, motor skills, development of muscular dystrophies leading to complete immobility.
The life expectancy of such patients on average ranges up to 30 years, although there are cases when they lived up to 50 years of age.
Inspection
On physical examination, swelling of the affected area and sometimes hyperemia is noted. Pain may occur during palpation of this area; The pectoralis major and minor muscles and the sternum are also painful.
The pain can be reproduced with retraction, protraction, or elevation of the shoulder or with deep inspiration. Tietze syndrome results in limited muscle strength and range of motion in the upper extremities. In such patients, the level of functional activity may decrease. Typically, difficulties arise when ironing, lifting objects, or combing hair, but the disruption in functionality is minor.
As said above, if there is inflammation of the cartilage of one or more ribs, then you can talk about costochondritis, if there is also swelling/redness that is very painful, then you can talk about Tietze's syndrome.
Etiology
Currently, the etiopathogenetic factors of Tietze syndrome remain unknown. Several theories of the occurrence and development of the disease have been developed. The main ones:
The traumatic or mechanical theory explains the occurrence of the disease in athletes, people engaged in heavy physical labor, or those who have suffered traumatic damage to the ribs in the past. Direct trauma to the shoulder results in damage to the costal cartilage. This irritates the perichondrium and disrupts further differentiation of cartilage cells. As a result of such changes, pathological cartilage tissue is formed, which compresses the nerve fibers, which is manifested by pain. The traumatic theory is considered the most popular.
According to the infectious theory, Tietze syndrome develops after suffering an acute respiratory infection, which provoked a decrease in the general resistance of the body.
Dystrophic theory - the development of pathology occurs as a result of calcium metabolism disorders and deficiency of vitamins C and B. This is one of the earliest theories developed by Tietze himself. It is not confirmed by objective data and is considered doubtful.
Factors contributing to the development of pathology:
- Pronounced and regular loads on the shoulders and chest,
- Chronic chest injuries in athletes,
- Acute infections
- Arthrosis-arthritis,
- Bronchopulmonary pathology,
- Occupational scoliosis,
- Metabolic disorders
- Endocrinopathies,
- Allergic reactions,
- Postmenopausal osteoporosis,
- Collagenoses.
The risk group includes:
- Athletes,
- Persons engaged in heavy physical labor
- Drug addicts,
- Persons after thoracotomy.
At the junction of the cartilages of the ribs and sternum, metabolic processes are disrupted. Prolonged aseptic inflammation leads to dystrophy, the appearance of areas of sequestration in the cartilage, metaplasia of cartilage tissue, its calcification and sclerosis. Benign reversible swelling of the costal cartilages causes pain. Degenerative changes lead to deformation of the cartilage, a decrease in its size, and weak intractability. As a result of ossification of the cartilage, the configuration of the chest changes, its mobility and elasticity decrease, and it becomes rigid.
Treatment
Drug treatment includes relative rest for 4-6 weeks, injections of a corticosteroid anesthetic, topical or oral analgesics, and other drugs, including Sulfasalazine or Caspofungin in combination with Fluconazole.
Physical therapy
Currently, there are no reliable clinical studies on the treatment of this disease. Treatment of Tietze syndrome is mainly symptomatic.
What can be done?
- Reassure the patient by explaining what is happening to him.
- It is important for the physical therapist to educate the person about proper body positioning while sitting or performing daily activities. It is also important that the patient avoids repetitive movements/activities. In general, these patients need a good balance between exercise and rest.
- The treatment program may include exercises to increase range of motion. Typically, patients tolerate such exercises well, but if they aggravate symptoms, then they should be abandoned or postponed.
- Stretching the pectoralis major muscle is helpful. You can stretch the pectoralis major muscle by standing in a doorway with emphasis on your forearms. You need to repeat this exercise several times a day for 1 or 2 minutes.
- Use hot/cold compresses and massage to reduce pain and symptoms of muscle overuse. For this purpose, you can also use a variety of sprays.
- Mobilizations of the spine and ribs are also helpful. This will help to avoid chest stiffness and reduce complaints.
- It is important to teach the patient breathing exercises and methods of working with pain.
- Exercises for the shoulder girdle and back can be provocative, so they should only be prescribed if symptoms disappear.
- Transcutaneous electrical stimulation and electroacupuncture can be used. In the latter case, an acupuncture needle is placed into the affected segment of the spine.
- Injection therapy with local anesthetics or corticosteroids has previously been described as a treatment for chest pain associated with costochondral joint lesions. Results from previous studies have shown that dry needling may be as effective as injection therapy in treating similar conditions.
Causes
Costochondritis is an inflammatory process in cartilage tissue, usually without any specific cause. Repeated minor injuries to the chest and acute respiratory infections can cause pain in the area where the ribs are attached (the impact of both the viruses themselves and frequent coughing on the area where the ribs are attached). Sometimes costochondritis occurs in people taking parenteral drugs or after surgery on the chest. After surgery, damaged cartilage tissue is more susceptible to infection due to impaired blood supply.