Gastrointestinal bleeding is the loss of blood from damaged blood vessels in or near the walls of the digestive tract when bleeding occurs into the lumen of the gastrointestinal tract. The source of bleeding can be any part of the digestive tract, from the pharynx to the rectum.
Bleeding can have many different causes and clinical progression depending on the rate and amount of blood lost, as well as the general condition, especially concomitant diseases.
Types of gastrointestinal bleeding
The content of the article
The severity of bleeding can range from microscopic blood loss to massive bleeding with the release of large amounts of blood (usually a mixture of blood, clots, and possibly hematin) through the mouth or anus, which can lead to hypovolemic shock and death.
Microscopic blood loss can only be detected in stool using specialized laboratory tests. The condition can also be identified by the results of peripheral blood tests and decreased iron levels.
Gastrointestinal bleeding is divided into:
- Bleeding from the upper gastrointestinal tract
. Their source is between the pharynx and the ligament of Treitz (duodenal ligament). They are involved in 80% of cases of gastrointestinal bleeding; - Gastrointestinal bleeding from the lower gastrointestinal tract
. Their source is between the ligament of Treitz and the rectum; - Hidden gastrointestinal bleeding
. This form differs from ordinary bleeding in its clinical picture and requires specific diagnostic procedures.
How to competently provide first aid for severe capillary bleeding?
First aid for capillary bleeding involves applying a tourniquet. The indication is extensive damage, impaired coagulation. Rules for applying a tourniquet:
- Wrap the tourniquet 2 times around the injured limb above the wound. Correct actions lead to the fact that the pulse under the wound will not be palpable.
- Place a piece of fabric under the tourniquet to avoid trophic changes.
- Be sure to record the exact time of application of the tourniquet. The skin condition is monitored.
- In the warm season, you can leave the tourniquet on the body for up to 2 hours, in winter - no more than 1 hour. Every 30 minutes you need to relax the rubber band for 30 seconds to avoid tissue death. If everything is done correctly, the limb does not turn blue or swell. And vice versa.
After applying a rubber tourniquet, the victim is quickly sent to the hospital for diagnosis and treatment. If you don’t have a rubber band at hand, use a belt, scarf, or tie.
Symptoms of upper gastrointestinal bleeding
Such bleeding can be identified by specific symptoms. The patient is concerned about:
- Vomiting and tarry stools;
- Fusion vomiting - vomiting of blood (hematemesis) with an admixture of hematin, formed by the action of hydrochloric acid on hemoglobin;
- Vomiting “coffee grounds.” It is black or brown in color due to the presence of hematin. With light bleeding, “coffee grounds” may not appear, and then the only sign is tarry stool.
During intense bleeding from the upper gastrointestinal tract, vomiting blood may be accompanied by loose, bloody stools. Information about the appearance of stool can be obtained from anamnesis or rectal examination. It should be borne in mind that there are medications that can cause stools to turn black, for example, iron or bismuth salts.
Determining the cause and assessing the intensity of bleeding
Often the probable cause of bleeding can be determined by history.
Important things to consider:
- symptoms of dyspepsia (especially at night);
- symptoms of stomach ulcer;
- side effects of medications taken, especially those that inhibit blood clotting, such as non-steroidal anti-inflammatory drugs;
- likelihood of alcohol abuse;
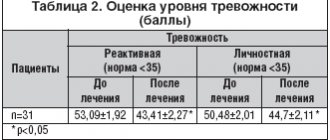
- the presence of hepatitis B or C - these may indicate liver cirrhosis and portal hypertension as possible causes of bleeding.
Physical examination
Physical examination
The gastroenterologist begins the examination from the head - carefully examining the nose, mouth and throat, since sometimes the cause of bleeding can be localized.
Next, they are identified with
symptoms of anemia and hypovolemia. The patient's heart rate and blood pressure are determined. A bad symptom is an acceleration of heart rate and a drop in blood pressure (>10 mmHg). Orthostatic hypotension involves rapid or severe blood loss.
Other signs that may indicate significant blood loss include:
- cool skin;
- oliguria;
- disturbances of consciousness.
Patients with anemia feel weak, dizzy, see spots before their eyes, have chest pain, and may faint. The severity of these symptoms depends on the amount of blood lost and the rate of bleeding.
It is also important to carefully examine the patient's body for symptoms of chronic liver disease. A number of specific symptoms indicate a pathological condition of the liver:
- presence of spider veins on the skin of the breast
- gynecomastia;
- loss of axillary and pubic hair;
- yellowing of the skin;
- palmar erythema;
- enlarged spleen;
- ascites;
- swelling of the legs;
- hand tremors
Further treatment
Combined methods are mainly used.
First of all, it is necessary to eradicate the source of the disorder. This problem is solved by surgical intervention methods.
The vessel and tissues are sutured, and the damaged area is eliminated (if necessary, doctors perform a resection and remove part of the altered structures). Mandatory measures are also taken regarding the consequences of the pathological process.
In parallel, transfusion is necessary to restore lost blood volume and the introduction of saline solutions to correct the balance of electrolytes. The patient's condition is constantly monitored in a hospital setting.
Symptoms of neoplasms
Advanced neoplastic diseases are indicated by:
- underweight;
- enlarged, hard liver with a lumpy structure;
- palpable tumor in the abdominal cavity;
- enlarged and hard lymph nodes.
Other symptoms:
- Subcutaneous emphysema in a patient with persistent vomiting indicates Boerhaave syndrome (esophageal perforation). A prompt consultation with a surgeon is necessary.
- Telangiectasia on the mucous membranes may indicate Randu-Osler-Weber disease.
Sigmoidoscopy (rectoscopy)
If necessary, an examination of the rectum is performed. Sigmoidoscopy (rectoscopy) is a method of endoscopic examination of the rectum and distal sigmoid colon by examining their internal surface using a sigmoidoscope inserted through the anus.
Sigmoidoscopy is the most accurate and reliable examination of the rectum and lower sigmoid colon. In the practice of a coloproctologist, sigmoidoscopy is an obligatory component of every proctological examination. The examination allows you to visually assess the internal surface of the rectum and distal third of the sigmoid colon to a level of 20-35 cm from the anus.
Bleeding from the lower digestive tract
Bleeding from the lower gastrointestinal tract accounts for approximately 20% of cases of gastrointestinal bleeding. The main symptom is chestnut or burgundy stool mixed with fresh blood (hematochezia).
The appearance of blood in the stool can indicate where the source of the bleeding is, namely:
- The presence of bright red blood in the stool indicates bleeding in the left side of the colon (up to the flexure of the spleen) or in the rectum;
- If there is bleeding in the right side of the colon, the blood is dark in color and may be mixed with the stool;
- Blood from the rectum may also be clear if it passes quickly from the right side of the colon or if there is a lot of bleeding from the upper gastrointestinal tract. In approximately 13% of patients with fresh blood in the stool, the source of bleeding is in the upper gastrointestinal tract;
- In the case of tarry stools, the most common source of bleeding is the upper gastrointestinal tract. The stool may be the same color if the source of bleeding is the cecum.
What is the main danger of capillary bleeding?
First aid for capillary bleeding should not be called an unnecessary procedure. Compared to arterial and venous bleeding, capillary bleeding is not so dangerous, and in most cases the body copes with it on its own. But there are situations that are life-threatening:
- the skin is extensively damaged;
- the ambient temperature is increased;
- blood clotting is impaired;
- There is blood poisoning, oncology, hepatitis, arterial hypertension and other severe pathologies.
The most dangerous is bleeding as a result of damage to the blood vessels of internal organs. Prolonged bleeding provokes a decrease in blood pressure, oxygen starvation, and disruption of the cardiovascular system. If the blood loss is severe, the person dies without treatment. Hemorrhage in the brain affects important centers and also leads to a fatal outcome. Pleural bleeding disrupts breathing and puts pressure on the lung. In most cases, it is important to react in time to manifestations of capillary bleeding and provide first aid in a timely manner.
Determining the cause and assessing the intensity of bleeding from the lower gastrointestinal tract
Determining the cause and assessing the intensity of bleeding from the lower gastrointestinal tract
Sometimes bleeding from the upper gastrointestinal tract occurs without vomiting with bloody or soil-like contents, but with the removal of bloody contents through the anus.
It is important to consider the patient's age. For example, symptoms of bleeding from the lower gastrointestinal tract in a young person, with abdominal pain and diarrhea, may indicate inflammatory bowel disease. Similar symptoms in an elderly person indicate intestinal ischemia.
Streaks or spots of blood on the surface of the stool, pain in the anal area, and drops of blood on toilet paper or in the toilet indicate an anal fissure or bleeding from the rectum, such as hemorrhoids.
During the physical examination, the doctor pays special attention to symptoms indicating bleeding from the upper gastrointestinal tract and carefully examines the perineum and anal canal (rectally).
Forecast
Controversial. Depends on the situation. There are two main factors. This is the degree of the disorder (its severity), as well as the moment of initiation of therapy. With timely treatment, if the disorder is relatively harmless, there is every chance of full recovery.
Internal bleeding is a life-threatening process that is not always obvious at first glance. Without proper correction, it is often fatal.
Specialists eliminate the causes of the anomaly using surgical methods. Medication methods are also used. The forecasts remain vague. When assessing prospects, you need to proceed from the situation.
Hidden and unexplained gastrointestinal bleeding - classification, causes
In 2007, the American Gastroenterological Association proposed the following nomenclature for conditions associated with chronic gastrointestinal blood loss:
- Hidden bleeding
. This is the most common cause of iron deficiency. In men, it most often occurs in the gastrointestinal tract. In women, menstruation should be taken into account; - Vague bleeding
. It is recurrent or constant bleeding in the gastrointestinal tract, the cause of which cannot be determined despite endoscopic and radiological studies involving the entire gastrointestinal tract. This type of bleeding is divided into obvious and hidden.
The causes of hidden gastrointestinal bleeding are varied. The most common:
- colon cancer;
- esophagitis;
- inflammation or ulceration of the mucous membrane of the stomach or duodenum;
- intestinal inflammation;
- angiectasia;
- hypertensive portal gastropathy;
- diverticula;
- celiac disease.
Less common reasons include:
- esophageal carcinoma;
- stomach cancer;
- bleeding from the bile ducts or pancreatic ducts;
- aorto-intestinal fistulas;
- endometriosis;
- gastrointestinal infections.
Tests for latent blood in the stool may test positive for hemoptysis or nosebleeds.
It is not recommended to collect samples during digital rectal examination, as it may cause microtrauma and give a false-positive result.
Causes of pathology
Most often, patients seek help in this condition, after receiving injuries to the chest, abdominal cavity, when there is a fracture of the limbs, ribs and pelvic bones. This also leads to damage to some organs, for example, the spleen and liver. So, after a fall from a hill or an accident, damage to the intestines and mesentery is diagnosed, and the result of a traumatic brain injury can be bleeding in the cranial cavity. In the latter case, even a small amount of blood fluid puts pressure on the brain and poses a threat. It is necessary to clarify that this condition may not occur immediately, but after a couple of hours or even days, sometimes this happens even when the patient is feeling well. This problem can be caused by the following diseases that occur in acute or chronic form:
- Tuberculosis. Leads to pulmonary hemorrhages.
- Ulcers. They can damage blood vessels, resulting in blood in the intestines, peritoneum, and duodenum.
- Cirrhosis. Promotes hemorrhage from varicose veins located in the esophagus.
- Malignant tumors formed in the intestines and stomach. Their breakdown sometimes causes blood loss.
- Aortic aneurysm dissection. This is not a rare cause of such ailment in elderly patients.
- Gynecological pathologies.
- Mallory-Weiss syndrome. There are cracks in the esophagus, which have caused frequent drinking or overeating.
The list continues with physical activity and poor diet.
Peroxidase test to confirm the presence of guaiacol
This is the most commonly used stool blood test. The test available is called Hemoccult. In this study, a stool sample is distributed into a guaiacol-impregnated cardboard box, which, if the stool contains heme, turns blue (heme causes a reaction similar to peroxidase). The more blood in the stool, the higher the likelihood of a positive result.
The Hemoccult test gives a positive result in 50% of cases when 10 ml of blood enters the gastrointestinal tract during the day. Under physiological conditions, 0.5-1.5 ml of blood is normally extravasated into the lumen of the gastrointestinal tract during the day.
The sensitivity of the first test is estimated to be approximately 30%. Performing 3 tests (which is the standard) increases the confidence to 92%. False negative results are especially common in people taking medications or foods high in vitamin C.
Relatively often, the test gives false positive results when consuming large amounts of red meat and foods high in peroxidase (radish, radish, horseradish). Taking iron supplements does not give false positive results in the study.
Immunochemical tests
Immunochemical tests
Immunochemical tests (HemeSelect, FECA, I-FOBT and Hemoccult ICT), used within European standards, detect undenatured human hemoglobin and give a positive result when it enters the gastrointestinal tract in an amount of 0.3 ml/24 hours.
These tests are not positive if the source of the bleeding is found in the upper gastrointestinal tract—hemoglobin from this source is denatured and degraded before it reaches the stool.
Prohibited actions
What you should absolutely not do:
- Give enemas.
- Give any medications. It is not safe. The use of medications is impossible; a sharp deterioration in the condition is likely.
- Under no circumstances should you heat the affected area. This will lead to the dilation of blood vessels and will cause a sharp increase in the intensity of the outpouring of liquid connective tissue.
- Also, you should not move the patient again, so as not to provoke increased bleeding.
Attention:
Self-action in such a serious situation is the best way to ensure death for the patient. Everything must be within the minimums described above.
Determining the cause of bleeding - endoscopic and radiological methods
A history and physical examination are performed by a gastroenterologist in accordance with the principles of treatment when analyzing bleeding from the upper or lower gastrointestinal tract.
Further tests for a patient who tests positive for blood in the stool include:
- Peripheral blood test - looking for signs of anemia;
- Endoscopic examinations of the gastrointestinal tract - esophagogastroduodenoscopy and colonoscopy. These tests help identify the possible source of bleeding. Colonoscopy may be considered sufficient in the absence of anemia or gastrointestinal symptoms.
Enteroscopy offers great diagnostic and therapeutic options in case of suspicious changes in the small intestine.
When endoscopic examinations do not help determine the source of bleeding, X-ray examination
small intestine with evaluation of the fragment and possibly enteroclysis.
In difficult cases, CT or MRI enterography and endoscopic examination are performed using a special capsule with a built-in video camera, which the patient swallows like a regular pill.
Pathologies that rarely cause bleeding
A positive stool blood test should not be associated with pathologies of the gastrointestinal tract, which rarely cause hidden bleeding, namely:
- varicose veins of the esophagus;
- diverticulosis of the large intestine.
In the vast majority of these cases, bleeding is obvious. An exception is the disease of varicose veins of the esophagus, after endoscopic therapy or sclerotherapy procedures. The discovery of such changes in a patient with a positive test result does not exempt him from performing gastrointestinal studies.
Diverticula in the colon produce symptoms in people of the same age similar to organ cancer, which often causes hidden bleeding.
Reasons for false test results
- Anticoagulant treatment. A positive test result for the presence of latent exudate in the stool cannot be taken into account in patients taking medications that suppress blood clotting (acetylsalicylic acid, clopidogrel, acenocoumarol, warfarin, heparins). Also, taking such drugs does not eliminate the need to look for the cause of blood in the stool. Taking acetylsalicylic acid at a dose of 300 mg/24 hours. slightly increases the amount of blood passing into the stool. Neither aspirin nor warfarin interferes with fecal tests;
- Alcohol abuse. Hidden blood in the stool has nothing to do with alcohol consumption. But alcohol abuse increases the risk of developing peptic ulcers and gastrointestinal cancer;
- Menstruation. The most common cause of iron deficiency and anemia in premenopausal women is menstruation. However, when abdominal symptoms coexist, women over 40 years of age may be diagnosed with gastrointestinal cancer. A positive stool blood test requires diagnosis of sources of bleeding.
Antisecretory therapy
Optimal conditions for the implementation of vascular-platelet and hemocoagulation components of hemostasis are created at pH > 4.0. Proton pump inhibitors and H2-histamine receptor blockers are used as antisecretory drugs.
Attention! It is not advisable to prescribe H2-histamine receptor blockers and proton pump inhibitors at the same time.
Medicines of both groups suppress the production of hydrochloric acid in the stomach and thereby create conditions for stable hemostasis of the bleeding vessel. But proton pump inhibitors show more consistent results in reducing gastric acidity and are significantly more effective in reducing the risk of recurrent bleeding. The antisecretory effect of proton pump inhibitors is dose-dependent. Therefore, the use of high doses of drugs is currently recommended, so the prescription regimens indicated below are not a typo by the author.
Patients are prescribed an intravenous infusion of one of the following proton pump inhibitors:
- Omeprazole (Losec) 80 mg IV as a loading dose, followed by 8 mg/hour.
- Pantoprazole (Controloc) 80 mg IV as a loading dose, followed by 8 mg/hour.
- Esomeprazole (Nexium) 80 mg IV as a loading dose, followed by 8 mg/hour.
The loading dose of the drug is administered in approximately half an hour. Intravenous administration of the drug is continued for 48-72 hours, using, depending on possibilities, a bolus or continuous route of administration. In the following days, they switch to oral administration of the drug at a daily dose of 40 mg (for all of the proton pump inhibitors listed in this paragraph). The approximate duration of the course is 4 weeks.
Attention. The administration of proton pump inhibitors should be started before endoscopic intervention, as this reduces the likelihood of recurrent bleeding.
In the absence of proton pump inhibitors, or patients intolerant of them, intravenous H2-histamine receptor blockers are prescribed:
- Ranitidine 50 mg IV every 6 hours or 50 mg IV followed by 6.25 mg/hour IV. After three days, 150-300 mg orally 2-3 times a day;
- Famotidine 20 mg IV drip every 12 hours. Orally for treatment use 10-20 mg 2 times/day or 40 mg 1 time/day.
Diagnosis of gastrointestinal bleeding - tests
Diagnosis of gastrointestinal bleeding - tests
First of all, the gastroenterologist needs to detect the source of bleeding. It must be looked for using: endoscopic, x-ray and scintigraphic studies.
- Morphology of peripheral blood.
The analysis is necessary to assess blood loss. Comparing the current result with previous ones helps with this. On the first day of bleeding, analysis should be done every 4-6 hours. In the first few hours of acute bleeding, hemoglobin levels and hematocrit may not change significantly (due to compensatory mechanisms). In addition to the loss of red blood cells, elevated white blood cell and platelet counts are common in this diagnosis, and from days 3 to 7, the reticulocyte count begins to increase (however, this does not occur in people with significant iron deficiency); - Urea concentration and assessment of renal function.
Blood urea levels may rise slightly if there is heavy bleeding from the upper gastrointestinal tract because the protein-containing blood becomes a source of ammonia and urea. In this regard, the patient may have concurrent chronic kidney disease, which increases the risk of death. Acute prerenal kidney injury may be a symptom of hemorrhagic shock; - Liver markers
. Serum transaminase and bilirubin activities help assess the coexistence of liver disease; - Markers of thyroid diseases
. Measuring serum calcium levels can identify hyperparathyroidism, which contributes to the development of gastric and duodenal ulcers; - Assessment of blood clotting.
Tests that evaluate the efficiency of the blood coagulation system—prothrombin time (PT) and activated partial thromboplastin time (aPTT)—are important.
The problem occurs in patients taking warfarin or acenocoumarol. It should be assessed whether continuation of treatment, which makes it difficult to control bleeding, or discontinuation of treatment due to the risk of thromboembolic complications, would be more life-threatening. In such a situation, oral drugs are replaced with short-acting low-molecular-weight heparin drugs.
If generalized intravascular coagulation syndrome is suspected, the concentration of D-dimer, fibrinogen and platelet count should be determined.
When a blood transfusion is necessary, the blood type should be determined and cross-matched.
Diagnostics
Laboratory diagnostics
1. Complete blood count - depending on the duration of the bleeding, the blood picture may vary. In the acute phase, a decrease in the level of red blood cells, hemoglobin and the liquid part of the blood (plasma) is observed; the hematocrit “Ht” during acute bleeding remains unchanged, since plasma and formed elements are lost equally. With chronic minor bleeding, a decrease in the level of red blood cells and hemoglobin is also found, “Ht” in this case is reduced, there is an increase in the level of reticulocytes (immature red blood cells) - this is a compensation reaction, replenishing the number of red blood cells. An advanced analysis with determination of platelet levels is necessary for diagnosing thrombocytopenia (possible with various diseases of internal organs, poor nutrition, genetic pathologies).
2. General urine test - necessary to assess the functional ability of the kidneys to secrete urine. With significant blood loss, diuresis may be reduced and even absent altogether (anuria in hemorrhagic shock).
3. Biochemical blood test - determination of the concentration of bilirubin, urea, creatinine, total protein, LDH (lactate dehydrogenase), cholesterol, blood glucose, etc. All these studies are necessary for a thorough differential diagnosis.
4. Determination of blood group and Rh factor - necessary for possible blood transfusion.
5. Coagulogram - analysis of the function of the cascade protein blood coagulation system (prothrombin index, prothrombin time, level of fibrinogen, antithrombin III, D-dimer, etc.).
Instrumental diagnostics
1. X-ray of the abdominal organs and chest cavity - allows you to determine the presence of fluid accumulation in the cavities, displacement of organs, defects of large vessels. Additionally, special contrast agents (for example, barium sulfate) can be used.
2. Ultrasound examination (ultrasound) - used for primary and differential diagnosis of bleeding with other pathologies (cysts, tumors).
3. Computed tomography (CT) - used when the primary diagnosis is questionable. The essence of the method is to obtain a layer-by-layer image of tissues and organs using x-rays.
4. Magnetic resonance imaging is a safe and informative diagnostic method. Used when other graphical research methods are ineffective. Allows you to identify the smallest and “hidden” hematomas.
5. Diagnostic laparoscopy is a method of visualizing the contents of the abdominal cavity by puncturing the abdominal wall with the introduction of a tube with a video camera.
6. Diagnostic laparatomy - an incision is made in the anterior abdominal wall from the xiphoid process to the symphysis pubis (to the extent necessary for diagnosis). The doctor examines the organs and makes a final diagnosis.