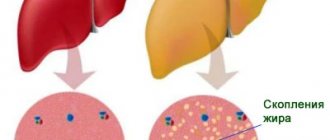
Fatty liver hepatosis (steatosis) is a primary or secondary pathological syndrome that occupies a leading position in the general structure of hepatopathologies. The main reason for the development of this condition is a metabolic disorder, leading to excessive accumulation of lipids and subsequent degeneration of hepatic parenchyma cells.
Causes of fatty hepatosis
There are three main reasons for the development of hepatic steatosis:
- Obesity. If the body mass index exceeds 30, the likelihood of dystrophy is about 40%.
- Drinking alcoholic beverages. Moreover, hepatosis can occur even in people who drink a little, but every day. There is a direct relationship between the duration of alcohol consumption and the severity of liver dystrophy and, as a consequence, the risk of developing cirrhosis.
- Long-term use of medications with hepatotoxic effects.
Less commonly, hepatosis develops against the background of diseases that occur with metabolic disorders; this category includes hyperlipidemia, hypercholesterolemia, diabetes mellitus, thyrotoxicosis, myxedema, Itsenko-Cushing syndrome, malignant neoplasms, chronic diseases of the gastrointestinal tract, in which the absorption process is disrupted, etc. .
Liver dystrophy can be caused not only by obesity, but also by poor nutrition - overeating, abuse of fatty foods and foods containing hydrogenated fats and simple carbohydrates.
The disease is sometimes diagnosed in people who have a deficiency of enzymes involved in lipid metabolism (hereditary disease).
Most often, more than one factor leads to the development of steatosis. In most cases, there is a multifactorial factor, for example, the consumption of alcohol by a person who is eating poorly or taking toxic medications.
Fully or partially limited products
The diet for liver hepatosis includes the following exceptions:
- Broths based on meat/fish and mushrooms, as well as first courses based on them.
- Fatty meat and fatty varieties of sea/river fish, meat of domestic waterfowl (goose and duck), smoked meats, sausages, salted fish.
- Products containing flavoring additives, preservatives, confectionery products with a long shelf life, freeze-dried products.
- Offal (liver, kidneys, brains), cooking/animal fat.
- Legumes and vegetables containing coarse fiber (radish, radish, turnip, white cabbage).
- Products rich in oxalic acid/essential oils (sour sauerkraut, sorrel, garlic, onion, spinach).
- Fried/hard-boiled eggs.
- Hot spices/herbs (horseradish, pepper, mayonnaise, mustard, ketchup).
- Heavy cream/milk, full-fat cottage cheese, chocolate, cakes, cheese curds, puff pastry, coffee, cocoa, cakes, muffins.
- Sour berries/fruits.
- Alcohol-containing and carbonated sweet drinks, and mineral waters.
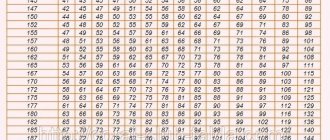
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| canned vegetables | 1,5 | 0,2 | 5,5 | 30 |
| eggplant | 1,2 | 0,1 | 4,5 | 24 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| peas | 6,0 | 0,0 | 9,0 | 60 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| chickpeas | 19,0 | 6,0 | 61,0 | 364 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| parsley | 3,7 | 0,4 | 7,6 | 47 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| iceberg lettuce | 0,9 | 0,1 | 1,8 | 14 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| dill | 2,5 | 0,5 | 6,3 | 38 |
| beans | 7,8 | 0,5 | 21,5 | 123 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
| marinated mushrooms | 2,2 | 0,4 | 0,0 | 20 |
Nuts and dried fruits | ||||
| nuts | 15,0 | 40,0 | 20,0 | 500 |
| peanut | 26,3 | 45,2 | 9,9 | 551 |
| seeds | 22,6 | 49,4 | 4,1 | 567 |
Cereals and porridges | ||||
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
| dumplings | 11,9 | 12,4 | 29,0 | 275 |
Bakery products | ||||
| buns | 7,9 | 9,4 | 55,5 | 339 |
| Rye bread | 6,6 | 1,2 | 34,2 | 165 |
Confectionery | ||||
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
| shortbread dough | 6,5 | 21,6 | 49,9 | 403 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
Dairy | ||||
| milk 4.5% | 3,1 | 4,5 | 4,7 | 72 |
| cream 35% (fat) | 2,5 | 35,0 | 3,0 | 337 |
| whipped cream | 3,2 | 22,2 | 12,5 | 257 |
| sour cream 30% | 2,4 | 30,0 | 3,1 | 294 |
Cheeses and cottage cheese | ||||
| parmesan cheese | 33,0 | 28,0 | 0,0 | 392 |
Meat products | ||||
| fatty pork | 11,4 | 49,3 | 0,0 | 489 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
| bacon | 23,0 | 45,0 | 0,0 | 500 |
Sausages | ||||
| smoked sausage | 9,9 | 63,2 | 0,3 | 608 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
| salmon | 19,8 | 6,3 | 0,0 | 142 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
| salmon | 21,6 | 6,0 | — | 140 |
| trout | 19,2 | 2,1 | — | 97 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Alcoholic drinks | ||||
| dry red wine | 0,2 | 0,0 | 0,3 | 68 |
| vodka | 0,0 | 0,0 | 0,1 | 235 |
| beer | 0,3 | 0,0 | 4,6 | 42 |
Non-alcoholic drinks | ||||
| soda water | 0,0 | 0,0 | 0,0 | — |
| cola | 0,0 | 0,0 | 10,4 | 42 |
| instant coffee dry | 15,0 | 3,5 | 0,0 | 94 |
| sprite | 0,1 | 0,0 | 7,0 | 29 |
| * data is per 100 g of product | ||||
Classification
Based on etiology, hepatosis is divided into non-alcoholic fatty liver disease and alcoholic steatosis. The first type of disease is diagnosed in only 7–10% of cases.
Hepatosis occurs:
- primary - caused by metabolic disorders, for example, obesity or hyperlipidemia;
- secondary – due to the impact on the body of external negative factors, which subsequently lead to metabolic disorders, for example, fasting, long-term use of corticosteroids, intestinal resection.
Doctors also take into account the characteristics of fat deposition, according to which hepatosis is divided into:
- diffuse;
- zonal;
- focal disseminated;
- pronounced disseminated.
Symptoms of fatty liver disease
There are no specific signs of fatty liver hepatosis, even when there are already significant morphological changes. This is the insidiousness of the disease and lies a serious danger.
At the initial stage, the following nonspecific symptoms of fatty hepatosis may occur:
- general fatigue, asthenia, decreased ability to work;
- heaviness in the abdomen, stool instability, discomfort in the right hypochondrium, nausea, flatulence, sometimes vomiting;
- weight gain;
- causeless increase in body temperature for a long period of time;
- slight enlargement of the liver;
- skin itching.
As the disease progresses, icteric staining of the mucous membranes and skin is possible. Blood pressure often decreases and fainting occurs. There is a tendency to hemorrhages (increased bleeding).
There are 3 degrees of fatty hepatosis depending on the lesion:
- up to 33% – I degree;
- 33–66% – II degree;
- more than 66% – III degree.
Diagnostics
Diagnosis of the disease is difficult. Firstly, steatosis has no specific symptoms. Secondly, biochemical tests do not show significant changes. Sometimes the activity of serum transaminases increases, but this indicator does not change in all patients with steatosis. In this regard, differential diagnosis with hepatitis, biliary tract obstruction, primary hemochromatosis, and hepatocerebral dystrophy is of primary importance.
The doctor makes the final diagnosis based on a comprehensive examination and a series of tests, including ultrasound and biopsy.
To find out the cause of fatty hepatosis, the level of insulin in the blood, serum glucose concentration, hormonal status, antibodies to cytomegalovirus and hepatitis viruses, markers of autoimmune hepatitis, etc. are determined.
Treatment of fatty hepatosis
Treatment of fatty hepatosis is usually complex, including diet therapy, drug therapy and physical therapy.
Diet plays an important and sometimes paramount role in the treatment of steatosis. Sometimes, to cure the first stage, it is enough to follow a diet. Thanks to a significant limitation of fat consumption, healthy cells, and there are more than 66% of them, independently remove the fat present in the liver. But even in the later stages, nutritional correction is a prerequisite. It is recommended to steam food, eat more greens, vegetables and low-fat dairy products, eggs, cereals, and vegetarian dishes.
The cause of its occurrence directly affects how fatty hepatosis is treated.
Weight loss is a necessary condition for obese patients. As a rule, this helps to get rid of insulin resistance, which leads to normalization of carbohydrate and lipid metabolism. But there is one important nuance here - you should not lose weight too quickly (up to 600 g per week is allowed), otherwise there is a risk of progression of fatty hepatosis.
For alcoholic fatty degeneration, successful treatment is only possible with complete abstinence from alcohol. Patients are recommended to consult a narcologist.
Lipotropic drugs for fatty hepatosis are prescribed to accelerate the removal of fat from the liver. This category includes drugs that normalize cholesterol and lipid metabolism, promote fat oxidation and its mobilization from the liver: lipoic acid, essential phospholipids, folic acid, B vitamins.
To prevent the destruction of cell membranes and stimulate the regeneration of hepatocytes, hepatoprotective drugs are prescribed for fatty liver hepatosis: betaine, taurine, ursodeoxycholic acid, glutargin, phosphatidylcholine,
Tablets containing ursodeoxycholic acid often prescribed for fatty hepatosis: Livodexa, Grinterol, Urdoxa, Ursodez, Ursoliv, Ursofalk, Exchol, Ekurochol.
Thiazolidinediones and biguanides are used to eliminate insulin resistance.
The utilization of fatty acids is improved by physical exercise, so it is recommended for all patients with this disease.
Obesity... of the liver: what is dangerous about steatohepatosis and how to live with this diagnosis?
Our expert:
Evgeniy Ivanovich SAS
gastroenterologist, hepatologist, doctor of medical sciences, professor, leading researcher at the research center of the St. Petersburg State Pediatric Medical University
– Evgeny Ivanovich, let’s start the conversation with a clear definition of the diagnosis. There are names “fatty hepatosis”, “fatty liver”, “non-alcoholic fatty liver disease” (NAFLD), “steatohepatosis”. Do all these terms refer to the same disease or different ones?
- Yes and no. At first glance (we often see this in publications) these are different names for the same disease. Let's say that we have a patient with diabetes or obesity. In this case, the diagnosis “non-alcoholic fatty liver disease” (NAFLD) would sound more correct, which reflects that metabolic disorders play a major role in the development of the pathology. When the cause is not yet known (it could be drug, toxic or alcohol-induced liver damage), we use the terms “fatty liver disease”, “fatty liver” or “steatohepatosis”.
– What are the symptoms and signs of fatty liver disease? How long can the disease develop asymptomatically, because, as you know, the liver is one of the most “silent” organs; it does not “report” its unfavorable condition until the onset of a very serious condition...
– Symptoms of fatty liver disease are truly nonspecific. These are increased fatigue, daytime sleepiness, insomnia at night, and so on. Many have already recognized themselves (especially on the eve of vacation), right? However, these symptoms can be either a consequence of simple fatigue or a signal of many other diseases. The only reliable option for detecting fatty hepatosis (which has been practiced in our country for many years) is preventive examinations with a biochemical blood test and ultrasound examination of the abdominal organs - a kind of “technical examination of the body.”
– What happens in the liver during fatty hepatosis? Do I understand correctly that functional cells - hepatocytes are replaced by adipose tissue? Is this dangerous, and if so, what is this danger?
– Let’s imagine a librarian (or any other person) who has gained 30–50 kilograms in weight. He comes to work in the morning and must carry out his job duties: maintain a file cabinet, look for requested books (sometimes climb on a stepladder to get them), arrange returned books... By lunchtime it will become clear that every extra kilogram has to be worked off, and there is absolutely no strength left . Roughly the same thing happens with the liver: the cells are filled with fat, it’s difficult for them to work, but they can’t “reach out to the owner.”
– What factors contribute to the occurrence of fatty hepatosis? Which of them depend only on the patient himself and can be corrected by him?
– First of all, it is necessary to talk about the wrong way of life. Excessive consumption of sweet and fatty foods, sedentary lifestyle. Separately, I would like to say about the excessive consumption of healthy foods. In the summer, many people try to make up for what they missed during the long winter, saturate their bodies with “fresh vitamins” and begin to consume large quantities of fresh fruit (or actively feed their children with it). One kilogram of grapes, bananas, persimmons, dates, some varieties of apples and other sweet fruits contains a lot of carbohydrates and, accordingly, an amount of calories that we cannot spend during the day. This is a sure step towards obesity and fatty hepatosis. Separately, I would like to dwell on physical activity: recent studies have shown that skeletal muscles have hormonal activity, so physical education will help not only normalize metabolism, but also reduce the activity of the inflammatory process in the liver and pancreas.
– How is the diagnosis made? What tests do I need to take and what studies do I need to undergo? What should serve as a warning signal for a person to make an appointment with a hepatologist? Or do you need to check the condition of your liver periodically, even if nothing worries you?
– It is quite difficult to get to a hepatologist, and the need to visit him arises when we cannot establish the cause of fatty hepatosis or all attempts to treat it are unsuccessful. As a rule, the diagnosis is made by the “first contact” doctor – the therapist. To do this, it is necessary to perform a biochemical blood test and an ultrasound examination of the abdominal organs. But, I will repeat once again, in view of the importance of what has been said: the leading role in the diagnosis of fatty hepatosis is given to an annual in-depth medical examination.
– Is it correct to talk about prevention in relation to fatty hepatosis? Is it possible to prevent the occurrence and development of this disease?
– Fatty hepatosis is exactly the disease to which it is very appropriate to apply the concept of prevention. Eating enough dietary fiber (porridge, vegetables), reducing the consumption of sweets first and then fatty foods, physical activity, consuming fish oil (not in the form of cooked fatty fish, which will add a few extra centimeters to the waist, but in the form of food supplements) is an adequate prevention of fatty hepatosis.
– If the diagnosis has already been established, what changes should occur in the patient’s life? For example, do you need to adjust your diet and how severe should such dietary changes be?
– Food should be varied and sufficient. Our diet contains a huge number of foods that are low in calories and at the same time beneficial for the liver (low-fat cottage cheese, turkey, rabbit, strawberries, raspberries, etc.), which allows the patient not to feel “deprived”. I try to avoid the word “diet,” which scares off many patients, or talk about a specific period of dieting. This is a healthy lifestyle that needs to be followed from childhood. As a rule, all exotic diets combined with the use of a “miracle” product or technique are based on the basic principles of a healthy lifestyle. I would like to warn readers: a sharp restriction of calories and rapid loss of body weight may be accompanied by an increase in hepatosis at the first stage and an increase in the lithogenicity of bile (the tendency to form stones). Therefore, it is necessary to “accompany” the patient with a doctor at this stage and timely correction of these changes with ursodeoxycholic acid drugs (ursosan).
– How to treat the disease? How often should you visit a doctor? Should a patient with fatty hepatosis be registered with a hepatologist and periodically monitor the dynamics of the disease?
– The therapy is based on lifestyle modification: the use of foods with a low glycemic index, increased aerobic (walking, running, swimming, etc.) exercise, mandatory correction of intestinal microflora, as well as the use of drugs that have a hepatotropic effect (restoring liver function) . Separately, it is necessary to touch upon the correction of metabolic disorders: for patients with diabetes mellitus, this is control of sugar levels; for patients with lipid metabolism disorders – normalization of cholesterol levels. In this regard, the doctor determines on an individual basis the frequency of visits to his patient.
– What are the prognosis for the development of fatty hepatosis? Can he be completely cured? Are the changes that occur with this liver disease reversible or irreversible? Can steatohepatosis lead to serious consequences for the liver - for example, cirrhosis, cancer?
– Fatty hepatosis is reversible, so it is necessary to strive to cure it. However, with the long-term development of the disease, an inflammatory process occurs, which leads to fibrotic changes (which are already irreversible) in the liver, followed by possible cirrhotic and oncological transformation, which determines the need for early diagnosis and treatment of this disease.
Interviewed by Tatiana GOLTSMAN
Fatty hepatosis of pregnant women
Separately, there is hepatic steatosis, which occurs without a significant cause in women bearing a child. Acute fatty hepatosis of pregnancy is diagnosed in one out of 13,000 women. 20–25% of cases end in death, according to foreign authors, and up to 60%, according to domestic sources.
The disease progresses quickly, over 2–3 weeks. Occurs mainly in late pregnancy - 32–36 weeks. The exact cause of this pathology has not yet been established.
Symptoms that may indicate acute fatty hepatosis in pregnant women: excessive vomiting, severe nervous disorders, general weakness, drowsiness.
The only treatment method is emergency delivery. Within 5 weeks after birth, the disease regresses.
Authorized Products
The diet for liver hepatosis includes inclusion in the diet:
- Vegetable broths and soups based on them with the addition of cereals, noodles, and vegetables.
- Low-fat varieties of red meat (beef/veal), rabbit, chicken, turkey. The meat must be pre-boiled followed by cooking.
- Day-old/dried wheat bread up to 500 g per day. If well tolerated - rye bread, low-fat cookies, dry biscuit.
- Low-fat types of sea/river fish, baked with vegetables.
- Cereals in the form of casseroles, porridge.
- Low-fat fermented milk products: yogurt, kefir, bifidum-kefir, acidophilus and low-fat cottage cheese.
- Milk/sour cream only as an additive to prepared dishes.
- Chicken eggs in the form of a steam omelet/soft-boiled.
- Fresh, baked and stewed vegetables in the form of salads with the addition of vegetable oil, mashed potatoes and homemade squash caviar. Spices include garden herbs, cumin, bay leaf.
- Sour cream, milk and vegetable sauces.
- Non-acidic fruits/berries in fresh and processed form (jelly, compotes, mousses).
- Marmalade, honey, caramel, marshmallows, jams, toffee. Sugar is partially replaced with xylitol.
- Butter/vegetable oil is added only to ready-made dishes; heat treatment is excluded.
- Still table water, rosehip infusion, weak tea, vegetable juices, wheat bran decoction, coffee with milk (not strong).
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| broccoli | 3,0 | 0,4 | 5,2 | 28 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Fruits | ||||
| apricots | 0,9 | 0,1 | 10,8 | 41 |
| quince | 0,6 | 0,5 | 9,8 | 40 |
| watermelon | 0,6 | 0,1 | 5,8 | 25 |
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| pears | 0,4 | 0,3 | 10,9 | 42 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
| kiwi | 1,0 | 0,6 | 10,3 | 48 |
| peaches | 0,9 | 0,1 | 11,3 | 46 |
| plums | 0,8 | 0,3 | 9,6 | 42 |
| persimmon | 0,5 | 0,3 | 15,3 | 66 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| strawberry | 0,8 | 0,4 | 7,5 | 41 |
| blueberry | 1,1 | 0,4 | 7,6 | 44 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| dried figs | 3,1 | 0,8 | 57,9 | 257 |
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| dried apricots | 5,0 | 0,4 | 50,6 | 213 |
| prunes | 2,3 | 0,7 | 57,5 | 231 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
| buckwheat noodles | 14,7 | 0,9 | 70,5 | 348 |
Bakery products | ||||
| wheat bread | 8,1 | 1,0 | 48,8 | 242 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| fruit and berry marmalade | 0,4 | 0,0 | 76,6 | 293 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
Dairy | ||||
| kefir 1.5% | 3,3 | 1,5 | 3,6 | 41 |
| curdled milk 1% | 3,0 | 1,0 | 4,1 | 40 |
| acidophilus 1% | 3,0 | 1,0 | 4,0 | 40 |
Cheeses and cottage cheese | ||||
| cottage cheese 1% | 16,3 | 1,0 | 1,3 | 79 |
| cottage cheese 1.8% (low-fat) | 18,0 | 1,8 | 3,3 | 101 |
Meat products | ||||
| beef | 18,9 | 19,4 | 0,0 | 187 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken breast | 29,8 | 1,8 | 0,5 | 137 |
| boiled chicken drumstick | 27,0 | 5,6 | 0,0 | 158 |
| boiled turkey fillet | 25,0 | 1,0 | — | 130 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Fish and seafood | ||||
| flounder | 16,5 | 1,8 | 0,0 | 83 |
| pollock | 15,9 | 0,9 | 0,0 | 72 |
| cod | 17,7 | 0,7 | — | 78 |
| hake | 16,6 | 2,2 | 0,0 | 86 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
Non-alcoholic drinks | ||||
| water | 0,0 | 0,0 | 0,0 | — |
| mineral water | 0,0 | 0,0 | 0,0 | — |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| peach juice | 0,9 | 0,1 | 9,5 | 40 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| rose hip juice | 0,1 | 0,0 | 17,6 | 70 |
| * data is per 100 g of product | ||||
Prevention
Preventive measures include:
- proper nutrition, in particular limiting fatty, spicy, fried and smoked foods;
- moderation in the consumption of alcoholic beverages;
- taking medications correctly;
- regular physical activity.
Fat accumulation is often caused by excess weight due to a sedentary lifestyle. Scientists have proven that if you eat only fast food for 4 weeks, this disease will almost certainly occur. Student volunteers took part in the experiment. Moreover, the first signs appeared after 1 week of such nutrition. Therefore, nutrition and weight control are of great importance.
For prevention, hepatoprotectors should be used, especially during periods of increased load on the liver, for example, with prolonged alcohol consumption, antibiotic treatment, and following a diet aimed at weight loss.
Diet features
General recommendations for diet for fatty hepatosis:
- Refusal of alcoholic beverages;
- Limiting fatty, fried, smoked, sweet foods;
- Food at least 3 times a day;
- Increase fluid intake per day;
- Baked, boiled, steamed food;
- Increase in the diet of vegetables and seafood;
- A sufficient amount of calories in the diet (moderate deficit if necessary to lose weight);
- Limiting salt in the diet to 6-8 g per day;
- Limiting spices and spicy foods.
Following a healthy diet early in the course of the disease can be a key component of treatment.
Frequently asked questions about fatty liver disease
Which doctor should I contact?
A hepatologist specializes in liver diseases.
How to determine fatty hepatosis?
Unfortunately, the disease has no specific symptoms. A comprehensive examination allows you to identify deviations.
Can hepatic steatosis be cured?
With proper and timely therapy, changes in the liver are reversible. The main thing is to strictly follow all the doctor’s instructions, stick to your diet, and give up alcohol and “harmful” foods.