How common is cytomeglovirus infection?
Infection with cytomegalovirus can occur in several ways:
- Airborne
- During a kiss
- Contact and household
- Sexually
- During blood transfusion
- In utero from mother to fetus
- In childbirth from mother to baby
- When breastfeeding through mother's milk to the baby
Airborne transmission, according to doctors, is quite rare. Therefore, ordinary communication with a patient or carrier does not pose a great danger. Most often, people become infected through household contact, sexual contact and through kissing.
Clinical signs of cytomegalovirus infection
CMV infection can develop in three different ways. Each of them requires a different approach to treatment. Here are the forms of the disease:
- Cytomegalovirus enters the human body with a normal immune system
- Cytomegalovirus infection in immunodeficiency
- Congenital generalized cytomegalovirus infection.
The symptoms of the disease for each variant of the disease and the characteristics of its course differ from each other.
CMV infection in people with a normal immune system who do not suffer from chronic diseases resembles a common cold. The main symptoms are headache, general malaise, decreased performance, decreased attention, runny nose, bronchitis, muscle pain. Patients develop the so-called mononucleosis-like syndrome, which may be accompanied by chills and fever, sore throat, enlarged tonsils and all groups of lymph nodes. Over the course of several weeks, the body copes with the virus on its own. Often the diagnosis is not made, attributing the manifestations of infection to a common ARVI. The duration of the incubation period for CMV infection is 3-8 weeks. Therefore, identifying the source of infection can be very difficult, almost impossible.
The chronic form proceeds unnoticed, occasionally manifesting as mild cystitis or inflammation of the kidneys. But with any immunity disorder, an exacerbation of cytomegaldovirus infection can occur. The carrier of the virus poses a danger to people living with him or his sexual partner. In most cases, the person feels completely normal, the infection occurs in a latent form.
Cytomegalovirus is dangerous for people with impaired immunity. First of all this:
- HIV-infected
- Patients taking immunosuppressants and undergoing chemotherapy
- Patients after organ transplantation or after extensive surgery
- Patients with chronic renal failure undergoing hemodialysis
Cytomegalovirus infection in this group of patients is severe, and its consequences are difficult to predict. The process involves the liver, spleen, kidney tissue and adrenal glands, gastrointestinal tract, and pancreas. Also characteristic are manifestations from the respiratory system, sore throat, rash, enlargement of almost all lymph nodes of the body, and the number of platelets in the blood decreases.
In immunocompromised patients, cytomegalovirus infection can cause death.
Congenital cytomegalovirus infection is relatively rare. It is diagnosed if the mother is infected in the second or third trimester. When the embryo is affected before 12 weeks, miscarriage most often occurs.
Prognosis and prevention
In immunocompetent people, carriage of the virus does not affect the quality of life. Only a few studies indicate the risk of developing atherosclerosis with long-term persistence of CMV in the body. The prognosis for immunodeficiency depends on the clinical manifestations of the disease and the timeliness of treatment. The highest mortality rate is characterized by cytomegalovirus pneumonia.
Prevention methods:
- compliance with personal hygiene rules (You must wash your hands regularly);
- separate meals with the child;
- regular cleaning of any objects that have come into contact with the child’s urine or saliva (This is especially true for toys);
- using a condom;
- regular examinations for HIV positive status and other conditions that negatively affect immunity.
- drug prevention of infection during organ transplantation and use of immunosuppressants.
Thus, cytomegalovirus infection is a viral disease that can affect human organs and tissues when the immune system is impaired. First of all, this pathology is dangerous for pregnant women and children, so screening for CMV must be carried out in advance.
Diagnosis of CMV
When a patient comes to the doctor with complaints of prolonged malaise, low-grade fever, especially if enlarged lymph nodes are detected, he is prescribed additional tests. Cytomegalovirus is detected in various body fluids - blood, saliva, urine, vaginal secretions, semen. Most often, urine is sent for analysis.
Additional examination methods also include:
- Growing the virus in cell culture or hybridization
- PCR (polymerase chain reaction) with detection of cytomegalovirus DNA
- Blood test for antibodies (serological diagnosis)
PCR is by far the most informative method. It helps detect DNA by amplifying material at a specific temperature with a special primer that replicates the genetic material of the virus. But this analysis does not yet indicate the presence of an acute infection, because many people are carriers of CMV. When detecting a virus by PCR, it is necessary to determine its quantity and dynamics of increase over time, as well as take into account clinical symptoms.
Many laboratories use the technique of cultivating the virus in cell culture. The study makes it possible to find out the type of pathogen and determine the degree of its virulence. The technique also allows you to determine sensitivity to drugs and select the most effective treatment regimen.
Cytomegalovirus, entering the body, causes the production of antibodies. Serological studies can determine them. The detection of IgG in the blood indicates infection with the virus, an increase in their titer indicates a possible exacerbation of the infection, and the presence of IgM indicates an acute process. To detect an increase in antibody titer, studies are carried out several times with an interval of 10-15 days. If there are no clinical symptoms, but the IgG level increases, a diagnosis of latent cytomegalovirus infection is made. If IgM is present, an acute illness is diagnosed, but it is advisable to confirm the results using other tests
Cytomegalovirus infection (CMVI) is a widespread human infectious disease, with vertical, sexual, parenteral, and oral transmission routes through blood, cervical and vaginal secretions, sperm and human milk. In most cases, the infection occurs without clinical manifestations. With immunosuppression caused by various reasons, cytomegalovirus (CMV) can lead to the development of a disease with a variety of symptoms, which is due to its ability to infect almost all organ systems (retinitis, uveitis, seronegative mononucleosis, pneumonia, hepatitis, diseases of the gastrointestinal tract, central nervous system , post-transfusion syndrome) [1-5].
On average, 90-95% of the adult population has antibodies to CMV. The literature provides numerous data on the features of the course of CMV infection in newborns, pregnant women and immunocompetent patients. Currently, the following categories of citizens are subject to examination for CMV infection: women preparing for pregnancy, pregnant women and patients with identified immunodeficiency conditions. Special attention is paid to studying the significance of CMV in the pathology of the adult population [6–9]. However, it is not taken into account that CMV often contributes to chronic inflammatory damage to the pelvic and genital organs, which causes low effectiveness of treatment for sexually transmitted infections (STIs) and a decrease in the reproductive capacity of patients.
The purpose of this study is to determine the forms of CMV infection of the urogenital tract in sexually active women of reproductive age.
Material and methods
We observed 356 patients with CMV, which was characterized by the presence of anti-CMV IgG in the blood.
To identify CMV, an enzyme-linked immunosorbent assay (ELISA) was used to identify specific anti-CMV class IgM (qualitative analysis) and class IgG (quantitative analysis) in the blood serum, which was carried out by the sandwich method of solid-phase ELISA using diagnostic kits Diagnostic systems (Russia ). To detect antibodies of the IgM class, the DS-ELISA-ANTI-CMV-M CM-153 test system was used, and to detect antibodies of the IgG class, the DS-ELISA-ANTI-CMV-G CM-151 test system was used. Virological detection of CMV was carried out on a culture of human embryonic lung fibroblasts, in the study of blood, saliva, urine, discharge from the cervical canal, urethra and vagina. Monoclonal antibodies to the immediate early (pp72) and early (pp65) antigen were used to detect the CMV antigen using an indirect fluorescence reaction. CMV DNA was determined by polymerase chain reaction (PCR). Conditionally pathogenic and pathogenic flora of the urogenital tract were studied using regulated methods - microscopic, bacteriological, molecular genetic.
To identify reliable trigger clinical and laboratory factors associated with CMV infection of the urogenital tract, the data from the survey and examination of patients were compared with the results of similar studies conducted in the control group, which consisted of 120 women. The selection criteria were: reproductive age, absence of pregnancy, lactation, systemic and local antibacterial therapy within 1 month before the start of this examination, normal state of the microflora of the urogenital tract and excluded CMV infection.
Statistical calculations were performed using SPSS 17.0. All obtained quantitative anamnestic, clinical, laboratory and instrumental data were processed using the methods of variation statistics. To compare numerical data (after checking for normal distribution), ANOVA (for several groups) and Student's t-test for two independent samples were used. For comparison of nonparametric data, Kruskal-Wallis methods were used (for several groups), pairwise comparisons were carried out using the Mann-Whitney test (for two groups) for unrelated populations. To determine differences between qualitative indicators, we used the χ2 method with Yates' correction for continuity, for the calculation of which 2×2 and 3×2 “grids” were built, as well as Fisher’s exact test for small samples. Differences were considered statistically significant at p<0.05 (95% significance level) and p<0.01 (99% significance level).
results
The majority of women with CMV infection noted the presence of vaginal discharge (61.52%), itching (27.81%) and discomfort in the genital area (37.92%). Pain during sexual intercourse was registered in 12.92% of cases. 21.07% of the patients in the main group had no complaints (68.33% of women in the control group; Table 1).
Information about previous somatic and infectious diseases is important for clarifying the nature of CMV infection. The frequency of extragenital pathology indirectly reflects the state of the body’s anti-infective defense and immune system as a whole.
When analyzing somatic pathology (Table 2)
the most common infectious viral diseases (82.58% of cases), gastrointestinal tract pathology (55.9%) and respiratory diseases (20.51%) were noted in the main group compared to the control group. In patients with CMV infection, pathology of the endocrine system was 4.2 times more likely (in 31.46% of cases; p<0.05).
Data on gynecological diseases, which are among the factors influencing the state of systemic and local immunity, were subjected to detailed analysis.
Among the gynecological diseases experienced, the most common pathologies were the cervix (44.10% of cases; p<0.05) and inflammatory diseases of the pelvic organs (75%; p<0.05) compared with the control (Table 3).
In addition, women with CMV infection were more likely to have STIs (in 55.34% of cases; p<0.05) and infertility (28.65%; p<0.05).
When studying the characteristics of sexual history (Table 4)
It was found that patients with CMV infection were 3 times more likely (p<0.05) to have an early onset of sexual activity. The ratio of women by number of sexual partners in both groups was comparable. During the analysis of the characteristics of sexual preferences, it was found that patients of the main group more often practiced anogenital contacts (p<0.05).
More than 84% of patients with CMV and 70% of women from the control group had a history of unprotected sexual intercourse (including without using a condom followed by treatment with miramistin solution) (p<0.05).
Thus, a likely predisposing factor for CMV infection of the urogenital tract was early onset of sexual activity and a large number of unprotected anogenital contacts.
During the clinical examination, the characteristics of subjective sensations were analyzed and a thorough general and gynecological examination was performed.
In women with CMV infection, a varied nature of discharge from the vagina and cervix was noted (Table 5):
often abundant (39.61%), predominantly yellow-white (85.39%), homogeneous (76.12%), viscous (51.69%) or liquid (48.31%). Hyperemia of the cervical mucosa was registered in 54.78% of cases, vaginal hyperemia - in 25.56%, contact bleeding - in 46.91% of cases. During bimanual examination, these women more often noted pain and enlargement of the uterine appendages, and the presence of adhesions (in 32.58 and 58.15% of patients, respectively). In the control group, examination in the mirrors more often revealed scanty discharge (52.5%), white (95%), homogeneous in 100% of cases and viscous in 85.83% of women. No pathology of the mucous membranes was detected in the control group. During bimanual examination, adhesions were observed in only 13.33% of patients.
Thus, in patients with CMV infection, a gynecological examination more often revealed an acute or chronic inflammatory process in the pelvis.
The results of a microscopic examination of Gram-stained smears of the genital tract discharge are presented in table. 6.
Analysis of the results of a cultural study of the discharge of the genitourinary tract of women revealed the dominance of Candida
spp.
(48.60%), G. vaginalis
(30.62%),
T. vaginalis
(21.35%).
In the majority of women, in the vaginal biotopes, there was an association of CMV with opportunistic bacteria ( Streptococcus, St. aureus, Ureaplasma
spp.,
M. hominis
) in a high titer (more than 105 CFU/ml;
Table 7).
The results of a comprehensive examination of these women are presented in Table. 8.
In 71 (19.9%) women, the state of vaginal microecology was assessed as normocenosis. Having analyzed the data obtained, it was possible to highlight some of its features, which in some cases made it possible to call this condition normocenosis only conditionally. Thus, only 22 (6.18%) women out of 356 had a microecological state that fully complied with all the criteria for the norm of reproductive age: microscopy of vaginal discharge showed no pronounced leukocyte reaction (the number of leukocytes did not exceed 10 in the field of view), the epithelium was represented by cells of the superficial and intermediate layers, the amount of microflora was moderate with an absolute predominance of the morphotype of lactobacilli. Morphotypes of opportunistic microorganisms (OPM) were not determined. On culture, the titer of lactobacilli was 106-8 CFU/ml of vaginal discharge, and the concentrations of UPM were low (less than 103 CFU/ml).
In 28 (7.87%) women, the difference from the classic version of normocenosis was the presence of a moderately pronounced leukocyte reaction according to microscopy, in which 10-20 leukocytes were detected in the field of view. In 21 (5.90%) women, a pronounced leukocyte reaction was noted (more than 20 leukocytes in the field of view). With a moderate total amount of microflora and the dominant role of lactobacilli, the appearance of UPM morphotypes has been recorded. When inoculating vaginal contents, lactobacilli were isolated in a titer of 106-7 CFU/ml and moderate concentrations of UPM ( Streptococcus
group B - 104-5 CFU/ml,
St.
aureus - 103-5 CFU/ml). In most cases, UPMs occurred in the form of polymicrobial associations (2-4 associates).
The most common pathology among 356 examined patients with CMV infection was candidiasis (57.30%), in most cases accompanied by a moderate increase in the titer of UPM ( Streptococcus
group B at 106 CFU/ml and
St.
aureus more than 106 CFU/ml).
Aerobic vaginitis (1.12%) as a variant of vaginal dysbiosis was caused by colonization of the vaginal biotope with high titers of E. coli (more than 107 CFU/ml) and group B streptococci (106 CFU/ml). According to microscopy, in these cases there was also a pronounced leukocyte reaction (more than 40 leukocytes in the field of view).
In 21.06% of women, bacterial vaginosis was microscopically established, which was accompanied by high colonization of facultative anaerobic and anaerobic flora (more than 106 CFU/ml).
In 0.56% of cases, the state of vaginal microecology was assessed as another variant of vaginal dysbiosis, when, with a minimum content of microflora (microscopy data), facultative anaerobic and aerobic UPM (Gram-positive cocci) dominated, and lactomorphotypes were single in the field of view.
Thus, only 19.9% of patients with CMV had the classic variant of microcenosis; in other cases, the vaginal microflora underwent changes associated with an increase in the titer of facultative anaerobic UPM. In 80.1% of women, disorders of the vaginal microcenosis were detected, in most cases associated with an increase in the number of Candida
spp.
When examining urethral discharge using PCR, the causative agents of STIs and UPM were identified. The most frequently detected DNA was HPV (11.52%), T. vaginalis, M. hominis
, HSV types 1 and 2 (2.81 and 3.08%, respectively),
C. trachomatis
was identified in the urethra in 5 ,34% of patients.
In the cervical canal, UPM and pathogens were detected 5 times more often. Thus, the most frequently isolated human papillomavirus (42.13%) and T. vaginalis
(11.52%),
M. hominis
(21.63%),
C. trachomatis
(18.82%) and
Ureaplasma
spp. (24.44%).
In vaginal scrapings, human papillomavirus DNA was also most often detected (43.25%), T. vaginalis
(21.35%),
M. hominis
(14.89%),
Ureaplasma
spp.
(19.38%), as well as G. vaginalis
(25%).
When examining samples from the rectum, HPV DNA (28.93%) and M. hominis
(11,24%).
To verify the diagnosis of CMV, an extensive analysis of the results obtained by different research methods was carried out (Table 9).
When analyzing data to identify CMV markers, the highest frequency of detection of anti-CMV IgG was established - 356 (100%) cases. Anti-CMV IgM was detected in 89 (25%) women. The detection of class G antibodies to CMV indicated both infection and the presence in most cases of developed specific antiviral immunity. The detection of class M antibodies together with IgG was one of the signs of reactivation of this viral infection.
When examining material obtained from the urogenital tract using PCR, CMV DNA was detected in 208 (58.43%) women.
CMV in a culture of human lung fibroblasts was detected in 93 (26.12%) women, urine - in 199 (55.90%), saliva - in 204 (57.30%) patients, vaginal discharge - in 225 (63). .20%), from the cervical canal - in 268 (75.28%) cases. Overall, CMV was detected in 268 (75.28%) patients.
Based on the examination results, variants of the course of CMV infection in sexually active women were determined. Latent form
CMV infection was observed in 92 (25.84%) patients.
In this case, positive blood ELISA results (anti-CMV IgG) were combined with the detection of CMV in the genital tract and, in some cases, in other biological fluids. The reactivated form
of CMV was registered in 176 (49.44%) patients and was characterized by the presence of both anti-CMV IgG and anti-CMV IgM in the blood, combined with the detection of CMV in the genital tract and other biological fluids.
The persistent form
of CMV was diagnosed in 88 (24.72%) patients and was characterized by the presence of anti-CMV IgG.
Taking into account the etiology, pathogenesis and clinical manifestations of CMV infection in the urogenital tract, patients with reactivated and latent forms of CMV infection received complex therapy for the infectious process in accordance with clinical recommendations for the management of patients with STIs. Antiviral treatment included the use of the drug Panavir
.
The main active ingredient of this drug is a hexose glycoside, obtained by enzymatic hydrolysis followed by gas-liquid chromatography, consisting of glucose, rhamnose, arabinose, mannose, xylose, galactose, uronic acids. A number of experimental and clinical studies have established the antiviral and immunomodulatory activity of Panavir
.
This drug increases the body's nonspecific resistance to various infections and promotes the induction of interferon. Panavir
(5 ml of 0.004% solution) was administered parenterally (intravenous bolus) once a day after 48 hours (3 injections in the 1st week of treatment), then after 72 h (2 injections in the 2nd week of therapy). In total, the course consisted of 5 injections over 2 weeks.
In a control study conducted 14 days after treatment, only 2 (8.0%) patients with a latent form of CMV had CMV detected in cell culture of the cervical canal discharge; CMV DNA was not detected in 24 (96%) patients. As a result of treatment for the reactivated form of CMV, negativity of IgM anti-CMV in the blood was found in 100% of women. When studying CMV on a culture of human embryonic fibroblasts, viruria was detected in 1 (5.56%) patient, isolation from the cervical canal was noted in 3 (16.67%). The results of a virological examination of blood, saliva, and vaginal discharge were negative in all women. PCR revealed the presence of CMV DNA in 2 (11.11%) patients who received parenteral Panavir
.
Thus, in the course of the study, the main diagnostic clinical and laboratory criteria for various forms of CMV infection of the urogenital tract of sexually active women of reproductive age were determined, on the basis of which the possibilities of identifying this infection have increased significantly. The presence of clinical manifestations in reactivated CMV infection and the identification of viruses in subacute or chronic pelvic inflammatory diseases contributed to determining the significance of this infection in the development of genital pathology. Use of the drug Panavir
in complex therapy increased the effectiveness of treatment in 89.5% of cases, which allows us to recommend the drug
Panavir
for complex therapy of CMV infection.
Cytomegalovirus infection in pregnant women
Every fourth woman in our country who registers with an antenatal clinic due to pregnancy is diagnosed with cytomegalovirus. The level of infection among pregnant women with an antisocial lifestyle and promiscuous sexual intercourse is much higher; they are often diagnosed with other STIs. If an exacerbation of infection occurs during pregnancy, the chance of developmental pathologies in the newborn increases to 85%. Here are some defects that can be detected in children whose mothers suffered an infection during pregnancy:
- Delayed growth, physical and mental development
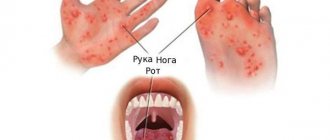
- Various types of vasculitis
- Skin rashes
- Retinopathy and other vision disorders
- Congenital deafness or hearing loss
- Increase in the size of various internal organs
- Improper development of teeth
The mortality rate of infants with congenital cytomegalovirus infection reaches 30%, and when infected or worsened in the first trimester, miscarriages most often occur. If intrauterine infection does not occur, there is a risk of transmission of the virus during passage through the birth canal. The pathogen can enter the newborn’s body from the mucous membranes or from the blood. cases of infection through breast milk have also been reported. Therefore, when diagnosing an acute disease, it is recommended to exclude breastfeeding.
If a pregnant woman has a cytomegalovirus infection that remains latent, there is practically no danger to the fetus and newborn child. In the normal state of the mother's immune system, her antibodies are transferred through the placenta to the baby. In such a situation, even an imperfect newborn defense system can cope with the pathogen. The placenta also protects the child’s body from the penetration of the virus, especially when its concentration in the mother’s blood is low. If a pregnant woman who registers has a low titer of antibodies and no clinical symptoms, treatment is not prescribed. The doctor monitors the patient and recommends repeated tests. They are also advised to lead a healthy lifestyle, not to overwork, and protect yourself from infections so as not to undermine the immune system.
It is best to identify cytomegalovirus infection before pregnancy by passing all the necessary tests. This will allow you to undergo treatment and not risk the baby’s health. If IgG is not detected in the ELISA, the pregnant woman is still advised to undergo examination every 3 months. After all, the most dangerous thing for the development of the fetus is the primary infection of the expectant mother. Both partners should be examined to rule out sexual transmission during this period. It is necessary to avoid accidental contacts, unnecessary kisses, and adhere to hygiene rules, especially in public places.
Symptoms
If the pathogen is in the body in a latent form, there are no symptoms of CMV in women. Signs of the disease appear only if the disease becomes acute. Then the patient complains of symptoms characteristic of ARVI: fever, weakness, cough, nasal congestion, muscle aches, headaches.
In the generalized form of cytomegalovirus infection, women may experience skin rashes, blurred vision, enlarged lymph nodes, inflammatory processes in internal organs, and damage to the nervous system.
Inflammatory processes affecting the genitourinary organs may also occur.
Treatment of cytomegalovirus
Before starting treatment for cytomegaovirus infection, two points should be taken into account:
- If there are no complaints or clinical symptoms, treatment is not prescribed
- When a patient has a weakened immune system, treatment is a vital necessity.
It is impossible to completely remove cytomegalovirus from the body. Also, you cannot select medications yourself, this will not have an effect and will not reduce the amount of the pathogen. The course of the disease in each patient has its own characteristics. Therefore, medications, doses, and course duration must be selected strictly individually, taking into account the type of virus and its concentration.
Complex treatment of cytomegalovirus infection consists of two directions. First of all, medications are prescribed that destroy the virus itself. The second direction is strengthening immunity. Antiviral treatment includes taking drugs such as ganciclovir, foxarnet, panvir, valganciclovir, etc. These drugs are quite toxic, therefore they have a number of side effects and contraindications. Drinking them on your own, without a doctor’s prescription, is strictly prohibited. This can lead to a number of negative consequences. One of them is disruption of the immune system, reducing the effectiveness of natural antiviral defense.
In some cases, doctors prescribe immunoglobulins to treat cytomegalovirus infection. They can be synthetic or made from blood products. These drugs contain ready-made antibodies against CMV or their analogues. Medicines are produced in the form of injections; they must be administered under strict medical supervision. Immunoglobulin preparations have proven their effectiveness, but the mechanism of their action has not yet been fully studied. Therefore, therapy is prescribed after a comprehensive examination and tests. Treatment of cytomegalovirus with immunoglobulin has a number of contraindications:
- Vaccination against certain viral diseases, carried out in parallel with the prescribed treatment
- Diabetes mellitus type I or II
- Tendency to allergic reactions
- Kidney failure or other urinary system problems
- Carrying and feeding a baby
The patient should be monitored during treatment. It is important to inform your doctor about the appearance of shortness of breath, difficulty urinating, a cold or ARVI, even in the mildest form, the appearance of edema, or a sharp increase in body weight. In this case, the specialist conducts an examination and adjusts the treatment. Symptoms of an allergy to the drug may be similar to those of meningitis. The patient experiences drowsiness, headache, photophobia and pain in the eyes, nausea and sudden vomiting.
Treatment
Drug treatment of infection involves the use of various antiviral agents. Clinical guidelines instruct physicians to prescribe cytomegalovirus immunoglobulin, ganciclovir, foscarnet, or cidofovir to patients. The specific treatment regimen depends on the symptoms of the disease and the patient’s condition.
Description of drugs
- Cytomegalovirus immunoglobulin is a specific class G antibody that can fight the virus. The drug blocks the ability of the virus to influence cell signaling systems and stimulate the assembly of virions. This medicine is used as primary therapy in combination with other antiviral medicines or prescribed to prevent the disease. The use of immunoglobulin can significantly reduce the risk of complications of the disease.
- Ganciclovir, foscarnet and other drugs block viral replication. Side effects of these drugs include increased bleeding, kidney damage, and gastrointestinal dysfunction. In case of renal failure, such medications are used as a last resort.
Timely implementation of prevention allows you to suppress the infectious process and gives the patient the opportunity to avoid taking dangerous drugs.
How to prevent CMV infection
To prevent infection with cytomegalovirus infection, you should first use condoms. Most often this applies to cases when you are not sure about the health of your partner. Very often, the virus is transmitted through kissing, so you should not come into close contact with people who have a fever, sore throat, weakness, and other symptoms of ARVI. Such precautions are very necessary for pregnant women so as not to transmit the dangerous virus to the baby in the womb.
To avoid infection or exacerbation, you should strengthen your immune system. Doctors give the following simple advice:
- Practice hardening the body
- Adhere to hygiene rules
- Exercise
- Eat right, the menu should contain the optimal amount of vitamins
- If necessary, use dietary supplements
There are a number of medicinal plants that effectively treat exacerbation of cytomegalovirus infection and prevent its development. These include ginseng root, echinacea, and lemongrass. Preparations based on these herbs, teas and infusions have an antiviral effect and also strengthen the human immune system.
Pathogenesis (what happens?) during Cytomegalovirus infection
The entry point for Cytomegalovirus is the mucous membrane, mainly of the upper respiratory tract and oropharynx. Infection can also occur through the genitourinary system, gastrointestinal tract and other organs.
There are no structural changes observed at the injection site. After the virus enters the body, it begins to attack mono- and lymphocytes, as well as the epithelium of the salivary glands, kidneys, lungs and other internal organs. In this case, cytomegaly is observed (an increase in the size of the affected cells by 3-4 times). Immature virions are formed in the cell nuclei. As a result, the cellular structures take on the appearance of an “owl’s eye.” The active course of the disease leads to the development of depression of most parts of the immune system, including the IFN-α protein.
In response to the penetration of CMV, a protective reaction develops - specific antibodies are formed, and delayed-type hypersensitivity is observed. This process is accompanied by the appearance of nodular formations of lymphocytic infiltrates. Cells that have been infected continue to function, secreting a special secret that masks the virus from the protective functions of the human body.
Traditional recipes for cytomegalovirus infection.
Folk remedies prevent exacerbation of cytomegalovirus infection. They can be included in complex treatment, but in no case exclude antiviral drugs. Here are some useful recipes:
- Multi-component infusion, including 7 herbs. It includes wild rosemary, birch buds, yarrow, leuzea, thyme, string and burnet. You should take the same amount of each ingredient. Then add 10 g of the herbal mixture from the total mass, pour in a liter of boiling water and leave in a thermos for 12 hours. Drink a quarter glass with meals.
- A collection of leuzea, licorice, kopeck, alder, chamomile and string in equal parts is brewed and drunk in the same way as in the previous recipe.
- Take 4 parts of licorice root and 1 part each of flax seeds, marshmallow root, coltsfoot and raspberry leaves, cinquefoil and elecampane. Pour a liter of boiling water and leave for 3 hours. Drink a quarter glass three times a day.
- Very useful for viral infections, including CMV, garlic and onions. If you add one clove of garlic and a sixth of an onion to your dishes every day, the risk of infection and worsening the infection drops by 30%
- To prevent airborne infection, tea tree oil can be sprayed in the room where the patient is located. It is best to use an alcohol solution for this purpose, which is sold in pharmacies. Pure oil can be added to the aroma lamp.
Gynecologist's recommendations for disease prevention
For infection to become possible, it is necessary to come into very close contact with an infected person.
Therefore, to prevent cytomegalovirus infection in women and protect against possible consequences, it is recommended to responsibly choose sexual partners, as well as donors in the case of blood transfusion or organ transplantation. Also, to prevent CMV, it is recommended to use personal dishes and cutlery - this requirement is especially important for people living in dormitories and communal apartments. Compliance with hygiene requirements is also extremely important. We are talking about timely washing of hands after contact with other people and objects, as well as maintaining intimate hygiene. For this purpose, you can use the Ginocomfort washing gel. Thanks to its balanced hypoallergenic composition, which includes tea tree oil, chamomile extract and other natural ingredients, this product delicately cleanses the intimate area and has an antimicrobial and moisturizing effect. Sources:
- ROLE OF CYTOMEGALOVIRUSES IN OBSTETRIC PATHOLOGY AND NEONATOLOGY. Smirnova A.I., Rossikhina E.V., Dyupina N.S. // Vyatka Medical Bulletin. – 2010. – P. 1-14.
- CYTOMEGALOVIRUS INFECTION. Lutsenko M. T. // Bulletin of physiology and pathology of breathing. – 2012. – No. 44. – pp. 131-136.
- CLINICAL VARIANTS AND CLASSIFICATION OF CYTOMEGALOVIRUS INFECTION IN YOUNG CHILDREN. Baranova I.P., Kerimova Zh.N., Konnova O.A., Lesina O.N., Nikolskaya M.V., Krasnova L.I. // 2009 – pp. 13-15.
- Human herpesvirus infections: a guide for doctors. Isakov, V.A., Arkhipova E.I., Isakov D.V. // SPb.: SpetsLit. - 2006. - P. 300.
- Viral infections of pregnant women: pathology of the fetus and newborns. Kitsak, V.Ya. // Inf.-met. allowance. Koltsovo. - 2005.- P.59-69.
- Modern therapy of herpesvirus infections: a guide for doctors. Isakov, V.A. // St. Petersburg. - 2004. - P. 168.
- https://www.omicsonline.org/open-access/cytomegalovirus-disease-in-patient-with-hiv-infection-antimi…
- https://www.medicinenet.com/cytomegalovirus_cmv/article.htm
- https://academic.oup.com/jid/article/215/10/1523/3738524