Hemeralopia (night blindness) is a pathology accompanied by impaired visual adaptation in low light conditions (twilight, darkness, artificial darkness). With hemeralopia, vision of objects in the dark deteriorates, spatial orientation is disrupted, as well as the process of light adaptation, visual fields are narrowed, and problems with color perception are identified.
The popular name for the disease is “night blindness” due to the similarity of its symptoms with the visual characteristics of chickens, which are also poorly oriented in the dark or twilight. The retina of our eye is made up of rod-shaped ("rod") and cone-shaped ("cone") light-sensitive cells that make up the photoreceptor apparatus of the eye. At the same time, “rods” provide black-and-white twilight and night vision, “cones” provide daytime perception of the color palette. On average, the retina contains approximately 110–125 million rods and up to 7 million cones, the normal ratio of which is 18:1.
The rod-shaped cells of the retina have the visual pigment rhodopsin, which provides dark adaptation to vision. This pigment tends to disintegrate in the light, and in the dark, reacting with vitamin A, it is restored. The synthesis of rhodopsin pigment occurs with the release of energy, the conversion of which into electrical impulses gives signals to the optic nerve, which sends impulses to the brain. This mechanism is ensured by the normal functioning of rod-shaped cells. Violation of the ratio of “cones” and “rods” with a lack of rhodopsin leads to the development of hemeralopia, when in low light visual acuity decreases, remaining normal in bright light.
Causes of hemeralopia
In ophthalmology, it is customary to distinguish three types of hemeralopia: congenital, symptomatic and essential.
In congenital hemeralopia, the causes of the disease are genetic factors that are hereditary and familial in nature. A similar pathology is characteristic of Usher syndrome, hereditary retinitis pigmentosa and other inherited pathologies.
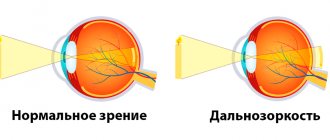
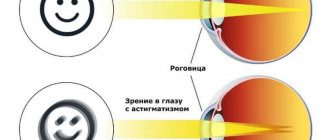
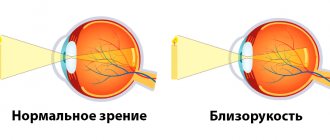
The symptomatic form of hemeralopia occurs against the background of certain eye diseases: high degrees of myopia, glaucoma, retinopathy, cataracts, retinal detachment, chorioretinitis, siderosis, optic nerve atrophy, radiation eye burns, etc.
Essential or, as it is also called, functional hemeralopia is the result of an acute deficiency in the body or a complete absence of vitamins A, B2, PP. A similar condition can occur with liver disease, anemia, exhaustion, diabetes, taking retinol antagonists (quinine), alcoholism, gastrointestinal diseases accompanied by impaired absorption of nutrients (chronic gastritis, colitis, enteritis, etc.).
The trigger mechanism for hemeralopia can be previous infections (rubella, measles, herpes, chickenpox), menopause in women, strict diets (including vegetarianism). Regardless of the form of the disease, deterioration of visual acuity in the dark is due to one factor - a violation of rhodopsin synthesis.
Causes of dangerous pathology
If you discover signs of night blindness, in order to save your vision, you will have to adhere to the basics of comprehensive treatment. Otherwise, the therapy will not give the desired long-term effect.
This is explained by the fact that the human retina consists of two types of cells:
- sticks;
- cones.
The former are responsible for the ability to see in poor lighting conditions, while the responsibilities of the cones include the ability to recognize colors and control overall visual acuity. As soon as even minor deterioration begins in the retinal cells, this immediately affects the rapid deterioration of well-being, because the patient develops night blindness.
Physiologically, the mechanism is explained by the fact that rods are formed from rhodopsin, which is obtained through cooperation with vitamin A. If light hits the retina, then rhodopsin disintegrates. To regenerate the component, a new vitamin dose is required, which the body simply has nowhere to take from. This makes it clear why the deficiency of useful components is so destructive.
If we consider the general primary sources of pathology without taking into account poor heredity and lack of minerals, then there will still be many other variations due to which hemeralopia is observed:
- liver failure;
- anemia;
- exhaustion of the body against the background of weak immunity, which is an ideal environment for the development of many other ailments, including scurvy;
- treatment with vitamin A antagonists.
Various atypical retinal pigment pathologies, retinal detachment, dysfunction of the optic nerve, inflammation, glaucoma, myopia and many other eye diseases can also act as a catalyst for deviation.
In recent years, cases have become more frequent when dangerous signs began to manifest themselves even in healthy people who had no history of night blindness, and a visit to an ophthalmologist did not reveal any specialized eye diseases.
Because of this, many patients begin to panic, asking: what is happening to them? In fact, the reason should be sought in prolonged work at the computer. The clinical picture is aggravated due to poor lighting. With repeated irritation, the nerve endings are damaged, which then signal a problem with the classic symptoms of hemeralopia.
In order not to reach such a deplorable state, experts recommend doing gymnastics, using drops, the name of which will be suggested by the doctor, and also periodically taking a break from the monitor during the working day.
Signs of hemeralopia
Symptoms of congenital hemeralopia develop in early childhood, characterized by persistent vision loss that cannot be cured. Night blindness is accompanied by a decrease in the acuity of twilight and night vision, and a feeling of visual discomfort even in twilight. Patients with hemeralopia note that they cannot distinguish between surrounding objects and lose spatial orientation in low light or when moving from a dark room to a well-lit one. At the same time, in the daytime, as well as with sufficient lighting, visual acuity is usually not impaired.
In addition, with hemeralopia, there may be a feeling of “sandiness” or dryness in the eyes. Children with hemeralopia are afraid of the dark, so they behave restlessly and often cry at dusk. This disease is characterized by a narrowing of visual fields with a decrease in the perception of yellow and blue colors.
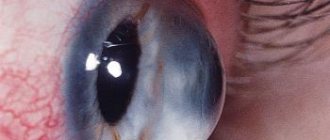
Essential hemeralopia is accompanied by the appearance of xerotic Iskersky-Bitot plaques on the conjunctiva, which are flat dry spots that are located within the eye fissure. In addition to eye symptoms, there may be dryness of the mucous membranes and skin, and areas of hyperkeratosis may appear on the body, with peeling and scratching of the skin, and bleeding gums. With acute vitamin A deficiency, softening and ulceration of the cornea (keratomalacia) is often observed.
Symptoms of night blindness
The first symptom that should cause concern to the patient is the appearance of tangible signs of decreased vision in the dark and irritation from bright light. Another sign of night blindness may be the appearance of spots in the eyes when moving from the dark to a brightly lit area. Often its appearance frightens patients and forces them to urgently seek advice from an ophthalmologist.
With night blindness, there may be a decrease in the ability to correctly distinguish colors, this is especially noticeable when identifying the color blue and its various shades.
Diagnosis of hemeralopia
Deterioration of twilight vision is a reason for an urgent consultation with an ophthalmologist, who will help identify the causes of hemeralopia. Typically, the examination begins with visometry - checking visual acuity, which in the case of essential hemeralopia is often unchanged. Performing achromatic as well as color perimetry makes it possible to detect a concentric narrowing of the visual fields and the presence of the Purkinje phenomenon.
The ophthalmoscopy picture for various types of hemeralopia has some of its own characteristics. Thus, the essential form of hemeralopia is characterized by the absence of changes in the fundus, while in others there are specific changes inherent to the disease that caused night blindness. With genetically determined hemeralopia, ophthalmoscopy reveals small round foci of degeneration on the retina.
The study of dark adaptation requires adaptometry. The functional state of the retina is assessed using electroretinography and other additional electrophysiological studies. Determining the causes of symptomatic hemeralopia may require tonography, refractometry, as well as biomicroscopy using a Goldmann lens, optical coherence tomography, etc. A comprehensive examination of patients with hemeralopia often includes consultations with a gastroenterologist and endocrinologist.
Treatment of hemeralopia
With the congenital form of hemeralopia associated with hereditary pathology, treatment is not carried out; it is incurable. To treat acquired hemeralopia, it is necessary to identify and subsequently eliminate the causes that caused the violation of dark adaptation.
Hemeralopia caused by myopia requires the selection of glasses or contact lenses; laser correction of myopia or refractive surgery (lens replacement, scleroplasty, etc.) may be offered. Hemeralopia caused by cataracts or glaucoma also requires surgical treatment of these diseases (anti-glaucomatous operations, cataract surgery). If the cause is retinal detachment, laser coagulation is indicated.
In case of essential hemeralopia, first of all, it is necessary to normalize the diet, enriching it with foods containing carotene and retinol (butter, cheese, cod liver, milk, eggs, carrots, tomatoes, spinach). In addition, instillation of vitamin drops for the eyes and oral forms of vitamin A, riboflavin, and nicotinic acid are prescribed, according to age-specific dosages. At the same time, treatment of gastrointestinal diseases and diabetes mellitus is mandatory (with monitoring of blood glucose levels and insulin therapy).
Treatment of decreased visual acuity at dusk, “night blindness”
If the cause of night blindness is a disease, then treatment is aimed at eliminating it. However, congenital night blindness cannot be treated.
For people who suffer from night blindness, doctors recommend the following:
- Taking vitamin A - the dose should be calculated by an ophthalmologist because vitamin A is toxic in large quantities;
- Periodically examine peripheral vision;
- To absorb vitamin A, it is recommended to adjust your diet and enrich it with fatty acids.
Prevention of hemeralopia
Symptomatic hemeralopia, depending on the severity of the underlying disease during treatment, can lead to both the restoration of dark adaptation of vision and its permanent loss. Functional hemeralopia usually responds well to therapy with complete restoration of twilight vision.
However, patients suffering from hemeralopia often develop a pathological fear of the dark, which takes on the nature of a phobia or obsessive-compulsive disorder, which is a mental disorder.
To prevent hemeralopia, it is necessary to ensure that the body receives the necessary vitamins, as well as adequate protection of the retina. To achieve this, treatment of concomitant pathologies, adequate nutrition, and the use of sunglasses must be provided, both outdoors and when working with harmful radiation. People with hemeralopia are not recommended to use fluorescent lamps. Children with mild myopia need to wear glasses in the evening.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic is open seven days a week and operates daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can make an appointment at the Moscow Eye Clinic by calling 8 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the online registration form.
Folk remedies
Photo: organicauthority.com
Folk recipes for combating night blindness also suggest diversifying your diet with fresh fruits, berries, vegetables, especially green ones - green onions, celery, spinach, parsley. A salad of grated carrots with vegetable oil, millet porridge, quickly cooked liver, cream, egg yolk, fresh blueberries and currants will be very useful.
A remedy that has long been popular is fish oil. Fish oil has been used to prevent rickets because it is high in vitamin D, but it also contains large amounts of fat-soluble vitamin A. To combat night blindness, it is enough to take one tablespoon for 3-4 weeks.
Decoctions and infusions that are used for night blindness.
- Infusion of red rose. Place a teaspoon of dried rose petals in a glass of water, pour boiling water over it, leave until it cools. Take three glasses a day.
- For a decoction, take dandelion leaves and roots, blueberry grass, linden flowers, a tablespoon each, buckwheat and sea buckthorn leaves, half a tablespoon each, boil in 1 liter of water for 15 minutes, let it brew for 30-40 minutes and take one glass a day, pre-strained.
- Young shoots of stinging nettle, two tablespoons, are infused in boiling water for one hour and drunk a third of a glass during the day before meals.
- An infusion of eyebright herb is prepared in the evening by pouring cold boiled water and leaving to infuse overnight (8-9 hours). In the morning, strain and take a quarter glass three to four times a day.
Decoction of rose hips. Give three tablespoons for two glasses of water and boil for 10 minutes. Take two glasses a day.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.