Today, complications often occur during pregnancy and childbirth. Premature placental abruption is very dangerous for the baby and the mother. This complication occurs, according to statistics, in 0.3 – 1.5 cases out of 100. Most cases are recorded in the first trimester. But basically everything ends well if such a complication appears in the early stages of pregnancy.
- Functions of the placenta
- What is placental abruption?
- Causes of detachment
- Classification
- Symptoms
- Severity of the problem
- Treatment
Functions of the placenta
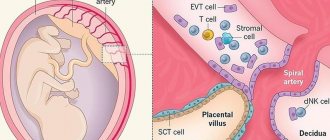
The placenta is considered a temporary organ. Its formation begins only when the egg fertilized by sperm is implanted into the uterus (on the 10-13th day after conception). The end of organ formation occurs at the 16-18th week, when the embryo begins to feed hematotrophically (in the early stages this is histotrophic nutrition). At this stage, the hematoplacental barrier is formed, and the placenta can already fully realize its function.
The placenta is also known by the popular name "baby place" or placenta. During labor, contractions begin, after which the placenta separates. This organ connects the body of the mother and the embryo for 9 months. Functions of the child seat:
- gas exchange
The fetus cannot breathe on its own; in the early stages, even its lungs are not fully developed. Therefore, oxygen enters the baby’s body from his mother’s body. Gas exchange occurs in the small body and carbon dioxide is released. And this gas enters the blood of the expectant mother. This is how the fetus breathes.
- nutrition
Between the villi of the placenta and the wall of the uterus lies the intervillous space. Maternal blood enters there with all the nutrients that are in the woman’s body. And the fetus thus “eats” through the placenta.
- excretory
As the baby develops, metabolites are formed. These are creatine, creatinine, urea. The placenta removes them.
- hormonal
Since the endocrine gland is not developed in the baby’s body, the placenta “steers the process” instead. It produces hormones, which are important for the formation of the fetus. Surely you have heard that there is such a pregnancy hormone as human chorionic gonadotropin. It stimulates the functioning of the placenta and causes the corpus luteum to produce progesterone.
During the gestational period, the mammary glands develop, among other things, under the influence of lactogen produced by the placenta. It is needed to ensure that milk is released in a timely manner and in sufficient quantities during lactation. Lactation also depends on prolactin. Estrogens and progesterone stimulate the growth of the mucous layer of the uterus and prevent new maturation of the egg from taking place while the baby is still developing in the stomach. The placenta also produces relaxin and serotonin, etc.
- protective
The placenta allows antibodies from the mother's body to enter the fetus's body. Therefore, the baby develops immunity to many diseases (which his mother had previously suffered from). The placenta also prevents conflict between the body of the embryo and the woman who bears it. But remember that the medications you take during pregnancy will reach the fetus. The same applies to nicotine, ethyl alcohol and narcotic substances. Viruses also pass through the placenta to the fetus.
Treatment of APS
Causes and consequences of placental abruption in early pregnancy
To prevent undesirable pregnancy outcomes with a confirmed diagnosis of APS, treatment should begin at the stage of preparation for childbirth. What is the therapy:
- Adrenocortical hormones are prescribed in small doses (Prednisolone 5 mg).
- In the 1st trimester, at 24 weeks and before birth, antiviral immunoglobulin is administered.
- During pregnancy, antiplatelet therapy is carried out with Curantil, Trental, Teonicol.
- In some cases, the use of Heparin in small doses is indicated.
- Before pregnancy and during it, plasmapheresis is indicated.
- Since the majority of pregnant women with APS have corpus luteum deficiency, prescribing Duphaston to such women is justified.
In the postpartum period, corticosteroid therapy (Prednisolone) started before conception and antiplatelet therapy under the control of blood coagulation continue. Mothers with this diagnosis are not allowed to breastfeed - they are given medication to suppress lactation.
In complex therapy, the prescription of antispasmodics and sedatives is indicated. The drug Magne B6 has proven itself well. The magnesium contained in it has a tocolytic effect, that is:
- Normalizes increased uterine tone.
- Reduces high blood pressure.
- Relieves anxiety, normalizes sleep, and has an anticoagulant effect.
You should remember the need for anti-anemic therapy with iron supplements.
What is placental abruption?
The placenta is normally located at the bottom of the uterus, moving to the posterior (less often, to the anterior) wall of the organ. The essence of abruption is that the baby's place is separated from the walls of the uterus even before childbirth occurs (during pregnancy or too early in the birth process). The muscles of the uterus press on the placenta from the outside, and amniotic fluid presses on it from the inside. Since the baby's place has a spongy structure, it is elastic (can stretch), so it does not peel off during gestation.
The area of the uterus where the placenta is attached may contract less than other areas of the organ. It also prevents placental abruption in normal pregnancies.
Norm of IAF by week
| Duration in weeks | Lower threshold | Upper threshold |
| 16 | 73 | 201 |
| 20 | 86 | 230 |
| 26 | 89 | 240 |
| 30 | 82 | 258 |
| 34 | 72 | 278 |
| 36 | 68 | 279 |
| 40 | 116 | 240 |
Oligohydramnios also adversely affects the development of the baby. The problem is especially dangerous in the 2nd and 3rd semesters of pregnancy. This pathology is detected by ultrasound using the same method as polyhydramnios.
Causes of detachment
The exact reasons are not known today. Basically, there are several factors that provoke complications:
- mechanical factor
- bleeding disorder
- vasculopathy
Causes:
- many births with little time between them, which causes endometrial degeneration)
- post-term pregnancy
- compression of the inferior vena cava, which changes blood pressure
- sudden surges in blood pressure due to stress and other reasons
- high blood pressure as a consequence of vascular diseases
- endocrine disorders, mainly diabetes mellitus
- age (from 30 years of age the risk is higher)
- hereditary bleeding disorders
- autoimmune diseases, such as SLE
- tearing off an additional piece of placenta during pushing
- gestosis
- premature “aging” of a child’s seat
- congenital malformations of the uterus
- operations or cesarean section, as a result of which scar tissue has formed that does not “hold” the placenta well
- infectious-allergic vasculitis
- blunt abdominal trauma
- taking drugs, drinking alcohol, smoking and other habits harmful to the organisms of mother and child
- incorrect location of the placenta (too low attachment or presentation)
- blood transfusion or infusion of colloidal solutions, which leads to vascular-allergic reactions that cause placental abruption
Causes of detachment during childbirth:
- rapid or rapid labor
- the birth of the first fetus when carrying several children (the baby “pulls” the placenta behind him
- rapid decrease in pressure inside the uterus as water flows out
- anomalies of ancestral forces
- delayed opening of the amniotic sac
- short umbilical cord length
- oxytocin for labor stimulation
- obstetric manipulations to help the baby be born
Consequences for mother and baby
The pathology is fraught with the most serious consequences for a woman and her unborn child.
complications. According to medical statistics, every tenth pregnancy with this pathology ends in death.
Death can occur as a result of massive blood loss and loss of uterine contractility in the postpartum period, as well as due to blockage of blood vessels.
Also, placental abruption poses a threat to the life of the child, especially in the period before the onset of labor. With a large area of detachment, the fetus may die due to an insufficient amount of oxygen entering the blood, resulting in severe hypoxia, incompatible with life.
Even if the baby is born, the effects of oxygen deprivation during the fetal period can affect its mental and physical development. A frequent complication in children born with placental abruption is pathology of the cardiovascular and other vital systems.
Symptoms
Typical symptoms give doctors the opportunity to recognize placental abruption, even without testing other than examination. In the first trimester, as already noted, there is a greater chance of a successful pregnancy outcome. Placental abruption in the first trimester indicates that there is a threat of miscarriage. The signs are:
- stretching or aching pain in the lower abdomen, radiating to the lower back
- moderate or slight bleeding
- low basal temperature
If the mother goes to the doctor immediately when alarming symptoms appear, the complication will be stopped, and the pregnancy can be carried to a normal term. The placenta will gradually grow, and the area that has lagged behind the uterus will no longer play a big role in the development of the fetus and the well-being of the expectant mother.
Ultrasound examination reveals placental detachment in the first trimester as a retrochorial hematoma. She's not growing. But ultrasound does not always detect this hematoma. Doctors and the mother can find out about the diagnosis after birth, when they see a blood clot or a hole in the child’s place that has a gray-burgundy tint.
In the 2nd and 3rd trimester, the consequences of the complication in question may be more serious. Possible bleeding from the uterus. It is caused by a violation of the integrity of the vessels that grow from the uterus to the placenta. As a result, blood begins to accumulate in the uterus and placenta, so exfoliation continues. A bruise forms inside, that is, a hematoma. It puts pressure on the placenta, so its function (described in detail above) is disrupted.
If in the middle and towards the end of gestation a placental abruption occurs in a pregnant woman, then the woman may have more or less intense discharge. How much of this will depend on the location of the detachment, the extent of the pathology and how normal the patient’s blood coagulation system is. When placental abruption occurs, there are 3 types of bleeding:
- visible
- external
- internal mixed
In 4 out of 5 cases of abruption, blood comes out. But this does not mean that part of it does not collect inside and form a hematoma that threatens the fetus. Basically, external bleeding occurs if the placenta is detached from the edge. Then the blood enters the vagina and out. If the hematoma is located at the bottom of the uterus, then blood will not exit through the genitals. The discharge will be dark.
If blood collects inside, the doctor diagnoses internal bleeding. This happens with central detachment of the placenta. Along the edges, the adhesion of the uterus and placenta is normal. A hematoma can grow in hours and even minutes, which provokes an increasingly large scale of detachment. The wall of the uterus collects blood and therefore contracts worse than it should. This is called "Cuveler's uterus". If the bleeding is not stopped in time, the woman’s condition will get worse as she loses blood. In some cases, hemorrhagic shock and blood clotting disorders (DIC) develop.
Placental abruption also causes pain. It is characterized as constant, bursting or dull. Pain can be felt in different areas, depending on where the placenta is located. If the placenta is attached mainly to the posterior wall of the uterus, then pain will be felt in the lumbar region. If the placenta is attached to the front wall, then it will hurt in front - the stomach. In some cases, the doctor palpates a tense and painful swelling.
There is not only pain, but also hypertonicity of the uterus, because the hematoma inside causes uterine irritation. And uterine contractions occur. The pain syndrome is caused by the pressure of the hematoma on the walls of the uterus, their excessive stretching, as well as the fact that they absorb blood, as well as irritation of the peritoneum.
Intrauterine fetal hypoxia is another manifestation of such a complication during pregnancy as placental abruption. The child's heart activity is impaired. The embryo does not receive the required amount of oxygen, resulting in bradycardia or tachycardia. If the placenta is severely detached, then for the child this is even worse than detachment of a small area.
Treatment
Why is low placental attachment dangerous during pregnancy?
Patient management tactics depend on:
- gestational age,
- degree of separation,
- volume of blood loss
- functional state of the mother and fetus.
In this case, the following drugs are prescribed:
- reducing tone;
- antispasmodics (for example, no-spa);
- hemostatic drugs (aminocaproic acid, etamsylate);
- in case of massive blood loss - iron supplements, folic acid to prevent anemia;
- in case of decompensation of chronic pathology - adjustment of doses of drugs received previously, or selection of new ones and replacement with more effective ones.
If the woman’s general condition worsens during therapy, or if bloody discharge reappears after the bleeding stops, attempts to save the child should be abandoned.
It is necessary to proceed to surgical treatment, as this indicates the progression of exfoliation and a threat to both lives.
Depending on the duration of pregnancy and the functional state of the organisms of the mother and fetus, various surgical solutions are possible.
- The most common method when fetal viability is likely is cesarean section under spinal or epidural anesthesia. After short preoperative preparation, a puncture of the subdural or subarachnoid space is performed. Injection of a local anesthetic solution. After the onset of pain relief, a layer-by-layer dissection of the soft tissues in the lower abdomen is performed and the child is removed. The wound is sutured layer by layer with a cosmetic skin suture. During this intervention, the presence of, in addition to the team of anesthesiologists and obstetricians, neonatologists is required for the early start of intensive care of the child;
- It is possible to manage delivery through the natural birth canal. But only if the mother’s condition is stable and the baby has no abnormalities. After birth, a manual examination of the uterine cavity is performed. This will help eliminate incomplete separation of the placenta or the preservation of an additional lobe;
- in the early stages, therapeutic curettage or abortion is performed under total intravenous or inhalation anesthesia.
The main and most severe complication is Kuveler's uterus. It represents imbibition of the uterine wall with blood leaking from ruptured capillaries.
In this case, before the operation, the pregnant woman signs consent to remove the uterus. A blood-soaked wall can become a source of blood clots and infection.
Pathology can initiate disseminated intravascular coagulation with subsequent heavy internal bleeding.
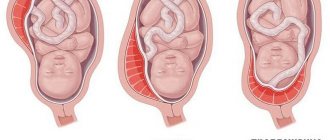
Severity of the problem
The complication in question can be of three degrees of severity:
- light
Such a detachment is discovered mainly after childbirth. Pathology can also be detected during gestation by ultrasound. At the same time, the woman feels normal, and the condition of the fetus is also normal. The symptoms described above simply do not exist.
- medium-heavy
This means that the baby's place is behind the uterus by 1/3-1/4 of the total area. In this case, a small amount of blood is released from the vagina. The doctor detects uterine hypertonicity and fetal bradycardia. In this case, the patient may have a stomach ache. Manifestations of hemorrhagic shock gradually intensify.
- heavy
Abdominal pain is characterized as bursting and severe. In this case, the pain appears suddenly, along with dizziness and severe weakness. Some women faint. There may be little or moderate bleeding from the genitals. The doctor notes that the uterus is asymmetrical, dense, and sharp pain occurs on palpation.
The placenta with this form has separated by ½ or more. This is a huge threat to the unborn child. It is urgent to take medical action so that the child does not die in the mother’s belly. There is a rapid increase in the manifestations of DIC syndrome, the patient feels worse and worse and may die.
Diagnostic methods
The clinical manifestations of the pathology are so typical that additional studies, as a rule, are not needed.
Diagnosis is based on the presence of bloody discharge, the presence of pain, changes in the shape of the uterus and increased tone of the organ.
Hardware methods include fetal heart rate measurement and ultrasound.
With a small area of change, ultrasound examination may not show detachment. But in any case, there will be a noticeable accumulation of blood behind the placenta.
It is also recommended to perform a vaginal examination, since bleeding is not necessarily caused by placental abruption. It is often caused by cervical erosion, infections or benign tumors.
Breech presentation of the fetus on ultrasound
Fetal presentation is not exactly the same as position. Position is understood as the placement of the fetus relative to a vertical axis running along the uterus, and presentation is what part of the baby’s body is rotated relative to the cervical canal. Until the 33rd week, the fetus changes its position every day, but then it experiences intense weight gain, and the position adopted until the 34th week does not change until birth. Normally, the baby turns his head down, but sometimes he fixes his body down with his legs or buttocks. This pathological position is called breech presentation of the fetus.
The contours of the baby can be seen very clearly on ultrasound. Ultrasound diagnostics is the only way to accurately visualize the baby’s position. The method helps to avoid complications during childbirth. As a rule, presentation is accompanied by polyhydramnios, and the fetus has the opportunity to behave more freely. If the baby does not change its position before the 36th week, the woman is prescribed a cesarean section.
Fetal hypoxia on ultrasound
The ultrasound diagnostic method perfectly detects fetal hypoxia. Hypoxia refers to a violation of the oxygen supply to the fetus, which occurs at any stage and poses a threat to the baby’s health.
Using ultrasound, they monitor the intensity of the baby's movement, heartbeat and blood flow of the umbilical cord flagellum. The Doppler method is the most informative. It allows you to identify the frequency of reflection of the ultrasound signal from the blood flow in the umbilical cord and blood vessels. Hemodynamic impairment (blood does not move from an area of high pressure to an area of low pressure) is the main sign of fetal hypoxia.
Causes of pathology:
- placental abruption
- umbilical cord entanglement
- compression of the cord
- high or low water
- Rhesus conflict
- congenital malformations of the fetus
- mother's stress
- infections.
Oxygen starvation is a very dangerous pathology that leads to the following:
- the walls of the placenta become too thin or thick
- the child moves less
- premature aging of the placenta
- developmental delay of the fetus in terms of weight and height
- brain damage in a child