Red moles (angiomas) are vascular neoplasms, the diameter of which ranges from several millimeters to several centimeters. Most often, angiomas appear during fetal development (congenital angiomas), but they can also occur after birth.
Small red moles can be localized on the stomach, arms, legs, back, chest, face, neck, and also on internal organs. Depending on the shape, there are three types of red moles: dotted, cavernous and stellate.
Causes of red moles
The exact reason why red moles appear on the body is unknown; it may be a predisposition due to a genetic factor. But there are other reasons:
- pregnancy;
- exposure to chemicals;
- some diseases, including infectious ones;
- unsuitable climate (too hot or cold)
- mechanical damage to the skin, such as a bite or cuts, in which pieces of skin are not completely torn off.
Their manifestations are also possible at a more mature age, this is due to a gradual decrease in immunity. Neoplasms occur in 75% of the population over the age of 60 years.
It is impossible to somehow influence the appearance or non-appearance of red moles on the body, since they are inherent in us at the genetic level; if one of the parents had a lot of them, it means that the children will have a similar situation, and even identical maps of the location of nevi are possible.
Prevention of angiomas
After establishing the true cause of the appearance of red moles, it is important to avoid provoking factors. As a preventative measure, experts recommend:
- drink at least 1.5 liters of water per day;
- eat more fresh fruits and vegetables rich in fiber;
- add olive oil to your diet;
- try to spend less time under the scorching sun;
- sunbathe only in the morning or evening (using sunscreen);
- stick to a balanced diet.
Locations
An increase in the growth of moles is observed in people aged 0 to 20 years, and then from 45 years and older. The rest of the time they appear, but not as actively as in the first and last phases of life. Typically, red moles appear on the upper body, arms, legs and shoulders. Their favorite places are also the head, feet, and hands. They can be located throughout the body, and it is impossible to predict their subsequent locations. Their red color comes from the accumulation of small blood vessels at the base, which supply them with blood.
Treatment methods
Treatment methods for angioma are selected after examination. If the formation is flat, it is easier to remove than a convex one. No major pain relief is required before the removal procedure. A local anesthetic may be used. After the procedure, the affected area may bleed slightly.
After completion of the procedure, a rehabilitation period is recommended, during which exposure to sunlight on the affected area is limited.
There are many ways to remove angioma.
- Application of X-rays
. They help identify and reduce the mole. If it is small, it can be completely eliminated after a course of therapy. At the moment, the method is rarely used due to the risk of malignant degeneration. - Surgical removal
. After the procedure, the mole is completely gone. A connective tissue scar may appear in its place. Therefore, the method is used for localization in invisible areas. After the procedure, rehabilitation methods are used. For example, antibacterial powders or ointments, a ban on swimming for 1-2 days. - Cauterization with carbon dioxide
. The technique is applicable for small formations located on the upper layers of the epidermis. Therapy for large moles is not carried out using this method, since its lower layers may remain intact, so it will form again. - Chemical sclerosis
. Suitable for capillary type moles. A substance is injected subcutaneously that eliminates the effect of blood vessels. The mole stops receiving blood and gradually disappears. - Cryodestruction
. The mole is cauterized with liquid nitrogen. Due to the low temperature, the walls of the capillaries are destroyed, and a crust gradually forms. Healthy tissue will form in its place. The technique is applicable when angioma penetrates to the deep layers of the epidermis. - Coagulation
. With its help, large and small formations are removed. There are no scars left after the procedure. We will use infrared, radio wave, and light methods.
Removal is recommended if the aesthetic appearance is compromised and there is a risk of malignant degeneration.
Types and classification
Moles have two main types:
- Pigmented. These include flat, often brown, nevi.
- Vascular, which are formed from changes in the structure of blood vessels.
They are also:
- Congenital - divided by size: small, medium and large.
- Acquired, divided into three types depending on the location of melanocytes in the layers of the epidermis.
- Hanging ones, they are also called papillomas.
There are invisible nevi that appear changing color over time. Also wandering, which change their location, appearing in one place or another. It is advisable to keep track of the location of your moles.
PRECAUTIONARY MEASURES
People with red moles should not have special restrictions. These formations do not require special care or specific treatment.
But some recommendations from experts should still be followed. As mentioned above, the only thing that can be dangerous is mechanical impact, hence the possibility of damage.
Specialists at LIC clinics recommend removing angiomas in places where there is a risk of injury. Also, avoid excessive sunbathing near water, as water increases exposure to ultraviolet rays. But if it so happens that you cannot avoid them at all, then you should use protective creams with a filter of at least SPF 30.
Are red moles dangerous?
Signs to pay attention to if small red moles appear:
- Color. If it is uneven and begins to change, this is a reason to visit a doctor.
- Inflammation around the formation, that is, redness in the form of a halo around the mole.
- An increase in the size of the mole or its thickening.
- The appearance of cracks and ulcers on the body of the mole.
- Hair loss if it grew from a mole.
- The appearance of itching, burning or tingling in the place where the mole is located.
- A change in the edges of the nevus also indicates that it is time to visit a specialist.
An accurate diagnosis can be made by a dermatologist or oncologist, and you can and should turn to them for help. Nevi are not dangerous as long as they are in a stable condition, in which case you can wait to see a doctor.
Spontaneous problem resolution
Red moles go away on their own if they are superficial or simple. This is possible in no more than 15% of cases. Most often, formations that are localized on closed parts of the body regress.
At first, the tumor becomes less bright and decreases in size. After six months, the mole becomes a pale pink spot located at skin level. In this case, the skin over it atrophies. After another 3-4 years, only a small depigmented area remains on the skin.
Red moles in children
For most people, the bulk of moles appear in the first 20 years of life, then the formation of moles (nevi) subsides. They also tend to sometimes disappear on their own, and this happens due to the fact that the blood vessels supplying the mole dry out or become clogged. One in 100 newborns are already born with small red moles on their body, and they are considered more prone to change and develop into melanoma. This red neoplasm that rises slightly above the surface of the skin is called a Spitz nevus.
Children can also be born with large blue spots on their backs; they are called Mongolian spots and are most often found in children with Asian roots. Any moles are often injured, especially in childhood. This can cause complications, so it is advisable to sometimes see a doctor, and also try to protect children from such injuries.
Types of hemangiomas
There are 2 types of hemangiomas - congenital - formed during intrauterine development - and acquired;
acquired in early childhood are often called infantile. By structure, single and multiple hemangiomas (hemangiomatosis) are distinguished; by structure - capillary, arterial and venous. By education they are local and segmental. Local hemangiomas grow from one point, are distinguished by smooth edges and relatively small sizes. Segmental - large, with a “ragged” edge, often develop as part of combined pathologies of the chest, aorta, pelvis and sacrum, heart defects, etc.
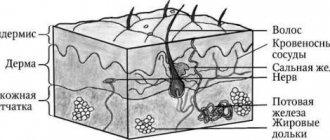
Hemangiomas are classified according to their location:
- simple – formed on the surface of the skin;
- cavernous - grows under the skin;
- combined - the process involves the superficial and deep layers of the dermis;
- mixed - not only dermal, but also nervous and muscle tissues are involved in the process.
Do red moles need to be removed?
Not only is it possible, but it is also necessary. If the hemangioma increases in size, changes shape or color, this is, of course, a direct indication to see an oncologist as soon as possible for further examination, and removal if necessary. Of course, not using artisanal or folk methods, but with the help of modern specialists. If the mole behaves quite calmly and does not change shape or color, then most likely there is no need to be afraid and you can postpone removing the moles.
When is treatment required?
Most often, angiomas do not cause discomfort or threaten health, so dermatologists do not recommend treating them. Surgical removal is indicated only in the following cases:
- visual defect, for example, when a large formation is located on the face;
- frequent mechanical damage due to inconvenient location (in the shaving area, bra wire);
- change in shade;
- increase in size;
- discomfort at rest or when pressed.
With negative symptoms, contact a dermatologist. A general examination is not enough. It may be necessary to conduct laboratory and instrumental tests to determine the degree of malignancy and the cause of negative signs.
Self-treatment and removal of moles at home is strictly prohibited. This can lead to complications. For example, bleeding, malignant degeneration, increase in size.
The only treatment method is surgery. The use of gels, ointments and other conservative remedies does not help. They can only improve the condition of the skin (moisturize, eliminate inflammation, prevent the effects of ultraviolet rays).
Diagnostics
In medicine, there is a general method for diagnosing skin tumors. These include an initial examination and recording of all patient complaints (history). If a malignant tumor is suspected, an MRI or radiography is prescribed. All data obtained is analyzed and conclusions are drawn, on the basis of which a preliminary diagnosis is made. The main and final point in making a diagnosis is the histological method (biopsy). It is a microscopic sampling of tissue from the body of a mole, and is done to identify the pathology of cells in the neoplasm.
How are hemangiomas treated?
The main method of treatment is surgical. In addition to cosmetic reasons, there are medical indications for this:
- rapid growth and threat of malignancy of the tumor;
- disruption of the normal functioning of organs - for example, if there is a tumor on the eyelid or tongue;
- impaired blood circulation – if the tumor is on a large vessel;
- infection and bleeding – for example, when on the genitals.
The priority is gentle, minimally invasive methods for removing hemangioma or vascular surgery methods to reduce blood flow in it. The excised tissue is sent for histological analysis.
If the neoplasm is small, it is possible to use electrocoagulation, radio wave or laser surgery, or cryodestruction with liquid nitrogen. For some forms of hemangiomas, sclerotherapy is effective - “gluing” damaged capillaries by injecting special solutions Source: Hemangiomas and vascular malformations. Modern theories and therapeutic tactics. Goncharova Y.A.: Child’s health, 2013.
For slow-growing tumors with a low risk of malignancy, conservative drug therapy with drugs from the group of beta-adrenergic receptor blockers is possible Source: Wong A., Hardy K., Kitajewsky A. Propranolol causes functional changes in hemangioma stem cells and hemangioma endothelial cells // Abstract book. ISSVA the 19th International Workshop on Vascular Anomalies. — 2012. – p. 245.. In some cases (if the tumor does not grow, does not bother, or there is a tendency towards its reverse development), they resort to wait-and-see tactics.
To ensure the effectiveness of treatment, after its completion, a control study is prescribed - ultrasound, tomography or dermatoscopy. To consult with a specialized specialist in St. Petersburg, fill out the online form.
Sources:
- What a pediatrician needs to know about infantile hemangiomas. Zakharova I.N., Kotlukova N.P., Roginsky V.V., Sokolov Yu.Yu., Zaitseva O.V., Maykova I.D., Idrisova G.R., Pshenichnikov I.I.: Medical Council , 2016
- Infantile hemangioma: classification, clinical picture and methods of correction. Sheptiy O.V., Kruglova L.S.: Russian Journal of Skin and Venereal Diseases, 2021.
- Hemangiomas and vascular malformations. Modern theories and therapeutic tactics. Goncharova Y.A.: Child’s health, 2013.
- Sires V. Systemic corticosteroid use in orbital lymphangioma /V. Sires, C. Goins, R. Anderson // Ophthal. Plast.Reconstr.Surg. — 2001. Mar. - Vol. 17(2). — P. 85 — 90.
- Wong A., Hardy K., Kitajewsky A. Propranolol causes functional changes in hemangioma stem cells and hemangioma endothelial cells // Abstract book. ISSVA the 19th International Workshop on Vascular Anomalies. — 2012. – p. 245.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Methods for removing red moles
If the mole does not bother you in any way and is not located in high-risk areas, that is, on the arms, feet, or head and back, then it is quite possible not to remove it.
If the hemangioma bothers you, then it can only be removed by specialists, a dermatologist or oncologist. You should not take the risk of removing a nevus from a cosmetologist and exposing the incorrectly removed hemangioma to the risk of growth or the risk of infection.
There are several common procedures for removing them.
- Electrocautery. The nevus is burned with an electric current delivered using a small instrument. The grounding block will be placed somewhere so that the rest of the body is not exposed to electricity.
- Cryosurgery. The mole is frozen using liquid nitrogen. It is destroyed by extreme cold. Liquid nitrogen is sprayed for 10 seconds, the problem is solved in one session. This method is quick and relatively simple. The wound also does not require special care.
- Laser surgery. This procedure uses a concentrated yellow laser beam that emits enough heat to destroy the nevus from the inside. This method is quick and is used on an outpatient basis, meaning it does not require subsequent hospitalization. Depending on how many moles will be removed, one to three procedures may be required. There may be small scars that will disappear within 10 days.
- Surgical method. This is the process of removing a nevus from the upper part of the skin by cutting the lesion and then applying sutures. It is not a frequently used method, and after such an intervention there are scars.
In any case, if you have concerns and questions about why red moles appear, you need to see a doctor, if only to reassure yourself with good tests. Because unexplained questions create stress, which in turn contributes to a decrease in immunity. Be healthy.
Features and advantages of laser technology
Many people prefer to remove moles using a laser. This technique has a number of advantages, including:
- high performance. It is possible to completely get rid of angioma in one procedure;
- comfort. Laser removal is carried out using modern anesthetic substances, so the patient does not experience any discomfort;
- availability. The prices for the technique are low;
- short duration. It takes no more than 20 minutes. The exact time depends on the size and number of moles;
- lack of long-term rehabilitation;
- safety (no bleeding or risk of infection).
Contraindications to the technique are minimal. It cannot be performed in the presence of infectious diseases, diseases of the cardiovascular system, lesions of the central nervous system, which are characterized by increased excitability. The doctor will tell you more about the possibility of using this technology after the examination.